Abstract
Background
Preoperative esophagogastroduodenoscopy (EGD) in patients undergoing bariatric surgery can help surgeons detect abnormalities in the upper gastrointestinal (UGI) tract that may require a change in surgical plan. However, the need for EGD before bariatric surgery is controversial.
Objectives
We aimed to determine the prevalence of UGI abnormalities and evaluate the predictive factors of abnormal findings that require a change in surgical plan or cause a delay in surgical treatment in patients undergoing bariatric surgery and develop a prediction model.
Methods
The medical records from January 2012 to July 2020 were retrospectively reviewed in patients who underwent EGD before bariatric surgery. The EGD findings were classified into four groups based on their effects on management. Group 1 had normal findings. Group 2 had abnormal findings that did not require a change in surgical management. Group 3 had abnormal findings that required a change in the surgical plan or caused a delay in surgical treatment. Group 4 had contraindications to surgery. Predictive factors for Groups 3 and 4 were analyzed using univariate and multivariate analyses. A model visualized as a nomogram was developed based on significant factors. Discrimination and calibration were evaluated.
Results
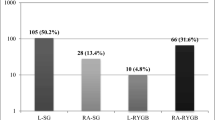
A total of 461 patient records (63.8% female) were reviewed. The mean age was 35.1 ± 11.2 years and the mean BMI was 47.7 ± 8.7 kg/m2. The prevalence of endoscopic findings in Groups 1, 2, 3, and 4 were 42.5%, 35.6%, 21.9%, and 0%, respectively. The most common abnormal findings were non-erosive gastritis (31.2%) followed by Helicobacter pylori infection (18.7%) and hiatal hernia (10.2%). Male sex and NSAID use were significantly associated with detection of lesions in Group 3 either on univariate or multivariate analysis, while type 2 diabetes mellitus (T2DM) was a significant protective factor on multivariate analysis. On subgroup analysis in patients ≥ 40 years old, multivariate analysis revealed age, BMI, and NSAID use were significantly associated with the detection of lesions in Group 3, while T2DM was still a significant protective factor. A nomogram to predict lesions in Group 3 for this subgroup was developed and showed good discrimination (C-statistics 0.737, 95% CI 0.721‒0.752).
Conclusion
A high prevalence of abnormal endoscopic findings was observed in Thai patients who are undergoing bariatric surgery. Preoperative EGD screening is helpful in detecting UGI abnormalities that require a change in the surgical decision plan. The new nomogram may help rational utilization of EGD prior to bariatric surgery.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is one of the biggest global health issues and it is recognized as a global epidemic. It is related to several diseases, such as diabetes, cardiovascular disease, gastroesophageal reflux disease (GERD), and various types of cancer [1]. Bariatric surgery is an option for the treatment of obesity that can result in effective short- and long-term weight maintenance [2]. The preoperative evaluation includes an assessment by a multidisciplinary team [3]. Esophagogastroduodenoscopy (EGD) is a preoperative evaluation that helps visualize the abnormalities in the upper gastrointestinal (UGI) tract. It also helps to diagnose diseases that should be treated before surgery, such as erosive esophagitis and peptic ulcer disease. Other findings may include hiatal hernia, mass lesion, or diverticulum that may affect the choice of surgical procedure [4]. An agreement has not been reached as to whether or not all patients should undergo an EGD before bariatric surgery. Some centers always perform an EGD in all patients but some do it selectively [5]. Several studies showed prevalences of abnormal findings that ranged from 51.0 to 89.5% [6,7,8,9,10,11]. However, to date no study has been done in the Thai population. Our hypothesis is that the prevalence of abnormalities in preoperative EGD findings in our patients who plan for bariatric surgery might be similar to the Asian race but different than the Caucasian race due to the higher incidences of Barrett’s esophagus and adenocarcinoma in the Caucasian race [12].
