Abstract
Background
Day-case surgery (DCS) has become increasingly popular over recent years, as has laparoscopic liver resection (LLR) for the treatment of benign or malignant liver tumours. The purpose of this prospective study was to demonstrate the feasibility of minor LLR as DCS.
Methods
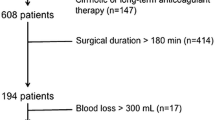
Prospective, intention-to-treat, non-randomised study of patients undergoing minor LLR between July 2015 and December 2017. Exclusion criteria were resection by laparotomy, major LLR, difficult locations for minor LLR, history of major abdominal surgery, hepatobiliary procedures without liver parenchyma resection, cirrhosis with Child > A and/or portal hypertension, significant medical history and exclusion criteria for DCS. The primary endpoint was the unplanned overnight admission rate. Secondary endpoints were the reason for exclusion, complication data, criteria for DCS evaluation, satisfaction and compliance with the protocol.
Results
One hundred sixty-seven patients underwent liver resection during the study period. LLR was performed in 92 patients (55%), as DCS in 23 patients (25%). Reasons for minor LLR were liver metastasis (n = 9), hepatic adenoma (n = 5), hepatocellular carcinoma (n = 4), ciliated hepatic foregut cyst (n = 2) and other benign tumours (n = 3). All day-case minor LLR, except two patients, consisted of single wedge resection, while one patient underwent left lateral sectionectomy. There were four unplanned overnight admissions (17.4%), one unscheduled consultation (4.3%), two hospital readmissions (8.6%) and no major complications/mortality. Compliance with the protocol was 69.5%. Satisfaction rate was 91%.
Conclusion
In selected patients, day-case minor LLR is feasible with acceptable complication and readmission rates. Day-case minor LLR can therefore be legitimately proposed in selected patients.




Similar content being viewed by others
Abbreviations
- DCS:
-
Day-case surgery
- LLR:
-
Laparoscopic liver resection
References
Mjåland O, Raeder J, Aasboe V, Trondsen E, Buanes T (1997) Outpatient laparoscopic cholecystectomy. Br J Surg 84:958–961
Trondsen E, Mjâland O, Raeder J, Buanes T (2000) Day-case laparoscopic fundoplication for gastro-oesophageal reflux disease. Br J Surg 87:1708–1711
Mariette C, Piessen G, Balon JM, Guidat A, Lebuffe G, Triboulet JP (2007) The safety of the same-day discharge for selected patients after laparoscopic fundoplication: a prospective cohort study. Am J Surg 194:279–282
Rebibo L, Dhahri A, Badaoui R, Dupont H, Regimbeau JM (2015) Laparoscopic sleeve gastrectomy as day-case surgery (without overnight hospitalization). Surg Obes Relat Dis 11:335–342
Bhalla A, Peacock O, Tierney GM, Tou S, Hurst NG, Speake WJ, Williams JP, Lund JN (2015) Day-case closure of ileostomy: feasible, safe and efficient. Colorectal Dis 17:820–823
Gignoux B, Pasquer A, Vulliez A, Lanz T (2015) Outpatient colectomy within an enhanced recovery program. J Visc Surg 152:11–15
Gagner M, Rheault M, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor [abstract]. Surg Endosc 6:97–98
Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232:753–762
Croome KP, Yamashita MH (2010) Laparoscopic vs open hepatic resection for benign and malignant tumors: an updated meta-analysis. Arch Surg 145:1109–1118
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:385–392 discussion 392-4.
