Abstract
Introduction
Stray energy transfer from monopolar radiofrequency energy during laparoscopy can be potentially catastrophic. Robotic surgery is increasing in popularity; however, the risk of stray energy transfer during robotic surgery is unknown. The purpose of this study was to (1) quantify stray energy transfer using robotic instrumentation, (2) determine strategies to minimize the transfer of energy, and (3) compare robotic stray energy transfer to laparoscopy.
Methods
In a laparoscopic trainer, a monopolar instrument (L-hook) was activated with DaVinci Si (Intuitive, Sunnyvale, CA) robotic instruments. A camera and assistant grasper were inserted to mimic a minimally invasive cholecystectomy. During activation of the L-hook, the non-electric tips of the camera and grasper were placed adjacent to simulated tissue (saline-soaked sponge). The primary outcome was change in temperature from baseline (°C) measured nearest the tip of the non-electric instrument.
Results
Simulated tissue nearest the robotic grasper increased an average of 18.3 ± 5.8 °C; p < 0.001 from baseline. Tissue nearest the robotic camera tip increased (9.0 ± 2.1 °C; p < 0.001). Decreasing the power from 30 to 15 W (18.3 ± 5.8 vs. 2.6 ± 2.7 °C, p < 0.001) or using low-voltage cut mode (18.3 ± 5.8 vs. 3.1 ± 2.1 °C, p < 0.001) reduced stray energy transfer to the robotic grasper. Desiccating tissue, in contrast to open air activation, also significantly reduced stray energy transfer for the grasper (18.3 ± 5.8 vs. 0.15 ± 0.21 °C, p < 0.001) and camera (9.0 ± 2.1 vs. 0.24 ± 0.34 °C, p < 0.001).
Conclusions
Stray energy transfer occurs during robotic surgery. The assistant grasper carries the highest risk for thermal injury. Similar to laparoscopy, stray energy transfer can be reduced by lowering the power setting, utilizing a low-voltage cut mode instead of coagulation mode and avoiding open air activation. These practical findings can aid surgeons performing robotic surgery to reduce injuries from stray energy.






Similar content being viewed by others
References
Tuncel U, Ozgenel GY (2005) Thermal injury due to electrosurgery. Ulus Travma Acil Cerrahi Derg 11(1):76–77
Martin KE et al (2016) Quantifying inadvertent thermal bowel injury from the monopolar instrument. Surg Endosc 30(11):4776–4784
Morrison JE Jr, Jacobs VR (2007) Rupture of the spleen with the harmonic scalpel: case report of an unexplained complication. Jsls 11(2):268–271
Awwad JT, Isaacson K (1996) The harmonic scalpel: an intraoperative complication. Obstet Gynecol 88(4 Pt 2):718–720
Harrell AG, Kercher KW, Heniford BT (2004) Energy sources in laparoscopy. Semin Laparosc Surg 11(3):201–209
Sankaranarayanan G et al (2013) Common uses and cited complications of energy in surgery. Surg Endosc 27(9):3056–3072
Willson PD, van der Walt JD, Rogers J (1995) Electrosurgical coupling to a metal cannula causing skin burns during laparoscopic surgery. Minim Invasive Ther 4(3):163–164
Willson PD, McAnena OJ, Peters EE (1994) A fatal complication of diathermy in laparoscopic surgery. Minim Invasive Ther 3(1):19–20
Tucker RD (1995) Laparoscopic electrosurgical injuries: survey results and their implications. Surg Laparosc Endosc 5(4):311–317
Odell RC (2013) Surgical complications specific to monopolar electrosurgical energy: engineering changes that have made electrosurgery safer. J Minim Invasive Gynecol 20(3):288–298
Jones EL et al (2017) Stray energy transfer during endoscopy. Surg Endosc 31(10):3946–3951. https://doi.org/10.1007/s00464-017-5427-y
Bojja-Venkatakrishnan S, Jones EL, Kiourti A (2018) Unintended RF energy coupling during endoscopy. Bioelectromagnetics 39(1):77–82. https://doi.org/10.1002/bem.22085
Guzman C et al (2019) Estimating the incidence of stray energy burns during laparoscopic surgery based on two statewide databases and retrospective rates: an opportunity to improve patient safety. Surg Technol Int 34:30–34
Townsend NT et al (2017) Single-incision laparoscopic surgery increases the risk of unintentional thermal injury from the monopolar "Bovie" instrument in comparison with traditional laparoscopy. Surg Endosc 31(8):3146–3151. https://doi.org/10.1007/s00464-016-5339-2
Townsend NT et al (2016) Unintended stray energy from monopolar instruments: beware the dispersive electrode cord. Surg Endosc 30(4):1333–1336. https://doi.org/10.1007/s00464-015-4388-2
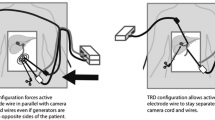