The aim of this study was to determine the prevalence of abnormalities found in preoperative EGD findings in patients who plan for bariatric surgery. We also aimed to evaluate the predictive factors of the abnormal findings that require a change in the surgical plan/approach or cause a delay in surgical treatment or if there are contraindications to bariatric surgery and develop a prediction model.
Materials and methods
Ethical approval for this study was obtained from the Human Research Ethics Committee at our institute. This was an observational retrospective study that focused on patients who underwent EGD before bariatric surgery in an academic medical center from January 2012 to July 2020.
All patients were evaluated at the Bariatric Center and met the bariatric surgery indications that were either a BMI ≥ 37.5 kg/m2 with or without obesity-related comorbidities or a BMI ≥ 32.5 kg/m2 with obesity-related comorbidities [13]. At our Bariatric Center, all patients routinely undergo a preoperative EGD to assess any abnormalities in the UGI that may impact the treatment plan.
The clinical data obtained from the patient electronic medical records included the demographics (i.e., sex, age, weight, height, and BMI), comorbidity conditions (i.e., alcohol use, smoking, hypertension, obstructive sleep apnea, diabetes mellitus, coronary artery disease, asthma, chronic obstructive pulmonary disease, anxiety, depression or other psychiatric disease, GERD, hypothyroidism, arthritis, and chronic liver disease), current medication use, and symptoms prior to endoscopy (i.e., heartburn, and acid regurgitation).
The definition of non-steroidal anti-inflammatory drug (NSAID) use was the history of aspirin or any NSAIDs taken within 1 month prior to EGD [14]. The excluded patients were those who had prior UGI tract or bariatric surgery or patients with incomplete data.
The reports of EGD were reviewed by the authors and classified into four groups based on their effects on management. Group 1 had normal EGD findings with no change in management. Group 2 had abnormal findings, which included non-erosive gastritis, non-erosive duodenitis, non-erosive esophagitis, esophageal ring, esophageal web, benign polyp, and Helicobacter pylori that did not require any change in surgical management. Group 3 had abnormal findings, which included mass lesion, peptic ulcers, arteriovenous malformation, bezoar, duodenal diverticulum, esophageal diverticulum, Barrett’s esophagus, erosive esophagitis, erosive gastritis, erosive duodenitis, and hiatal hernia that required a change in the surgical plan/approach or caused a delay in surgical treatment. Group 4 patients had contraindications to bariatric surgery that included varices and malignancy. In patients who had more than one endoscopic finding, the endoscopic findings in the highest group were used for the classification.
Categorical variables are represented as frequency and percentage, while continuous variables are represented as mean (standard deviation) or median (interquartile range). Univariate and multivariate analyses were used to find correlations between risk factors and abnormal findings in the UGI tract that required a change in the surgical plan/approach or caused a delay in surgical treatment (Group 3) or had contraindications to bariatric surgery (Group 4). For the univariate analysis, the Chi-square test or Fisher’s exact test was used with categorical variables, while the t test or Wilcoxon rank sum test was used with continuous variables. All variables were further assessed by multivariable analyses with backward step-wise selection, using likelihood ratio test with Akaike information criterion as the stopping rule. p values < 0.05 were considered statistically significant.
A nomogram was developed based on the results of the multivariate analyses to evaluate Group 3 and Group 4 endoscopic risk factors. Validation of the nomogram was performed by measuring discrimination and calibration curves. Bootstrap self-sample validation was performed using 500 bootstrap resamples of the developed dataset. The C-statistic was used to assess the discriminative ability of the nomogram. The calibration curves were used to compare the predicted probability with the observations in the study.
Results
A total of 461 patients were eligible for the analysis. Table 1 illustrates the patient characteristics, while the prevalences of the endoscopic findings classified by group are provided in Table 2.
Two hundred and sixty-five patients (57.5%) had one or more abnormal findings in the EGD screening. Non-erosive gastritis was the most common abnormal finding (31.2%) followed by H. pylori infection (18.7%), hiatal hernia (10.2%), benign polyp (8.5%), and peptic ulcer (7.4%). Nevertheless, none of the patients had UGI malignancy or varices (Table 3).
