Abstract
Background
The efficacy and outcomes of laparoscopic resection for pancreatic neuroendocrine tumors (PNETs) are well established; however, specific data regarding the outcomes of laparoscopic pancreaticoduodenectomy (L-PD) are limited. The purpose of the present study was to compare the clinical and oncological outcomes following L-PD versus open PD (O-PD) in patients with PNETs.
Methods
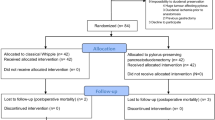
This retrospective study included 149 patients with PNETs who underwent PD at the Asan Medical Center between January 2006 and December 2017. In 58 patients, a laparoscopic approach was used (L-PD group), and in 91, an open technique was used (O-PD group).
Results
The mean operative time was longer in the L-PD group than in the O-PD group (417.4 min vs. 362.2 min; p = 0.002), and the mean duration of postoperative stay was shorter in the L-PD group (12.6 days vs. 17.8 days; p < 0.001). The estimated blood loss (433.2 ml vs. 415.0 ml; p = 0.824) and the overall complication rate (34.5% vs. 38.5%; p = 0.624) did not significantly differ between the two groups. Regarding the oncological outcomes, there were no significant differences in the resection margins, tumor size, tumor grading, or T/N stage. The number of harvested lymph nodes in the L-PD group was lower than that in the O-PD group (7.1 vs. 10.8; p = 0.002). The 3-year overall survival rate was 91.9% in the L-PD group and 93.6% in the O-PD group (p = 0.974). The 3-year disease-free survival rate was 94.8% in the L-PD group and 86.7% in the O-PD group (p = 0.225).
Conclusions
L-PD is feasible for the treatment of PNETs in selected patients and has the advantages of short recovery time and reduced hospital stay. The survival rate was similar in both groups; however, due to the difference in the harvested lymph nodes, a randomized trial should confirm the oncological safety of L-PD for PNETs.



Similar content being viewed by others
References
Halfdanarson TR, Rubin J, Farnell MB, Grant CS, Petersen GM (2008) Pancreatic endocrine neoplasms: epidemiology and prognosis of pancreatic endocrine tumors. Endocr Relat Cancer 15:409–427
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26:3063–3072
Ekeblad S, Skogseid B, Dunder K, Oberg K, Eriksson B (2008) Prognostic factors and survival in 324 patients with pancreatic endocrine tumor treated at a single institution. Clin Cancer Res 14:7798–7803
Sadot E, Reidy-Lagunes DL, Tang LH, Do RK, Gonen M, D’Angelica MI, DeMatteo RP, Kingham TP, Groot Koerkamp B, Untch BR, Brennan MF, Jarnagin WR, Allen PJ (2016) Observation versus resection for small asymptomatic pancreatic neuroendocrine tumors: a matched case-control study. Ann Surg Oncol 23:1361–1370
Spolverato G, Bagante F, Aldrighetti L, Poultsides G, Bauer TW, Field RC, Marques HP, Weiss M, Maithel SK, Pawlik TM (2017) Neuroendocrine liver metastasis: prognostic implications of primary tumor site on patients undergoing curative intent liver surgery. J Gastrointest Surg 21:2039–2047
Cheema A, Weber J, Strosberg JR (2012) Incidental detection of pancreatic neuroendocrine tumors: an analysis of incidence and outcomes. Ann Surg Oncol 19:2932–2936
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8:408–410
Cho CS, Kooby DA, Schmidt CM, Nakeeb A, Bentrem DJ, Merchant NB, Parikh AA, Martin RC 2nd, Scoggins CR, Ahmad SA, Kim HJ, Hamilton N, Hawkins WG, Weber SM (2011) Laparoscopic versus open left pancreatectomy: can preoperative factors indicate the safer technique? Ann Surg 253:975–980
Jusoh AC, Ammori BJ (2012) Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. Surg Endosc 26:904–913
Al-Taan OS, Stephenson JA, Briggs C, Pollard C, Metcalfe MS, Dennison AR (2010) Laparoscopic pancreatic surgery: a review of present results and future prospects. HPB 12:239–243
