Abstract
Aim
The impact of pelvis on the development of anastomotic leak (AL) in rectal cancer (RC) patients who underwent anterior resection (AR) remains unclear. The aim of this study was to evaluate the impact of pelvic dimensions on the risk of AL.
Methods
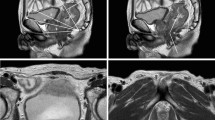
A total of 1058 RC patients undergoing AR from January 2013 to January 2016 were enrolled. Pelvimetric parameters were obtained using abdominopelvic computed tomography scans.
Results
Univariate analyses showed that pelvic inlet, pelvic outlet, interspinous distance, and intertuberous distance were significantly associated with the risk for AL (P < 0.05). Multivariate analysis confirmed that pelvic inlet and intertuberous distance were independent risk factors for AL (P < 0.05). Significant factors from multivariate analysis were assembled into the nomogram A (without pelvic dimensions) and nomogram B (with pelvic dimensions). The area under curve (AUC) of nomogram B was 0.72 (95% CI 0.67–0.77), which was better than the AUC of nomogram A (0.69, [95% CI 0.65–0.74]), but didn’t reach a statistical significance (P = 0.199). Decision curve supported that nomogram B was better than nomogram A.
Conclusion
Pelvic dimensions, specifically pelvic inlet and intertuberous distance, seemed to be independent predictors for postoperative AL in RC patients. Pelvic inlet and intertuberous distance incorporated with preoperative radiotherapy, preoperative albumin, conversion, and tumor diameter in the nomogram might provide a clinical tool for predicting AL.



Similar content being viewed by others
References
Ludwig SPMFGHK (1998) Anastomotic leakage impact on local recurrence and survival in surgery of colorectal cancer. Int J Colorectal Dis 13:160–163
Bell SW, Walker KG, Rickard MJ, Sinclair G, Dent OF, Chapuis PH, Bokey EL (2003) Anastomotic leakage after curative anterior resection results in a higher prevalence of local recurrence. Br J Surg 90:1261–1266
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102:462–479
Zhou C, Wu XR, Liu XH, Chen YF, Ke J, He XW, He XS, Hu T, Zou YF, Zheng XB, Liu HS, Hu JC, Wu XJ, Wang JP, Lan P (2018) Male gender is associated with an increased risk of anastomotic leak in rectal cancer patients after total mesorectal excision. Gastroenterol Rep 6:137–143
Pommergaard HC, Gessler B, Burcharth J, Angenete E, Haglind E, Rosenberg J (2014) Preoperative risk factors for anastomotic leakage after resection for colorectal cancer: a systematic review and meta-analysis. Colorectal Dis 16:662–671
Parthasarathy M, Greensmith M, Bowers D, Groot-Wassink T (2017) Risk factors for anastomotic leakage after colorectal resection: a retrospective analysis of 17 518 patients. Colorectal Dis 19:288–298
Mrak K, Uranitsch S, Pedross F, Heuberger A, Klingler A, Jagoditsch M, Weihs D, Eberl T, Tschmelitsch J (2016) Diverting ileostomy versus no diversion after low anterior resection for rectal cancer: a prospective, randomized, multicenter trial. Surgery 159:1129–1139
Ihnat P, Gunkova P, Peteja M, Vavra P, Pelikan A, Zonca P (2016) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30:4809–4816
Zur Hausen G, Grone J, Kaufmann D, Niehues SM, Aschenbrenner K, Stroux A, Hamm B, Kreis ME, Lauscher JC (2017) Influence of pelvic volume on surgical outcome after low anterior resection for rectal cancer. Int J Colorectal Dis 32:1125–1135
Targarona EM, Balague C, Pernas JC, Martinez C, Berindoague R, Gich I, Trias M (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247:642–649
Shimada T, Tsuruta M, Hasegawa H, Okabayashi K, Ishida T, Asada Y, Suzumura H, Kitagawa Y (2017) Pelvic inlet shape measured by three-dimensional pelvimetry is a predictor of the operative time in the anterior resection of rectal cancer. Surg Today 48:51–57
Jeong Yeon Kim YWK, Kim NK, Hur H, KangYong Lee BSM, Cho HJ (2011) Pelvic anatomy as a factor in laparoscopic rectal surgery. Surg Laparosc Endosc Percutaneous Tech 21:334–339
Kattan MW, Scardino PT (2007) Evidence for the usefulness of nomograms. Nat Clin Pract Urol 4:638–639
Karakiewicz PI, Briganti A, Chun FK, Trinh QD, Perrotte P, Ficarra V, Cindolo L, De la Taille A, Tostain J, Mulders PF, Salomon L, Zigeuner R, Prayer-Galetti T, Chautard D, Valeri A, Lechevallier E, Descotes JL, Lang H, Mejean A, Patard JJ (2007) Multi-institutional validation of a new renal cancer-specific survival nomogram. J Clin Oncol 25:1316–1322
Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, Group S (2017) The STROCSS statement: strengthening the Reporting of Cohort Studies in Surgery. Intl J Surg 46:198–202