A comparison between patients who had normal EGD findings or abnormal findings that did not require any change in surgical management (Groups 1 and 2) and patients who had abnormal findings that required a change in the surgical plan/approach or caused a delay in surgical treatment or had contraindications to bariatric surgery (Groups 3 and 4) is illustrated in Table 4. The univariate analysis revealed that patient abnormalities in Group 3 were associated with male sex (OR 1.83, 95% CI 1.17–2.87; p = 0.008) and NSAID use (OR 3.88, 95% CI 1.63–9.23; p = 0.002). Multivariate analysis also indicated that patient abnormalities in Group 3 were considerably associated with male sex (OR 2.37, 95% CI 1.37–4.07; p = 0.002), NSAID use (OR 5.19, 95% CI 2.09–12.93; p < 0.001), and T2DM (OR 0.56, 95% CI 0.32–0.96; p = 0.03).
A subgroup analysis in patients ≥ 40 years of age based on our generalized additive model was performed (see Supplementary Material Fig. S1). A comparison between patients in Groups 1 and 2 and Group 3 is illustrated in Table 5. The univariate analysis revealed that patient abnormalities in Group 3 were associated with BMI (OR 1.06, 95% CI 1.01–1.12; p = 0.016), and NSAID use (OR 4.08, 95% CI 1.44–11.59; p = 0.008). Multivariate analysis also indicated that patient abnormalities in Group 3 were considerably associated with age (OR 1.09, 95% CI 1.02–1.17; p = 0.009), BMI (OR 1.09, 95% CI 1.03–1.16; p = 0.002), NSAID use (OR 5.35, 95% CI 1.70–16.79; p = 0.009), and T2DM (OR 0.35, 95% CI 0.14–0.89; p = 0.021).
A nomogram to predict endoscopic Group 3 findings in patients ≥ 40 years of age was developed based on age, NSAID use, and BMI (Fig. 1). The C-statistics of this predictive nomogram was 0.737 (95% CI 0.721 − 0.752), which suggested good discrimination. The calibration curve of the constructed nomogram to predict the risk of an endoscopic Group 3 finding yielded a mean absolute error of 0.05 (see Supplementary Material Fig. S2).
Discussion
EGD screening before bariatric surgery is advantageous, especially for detection and assessing abnormalities in the upper GI tract. However, the necessity of undergoing a routine UGI endoscopy before bariatric surgery is still debatable. From the European Association for Endoscopic Surgery clinical practice guidelines on bariatric surgery, the panel provided a conditional recommendation for routine EGD recognizing that selective endoscopy in patients with upper abdominal symptoms might be more appropriate [15]. However, the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) later recommended to consider EGD in all patients with or without upper GI symptoms who plan to undergo a bariatric procedure [4]. Similarly, the latest recommendation from the American Society for Metabolic and Bariatric Surgery stated that routine preoperative EGD is justifiable and should be done at the surgeon’s discretion [16].
In accordance with the IFSO position statement, we classified endoscopic findings into four groups based on their effects on management, except for H. pylori infection and low-grade erosive esophagitis (Los Angeles Classification (LA) grades A and B). We decided to categorize H. pylori infection into Group 2 according to the results of two systematic reviews and meta-analysis [17, 18], which showed that postoperative complications (i.e., bleeding or leakage), hospital length of stay, and weight loss after bariatric surgery were similar for H. pylori-positive versus H. pylori-negative patients. However, the results from a large national database found that H. pylori was an independent predictor of marginal ulceration in patients who underwent Roux-en-Y gastric bypass [19]. In any case, patients with this infection receive H. pylori eradication in the early postoperative period to prevent a marginal ulcer from developing in the late postoperative. On the other hand, we classified low-grade erosive esophagitis (LA grades A and B) into Group 3 since recent studies showed a high prevalence of pathological acid reflux in patients with erosive esophagitis LA grades A and B. A study in Chinese patients found that 24% of grade A and 55% of grade B esophagitis patients had pathological acid reflux [20]. Another study also found that one-third of LA grades A and B erosive esophagitis had pathological acid exposure [21]. Therefore, in our practice, low-grade erosive esophagitis requires an ambulatory reflux monitoring test to establish GERD prior to bariatric surgery, which would cause a delay in surgical treatment.