Wang C, Zheng G, Zhang W, Zhang F, Lv S, Wang A, Fang Z (2017) Enhanced recovery after surgery programs for liver resection: a meta-analysis. J Gastrointest Surg 21:472–486
Gaillard M, Tranchart H, Lainas P, Tzanis D, Franco D, Dagher I (2015) Ambulatory laparoscopic minor hepatic surgery: retrospective observational study. J Visc Surg 152:292–296
de’Angelis N, Menahem B, Compagnon P, Merle JC, Brunetti F, Luciani A, Cherqui D, Laurent A (2017) Minor laparoscopic liver resection: toward 1-day surgery? Surg Endosc 31:4458–4465
Tranchart H, Fuks D, Lainas P, Gaillard M, Dagher I, Gayet B (2017) Laparoscopic liver surgery: towards a day-case management. Surg Endosc 31:5295–5302
Kraft K, Mariette C, Sauvanet A, Balon JM, Douard R, Fabre S, Guidat A, Huten N, Johanet H, Laurent A, Muscari F, Pessaux P, Piermé JP, Piessen G, Raucoules-Aimé M, Rault A, Vons C; French Society of Gastrointestinal Surgery; Association for Hepatobiliary and Transplantation Surgery (2011) Indications for ambulatory gastrointestinal and endocrine surgery in adults. J Visc Surg 148:69–74
Badaoui R, Alami Chentoufi Y, Hchikat A, Rebibo L, Popov I, Dhahri A, Antoun G, Regimbeau JM, Lorne E, Dupont H (2016) Outpatient laparoscopic sleeve gastrectomy: first 100 cases. J Clin Anesth 34:85–90
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
van den Broek MA, van Dam RM, van Breukelen GJ, Bemelmans MH, Oussoultzoglou E, Pessaux P, Dejong CH, Freemantle N, Olde Damink SW (2011) Development of a composite endpoint for randomized controlled trials in liver surgery. Br J Surg 98:1138–1145
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828, discussion 828–9
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ, Fan ST, Nimura Y, Figueras J, Vauthey JN, Rees M, Adam R, Dematteo RP, Greig P, Usatoff V, Banting S, Nagino M, Capussotti L, Yokoyama Y, Brooke-Smith M, Crawford M, Christophi C, Makuuchi M, Büchler MW, Weitz J (2011) Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford) 13:528–535
Le Roux F, Rebibo L, Cosse C, Chatelain D, Nguyen-Khac E, Badaoui R, Regimbeau JM (2018) Benefits of laparoscopic approach for resection of liver tumors in cirrhotic patients. J Laparoendosc Adv Surg Tech A 28(5):553–561
Hallet J, Sa Cunha A, Cherqui D, Gayet B, Goéré D, Bachellier P, Laurent A, Fuks D, Navarro F, Pessaux P, French Colorectal Liver Metastases Working Group, Association Française de Chirurgie (2017) Laparoscopic compared to open repeat hepatectomy for colorectal liver metastases: a multi-institutional propensity-matched analysis of short- and long-term outcomes. World J Surg 41:3189–3198
Cauchy F, Fuks D, Zarzavadjian Le Bian A, Belghiti J, Costi R (2014) Metabolic syndrome and non-alcoholic fatty liver disease in liver surgery: the new scourges? World J Hepatol 6:306–314
Chang S, Laurent A, Tayar C, Karoui M, Cherqui D (2007) Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg 94:58–63
Hasegawa Y, Wakabayashi G, Nitta H, Takahara T, Katagiri H, Umemura A, Makabe K, Sasaki A (2017) A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc 31:5356–5363
de Boer MT, Molenaar IQ, Porte RJ (2007) Impact of blood loss on outcome after liver resection. Dig Surg 24:259–264
Wong-Lun-Hing EM, van Dam RM, van Breukelen GJ, Tanis PJ, Ratti F, van Hillegersberg R, Slooter GD, de Wilt JH, Liem MS, de Boer MT, Klaase JM, Neumann UP, Aldrighetti LA, Dejong CH, ORANGE II Collaborative Group (2017) Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study). Br J Surg 104:525–535
Pattaro G, Fuks D, Tranchart H, Ettorre GM, Suhool A, Bourdeaux C, Lainas P, Dagher I, Gayet B (2017) Laparoscopic left liver resections: how far can we go? Surg Endosc 31:5303–5311
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Lionel Rebibo, Pauline Leourier, Rachid Badaoui, Fabien Le Roux, Emmanuel Lorne and Jean-Marc Regimbeau have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Rebibo, L., Leourier, P., Badaoui, R. et al. Minor laparoscopic liver resection as day-case surgery (without overnight hospitalisation): a pilot study. Surg Endosc 33, 261–271 (2019). https://doi.org/10.1007/s00464-018-6306-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6306-x