Robinson TN et al (2015) Separating the laparoscopic camera cord from the monopolar "Bovie" cord reduces unintended thermal injury from antenna coupling: a randomized controlled trial. Ann Surg 261(6):1056–1060. https://doi.org/10.1097/SLA.0000000000000841
Jones EL et al (2012) Radiofrequency energy antenna coupling to common laparoscopic instruments: practical implications. Surg Endosc 26(11):3053–3057. https://doi.org/10.1007/s00464-012-2312-6
Mendez-Probst CE et al (2011) Stray electrical currents in laparoscopic instruments used in da Vinci(R) robot-assisted surgery: an in vitro study. J Endourol 25(9):1513–1517
Overbey DM et al (2017) Hand-to-hand coupling and strategies to minimize unintentional energy transfer during laparoscopic surgery. J Surg Res. 219:103–107. https://doi.org/10.1016/j.jss.2017.05.091
Townsend NT et al (2015) Antenna coupling explains unintended thermal injury caused by common operating room monitoring devices. Surg Laparosc Endosc Percutan Tech 25(2):111–113. https://doi.org/10.1097/SLE.0000000000000137
Paniccia A et al (2014) Electromagnetic interference caused by common surgical energy-based devices on an implanted cardiac defibrillator. Am J Surg. 208(6):932–936. https://doi.org/10.1016/j.amjsurg.2014.09.011
Robinson TN et al (2014) Effect of radiofrequency energy emitted from monopolar "Bovie" instruments on cardiac implantable electronic devices. J Am Coll Surg 219(3):399–406. https://doi.org/10.1016/j.jamcollsurg.2014.03.060
Jones EL et al (2013) Blend mode reduces unintended thermal injury by laparoscopic monopolar instruments: a randomized controlled trial. Surg Endosc 27(11):4016–4020. https://doi.org/10.1007/s00464-013-3032-2
Govekar HR et al (2012) Effect of monopolar radiofrequency energy on pacemaker function. Surg Endosc 26(10):2784–2788. https://doi.org/10.1007/s00464-012-2279-3
Wu MP et al (2000) Complications and recommended practices for electrosurgery in laparoscopy. Am J Surg 179(1):67–73
Abu-Rafea B et al (2011) Monopolar electrosurgery through single-port laparoscopy: a potential hidden hazard for bowel burns. J Minim Invasive Gynecol 18(6):734–740
Jones ELM, Dean J (2018) Surgical energy. In: Henke PK, Hochwald SN, Tiao GM, Fischer JEE, Christopher E (eds) Fischer's mastery of surgery. Wolters Kluwer, Philadelphia
Gurtcheff SE (2008) Introduction to the MAUDE database. Clin Obstet Gynecol 51(1):120–123
Overbey DM et al (2015) Surgical energy-based device injuries and fatalities reported to the food and drug administration. J Am Coll Surg 221(1):197–205.e1. https://doi.org/10.1016/j.jamcollsurg.2015.03.031Epub 2015 Mar 27
Abraham NE, Simon R, Shah O (2011) Thermal injury causing delayed perforation of small bowel after transurethral resection of bladder tumor without evidence of bladder perforation. Can J Urol 18(4):5836–5838
Cassaro S (2015) Delayed manifestations of laparoscopic bowel injury. Am Surg 81(5):478–482
Berry SM et al (1994) Thermal injury of the posterior duodenum during laparoscopic cholecystectomy. Surg Endosc 8(3):197–200
Campagnacci R et al (2007) Electrothermal bipolar vessel sealing device vs ultrasonic coagulating shears in laparoscopic colectomies: a comparative study. Surg Endosc 21(9):1526–1531
Machado NO (2016) Duodenal injury post laparoscopic cholecystectomy: incidence, mechanism, management and outcome. World J Gastrointest Surg 8(4):335–344
Madani A et al (2014) Fundamental use of surgical energy (FUSE): a curriculum on surgical energy-based devices. Surg Endosc 28(9):2509–2512
Jones SB et al (2017) Fundamental use of surgical energy (FUSE): an essential educational program for operating room safety. Perm J 21:16–050
Reissis Y et al (2013) The effect of temperature on the viability of human mesenchymal stem cells. Stem Cell Res Ther 4(6):139
Zhang Y et al (2018) Temperature-dependent cell death patterns induced by functionalized gold nanoparticle photothermal therapy in melanoma cells. Sci Rep 8(1):8720
Funding
This study was funded by a 2016 SAGES Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Overbey received a 2016 SAGES Research Grant for this study. No study number was assigned. Drs. Carmichael, Wikiel, Hirth, Chapman, Moore, Barnett, T. Jones, Robinson, and E. Jones have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Overbey, D.M., Carmichael, H., Wikiel, K.J. et al. Monopolar stray energy in robotic surgery. Surg Endosc 35, 2084–2090 (2021). https://doi.org/10.1007/s00464-020-07605-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07605-5