The patient characteristics in this study were similar to some previous studies related to sex and BMI but lower in age, NSAID use, PPI use, and history of reflux symptoms [6,7,8,9,10,11]. Preoperative EGD indicated that abnormal endoscopic findings were found in 57.5% of all cases, while clinically significant abnormal endoscopic findings accounted for around one-fourth of all cases. Non-erosive gastritis, H. pylori infection, and hiatal hernia were the most frequent abnormalities. These results were similar to studies conducted in Asia, namely Lee et al. [6] and Ng et al. [9]. However, studies conducted in the West, for example, by Wolter et al. [11], Schigt et al. [10], and Wiltberger et al. [7], reported prevalences of clinically significant abnormal endoscopic findings of 0.5%, 1.3%, and 10.7%, respectively, which were much lower compared to our study. Many factors may explain the differences, such as the definitions of clinically significant abnormal endoscopic findings, the patient’s race, age, and BMI, as well as the prevalence of GERD, Barrett’s esophagus, and gastric cancers among the centers.
The results of this study and other Asian studies illustrate that preoperative EGD is beneficial in the detection and treatment of pathologies and have an influence on decision-making on the type of bariatric surgery to ensure patient safety. However, no data are available to support the cost effectiveness of routinely performing preoperative EGD in all patients who are expected to undergo bariatric surgery. Therefore, it is essential to identify the predictive factors to predict the chances of detecting clinically significant endoscopic findings. This study found that male sex and NSAID use were found to be positive predictive factors for Group 3, which were similar to several previous studies [6, 22,23,24]. This study also found that patient age ≥ 40 years old with high BMI faced a greater risk of having Group 3 lesions. As a result, we used only patients who were ≥ 40 years old to simply the nomogram to predict endoscopic Group 3 lesions, which showed good discrimination. The nomogram we developed identified patients who should have a preoperative EGD, which would reduce overall costs and complications following EGD, as well as the risks of airborne infection, especially during the COVID-19 pandemic.
The results showed that T2DM had a negative correlation between patient factors and the prevalence of a clinically significant abnormal EGD. A subgroup analysis was performed to explain this. The analysis found a low prevalence of hiatal hernia, which was classified as an abnormal finding in Group 3, in DM patients. Compared to non-diabetes mellitus patients, T2DM had a marginally statistical significance (5.8% vs. 12.1%, p = 0.06).
The strengths of this study include the relatively large sample size in an Asian population, classifying definitions of UGI abnormal findings in particular groups by a gastroenterologist at our institute, and classifying each group based on real-life practice according to the recent literature. Furthermore, a nomogram was constructed to help identify patients who should have preoperative EGD to achieve a balance between the benefits and risks of preoperative EGD. However, some limitations need to be acknowledged. First, the nature of a retrospective study design. Second, many endoscopists performed the EGD procedure; however, the endoscopic findings were reviewed by experienced endoscopists. Performing all EGD procedures by a single endoscopist could minimize performance bias and result in higher-quality data. Third, the developed nomogram was mainly based on Asian population, thus there was a limitation to apply this for other ethnic groups. Lastly, the optimal cut-off threshold for performing EGD in the proposed nomogram was not determined and the external validation of this model is required.