Ogiso S, Yamaguchi T, Hata H, Fukuda M, Ikai I, Yamato T, Sakai Y (2011) Evaluation of factors affecting the difficulty of laparoscopic anterior resection for rectal cancer: "narrow pelvis" is not a contraindication. Surg Endosc 25:1907–1912
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T (2009) Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 146:483–489
Eberl T, Jagoditsch M, Klingler A, Tschmelitsch J (2008) Risk factors for anastomotic leakage after resection for rectal cancer. Am J Surg 196:592–598
Steffen T, Tarantino I, Hetzer FH, Warschkow R, Lange J, Zund M (2008) Safety and morbidity after ultra-low coloanal anastomoses: J-pouch vs end-to-end reconstruction. Int J Colorectal Dis 23:277–281
Bhangu A, Rasheed S, Brown G, Tait D, Cunningham D, Tekkis P (2014) Does rectal cancer height influence the oncological outcome? Colorectal Dis 16:801–808
Chanchan Xiao MZ, Yang X, Xiao F, Liu X, Guo Yi, Li X, Cao H, Luo J (2019) Novel nomogram with microvascular density in the surgical margins can accurately predict the risk for anastomotic leakage after anterior resection for rectal cancer. J Surg Oncol 120:1412–1419
Chau J, Solomon J, Liberman AS, Charlebois P, Stein B, Lee L (2019) Pelvic dimensions on preoperative imaging can identify poor-quality resections after laparoscopic low anterior resection for mid- and low rectal cancer. Surg Endosc. https://doi.org/10.1007/s00464-019-07209-8
Atasoy G, Arslan NC, Elibol FD, Sagol O, Obuz F, Sokmen S (2018) Magnetic resonance-based pelvimetry and tumor volumetry can predict surgical difficulty and oncologic outcome in locally advanced mid-low rectal cancer. Surg Today 48:1040–1051
Baik SH, Kim NK, Lee KY, Sohn SK, Cho CH, Kim MJ, Kim H, Shinn RK (2008) Factors influencing pathologic results after total mesorectal excision for rectal cancer: analysis of consecutive 100 cases. Ann Surg Oncol 15:721–728
Escal L, Nougaret S, Guiu B, Bertrand MM, de Forges H, Tetreau R, Thezenas S, Rouanet P (2018) MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg 105:140–146
Adler JT (2008) Gray's anatomy the anatomical basis of clinical practice. Elsevier, Philadelphia
Zhang X, Gao Y, Dai X, Zhang H, Shang Z, Cai X, Shen T, Cheng X, Yu K, Li Y (2018) Short- and long-term outcomes of transanal versus laparoscopic total mesorectal excision for mid-to-low rectal cancer: a meta-analysis. Surg Endosc 33:972–985
Lei P, Ruan Y, Yang X, Fang J, Chen T (2018) Trans-anal or trans-abdominal total mesorectal excision? A systematic review and meta-analysis of recent comparative studies on perioperative outcomes and pathological result. Int J Surg 60:113–119
Kang L, Chen WH, Luo SL, Luo YX, Liu ZH, Huang MJ, Wang JP (2016) Transanal total mesorectal excision for rectal cancer: a preliminary report. Surg Endosc 30:2552–2562
Acknowledgements
The authors thank Dr. Jian-ping Wang for his help with study design at the beginning of this study.
Funding
This work was supported by National Key R&D Program of China (No. 2017YFC1308800), National Natural Science Foundation of China (No. 81870383), Guangdong Natural Science Foundation (Nos. 2016A030310187 and 2017A030313785), Science and Technology Planning Project of Guangzhou City (No. 201804010014).
Author information
Authors and Affiliations
Contributions
ZLY and XHL contributed to study concept and design, acquisition, analysis, and interpretation of data, and drafting of the manuscript. HSL, JK, YFZ, WTC, and ZYZ contributed to data collections and manuscript review. JX, PL, XRW and XJW contributed to study concept and design, analysis and interpretation of data, and critical revision of the manuscript for important intellectual content. XRW and XJW supervised the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Disclosures
The author Zhao-liang Yu, Xuan-hui Liu, Hua-shan Liu, Jia Ke, Yi-feng Zou, Wu-teng Cao, Jian Xiao, Zhi-yang Zhou, Ping Lan, Xiao-jian Wu, and Xian-rui Wu have no conflicts of interest or financial ties to disclose.
Informed consent
This is a retrospective trial with demonstrated minimal risk and we petition BPG for waiver of informed consent.
Institutional review board
This study was approved by the Institutional Review Board (IRB) of The Sixth Affiliated Hospital of Sun Yat-sen University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiao-jian Wu and Xian-rui Wu contributed equally to this study as co-corresponding authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, Zl., Liu, Xh., Liu, Hs. et al. Impact of pelvic dimensions on anastomotic leak after anterior resection for patients with rectal cancer. Surg Endosc 35, 2134–2143 (2021). https://doi.org/10.1007/s00464-020-07617-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07617-1