Song KB, Kim SC, Park JB, Kim YH, Jung YS, Kim MH, Lee SK, Seo DW, Lee SS, Park DH, Han DJ (2011) Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg Endosc 25:3364–3372
Xie K, Zhu YP, Xu XW, Chen K, Yan JF, Mou YP (2012) Laparoscopic distal pancreatectomy is as safe and feasible as open procedure: a meta-analysis. World J Gastroenterol 18:1959–1967
Drymousis P, Raptis DA, Spalding D, Fernandez-Cruz L, Menon D, Breitenstein S, Davidson B, Frilling A (2014) Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. HPB 16:397–406
Tamburrino D, Partelli S, Renzi C, Crippa S, Muffatti F, Perali C, Parisi A, Randolph J, Fusai GK, Cirocchi R, Falconi M (2017) Systematic review and meta-analysis on laparoscopic pancreatic resections for neuroendocrine neoplasms (PNENs). Expert Rev Gastroenterol Hepatol 11:65–73
Han SH, Han IW, Heo JS, Choi SH, Choi DW, Han S, You YH (2018) Laparoscopic versus open distal pancreatectomy for nonfunctioning pancreatic neuroendocrine tumors: a large single-center study. Surg Endosc 32:443–449
Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, Park KM, Lee YJ (2015) Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg 262:146–155
Lee CS, Kim EY, You YK, Hong TH (2018) Perioperative outcomes of laparoscopic pancreaticoduodenectomy for benign and borderline malignant periampullary disease compared to open pancreaticoduodenectomy. Langenbeck’s Arch Surg 403:591–597
Daniel Dindo M, Nicolas Demartines MD, Pierre-Alain Clavien MD (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591
Mehrabi A, Fischer L, Hafezi M, Dirlewanger A, Grenacher L, Diener MK, Fonouni H, Golriz M, Garoussi C, Fard N, Rahbari NN, Werner J, Buchler MW (2014) A systematic review of localization, surgical treatment options, and outcome of insulinoma. Pancreas 43:675–686
Pang L, Kong J, Wang Y, Zhang Y (2018) Laparoscopic versus open pylorus-preserving pancreatoduodenectomy. The first meta-analyse of retrospective matched cases. Acta Cir Bras 33:40–48
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 215:810–819
Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, Andren-Sandberg A, Asbun HJ, Bockhorn M, Buchler MW, Conlon KC, Fernandez-Cruz L, Fingerhut A, Friess H, Hartwig W, Izbicki JR, Lillemoe KD, Milicevic MN, Neoptolemos JP, Shrikhande SV, Vollmer CM, Yeo CJ, Charnley RM (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156:591–600
Tomassetti P, Campana D, Piscitelli L, Casadei R, Santini D, Nori F, Morselli-Labate AM, Pezzilli R, Corinaldesi R (2005) Endocrine pancreatic tumors: factors correlated with survival. Ann Oncol 16:1806–1810
Bettini R, Boninsegna L, Mantovani W, Capelli P, Bassi C, Pederzoli P, Delle Fave GF, Panzuto F, Scarpa A, Falconi M (2008) Prognostic factors at diagnosis and value of WHO classification in a mono-institutional series of 180 non-functioning pancreatic endocrine tumours. Ann Oncol 19:903–908
Bilimoria KY, Talamonti MS, Tomlinson JS, Stewart AK, Winchester DP, Ko CY, Bentrem DJ (2008) Prognostic score predicting survival after resection of pancreatic neuroendocrine tumors: analysis of 3851 patients. Ann Surg 247:490–500
Justin R, Parekh SCW, Bergsland Emily K, Nakakura Eric K (2012) Lymph node sampling rates and predictors of nodal metastasis in pancreatic neuroendocrine tumor resections: the UCSF experience with 149 patients. Pancreas 41:840–844
Funding
This study was supported by a Grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, South Korea (Grant Number: HI14C2640).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hanbaro Kim, Ki Byung Song, Dae Wook Hwang, Jae Hoon Lee, Shadi Alshammary, and Song Cheol Kim have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H., Song, K.B., Hwang, D.W. et al. Laparoscopic versus open pancreaticoduodenectomy for pancreatic neuroendocrine tumors: a single-center experience. Surg Endosc 33, 4177–4185 (2019). https://doi.org/10.1007/s00464-019-06969-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06969-7