Conclusion
This study revealed a high prevalence of abnormal endoscopic findings in preoperative EGD evaluations in Thai bariatric patients. Preoperative EGD should be considered in all patients undergoing bariatric surgery to find the UGI abnormalities that might require a change in the surgical decision plan, particularly in high-risk patients older than 40 years, male, and have a history of NSAID use. Our new nomogram may help endoscopists rationally utilize the EGD procedure prior to bariatric surgery. However, the external validation of this model is needed.
References
Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS (2003) Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289:76–79
Sowemimo OA, Yood SM, Courtney J, Moore J, Huang M, Ross R, McMillian U, Ojo P, Reinhold RB (2007) Natural history of morbid obesity without surgical intervention. Surg Obesity Related Dis 3:73–77
Ackermann MA, Serra EE, Duza GE (2020) Preoperative Management of Candidates for Bariatric Surgery. In: Gagner M, Cardoso AR, Palermo M, Noel P, Nocca D (eds) The perfect sleeve gastrectomy: a clinical guide to evaluation, treatment, and techniques. Springer International Publishing, Cham, pp 37–52
Brown WA, Johari Halim Shah Y, Balalis G, Bashir A, Ramos A, Kow L, Herrera M, Shikora S, Campos GM, Himpens J, Higa K (2020) IFSO Position statement on the role of esophago-gastro-duodenal endoscopy prior to and after bariatric and metabolic surgery procedures. Obes Surg 30:3135–3153
Parikh M, Liu J, Vieira D, Tzimas D, Horwitz D, Antony A, Saunders JK, Ude-Welcome A, Goodman A (2016) Preoperative endoscopy prior to bariatric surgery: a systematic review and meta-analysis of the literature. Obes Surg 26:2961–2966
Lee J, Wong SK, Liu SY, Ng EK (2017) Is preoperative upper gastrointestinal endoscopy in obese patients undergoing bariatric surgery mandatory? An asian perspective. Obes Surg 27:44–50
Wiltberger G, Bucher JN, Schmelzle M, Hoffmeister A, Dietrich A (2015) Preoperative endoscopy and its impact on perioperative management in bariatric surgery. Dig Surg 32:238–242
Sharaf R, Weinshel E, Bini E, Rosenberg J, Sherman A, Ren C (2004) Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg 14:1367–1372
Ng JY, Cheng AKS, Kim G, Kong LWC, Soe KT, Lomanto D, So JBY, Shabbir A (2016) Is elective gastroscopy prior to bariatric surgery in an asian cohort worthwhile? Obes Surg 26:2156–2160
Schigt A, Coblijn U, Lagarde S, Kuiken S, Scholten P, van Wagensveld B (2014) Is esophagogastroduodenoscopy before Roux-en-Y gastric bypass or sleeve gastrectomy mandatory? Surg Obesity Related Dis 10:411–417
Wolter S, Dupree A, Miro J, Schroeder C, Jansen MI, Schulze-Zur-Wiesch C, Groth S, Izbicki J, Mann O, Busch P (2017) Upper gastrointestinal endoscopy prior to bariatric surgery-mandatory or expendable? An analysis of 801 cases. Obes Surg 27:1938–1943
Committee ASoP, Wang A, Shaukat A, Acosta RD, Bruining DH, Chandrasekhara V, Chathadi KV, Eloubeidi MA, Fanelli RD, Faulx AL, Fonkalsrud L, Gurudu SR, Kelsey LR, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Pasha S, Saltzman JR, Yang J, Cash BD, DeWitt JM, 2015 Race and ethnicity considerations in GI endoscopy Gastrointest Endosc 82:593–599
Techagumpuch APS, Chansaenroj P, Boonyagard N, Wittayapairoch J, Poonthananiwatkul T, Chanswangphuvana P et al (2020) Thai society for metabolic and bariatric surgery consensus guideline on bariatric surgery for the treatment of obese patient in Thailand. J Med Assoc Thai 103:300–307
Graham DY, Smith JL (1986) Aspirin and the stomach. Ann Intern Med 104:390–398
Di Lorenzo N, Antoniou SA, Batterham RL, Busetto L, Godoroja D, Iossa A, Carrano FM, Agresta F, Alarçon I, Azran C, Bouvy N, Balaguè Ponz C, Buza M, Copaescu C, De Luca M, Dicker D, Di Vincenzo A, Felsenreich DM, Francis NK, Fried M, Gonzalo Prats B, Goitein D, Halford JCG, Herlesova J, Kalogridaki M, Ket H, Morales-Conde S, Piatto G, Prager G, Pruijssers S, Pucci A, Rayman S, Romano E, Sanchez-Cordero S, Vilallonga R, Silecchia G (2020) Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC, EASO and ESPCOP. Surg Endosc 34:2332–2358
Campos GM, Mazzini GS, Altieri MS, Docimo S Jr, DeMaria EJ, Rogers AM (2021) ASMBS position statement on the rationale for performance of upper gastrointestinal endoscopy before and after metabolic and bariatric surgery. Surg Obesity Related Dis 17:837–847
Smelt HJM, Smulders JF, Gilissen LPL, Said M, Ugale S, Pouwels S (2018) Influence of Helicobacter pylori infection on gastrointestinal symptoms and complications in bariatric surgery patients: a review and meta-analysis. Surg Obesity Related Dis 14:1645–1657
Mocanu V, Dang JT, Switzer N, Skubleny D, Shi X, de Gara C, Birch DW, Karmali S (2018) The effect of helicobacter pylori on postoperative outcomes in patients undergoing bariatric surgery: a systematic review and meta-analysis. Obes Surg 28:567–573
Schulman AR, Abougergi MS, Thompson CC (2017) H. Pylori as a predictor of marginal ulceration: a nationwide analysis. Obesity (Silver Spring, Md) 25:522–526
Qiu B, Zhang X, Bai T, Xu J, Xiang X, Hou X (2019) The importance of pH reflux monitoring test for the management of low-grade esophagitis in Chinese patients. Neurogastroenterol Motil 31:e13653
Zhang M, Tan N, Li Y, Chen M, Xiao Y (2019) Esophageal physiologic profiles within erosive esophagitis in China: Predominantly low-grade esophagitis with low reflux burden. Neurogastroenterol Motility 31:e13702
Gómez V, Bhalla R, Heckman MG, Florit PT, Diehl NN, Rawal B, Lynch SA, Loeb DS (2014) Routine screening endoscopy before bariatric surgery: is it necessary? Bariatric Surg Practice and Patient Care 9:143–149
Nam K, Shin JE, Kim SE, Baik GH, Choi SH, Lee JY, Park KS, Joo YE, Myung DS, Kim HJ, Song HJ, Choi SC, Kim HJ, Kim HY, Kim N (2018) Prevalence and risk factors for upper gastrointestinal diseases in health check-up subjects: a nationwide multicenter study in Korea. Scand J Gastroenterol 53:910–916
Muñoz R, Ibáñez L, Salinas J, Escalona A, Pérez G, Pimentel F, Guzmán S, Boza C (2009) Importance of routine preoperative upper GI endoscopy: why all patients should be evaluated? Obes Surg 19:427–431
Acknowledgements
The authors would like to thank Ms. Nannapat Pruphetkeaw from the Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Thailand, for her assistance in performing the statistical analysis of the data and Mr. Glenn Shingledecker for the proofreading and language support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Surawitch Sawathanon, Darawan Promchan, Meena Thongwong, Piyanun Wangkulangkul, Siripong Cheewatanakornkul, Suriya Keeratichananont, and Kamthorn Yolsuriyanwong have no conflict of interest or financial disclosure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sawathanon, S., Promchan, D., Thongwong, M. et al. Impact of preoperative esophagogastroduodenoscopy in patients undergoing bariatric surgery and development of a model to predict clinically significant abnormal endoscopic findings. Surg Endosc 37, 2202–2208 (2023). https://doi.org/10.1007/s00464-022-09391-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09391-8