Abstract
Background
We examined how problem-solving coaching impacts trainee skill acquisition and physiologic stress as well as how trainee sensitivity to feedback, known as self-monitoring ability, impacts coaching effectiveness.
Methods
Medical students completed a pre-training demographics questionnaire, a 12-item self-monitoring ability scale (1 = always false, 5 = always true), and baseline FLS Task 5 with physiologic sensors. After watching a laparoscopic suturing instructional video, students practiced the task for 30 min, either with a surgical coach, or alone, depending on condition. The coach logged frequency of coaching behaviors according to a task-specific coaching script. Trainees then completed FLS Task 5 with physiologic sensors, a post-training questionnaire, and a 12-item coaching quality evaluation (1 = poor, 5 = very good).
Results
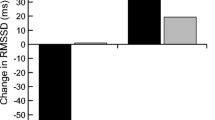
Twenty-four students (age 24.5 ± 1.4; 54% men; 58% MS4) participated in the study. All were fairly high self-monitors (3.8 ± 0.76). No differences in baseline suturing skills between the groups emerged. Improvement in the coaching group‘s suturing (N = 12; 285.0 ± 79.9) was significantly higher than the control group (N = 12; 200.9 ± 110.3). One measure of physiologic stress (rMSSD) was significantly higher in the coaching group. Trainees who received more coaching demonstrated larger improvements (r = 0.7, p < 0.05). Overall ,perceived quality of the coaching relationship was high (4.4 ± 0.6). There was no correlation between trainee self-monitoring ability and skill improvement.
Conclusions
This work suggests that coaching may increase heart rate variability of trainees, indicating coping well with training. Trainee disposition toward feedback did not play a role in this relationship.

Similar content being viewed by others
Abbreviations
- OR:
-
Operating room
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- RF:
-
Respiration frequency
- ECG:
-
Electrocardiogram
References
Parsloe E (1999) The manager as coach and mentor. CIPD Publishing, London
Cole SJ, Mackenzie H, Ha J, Hanna GB, Miskovic D (2014) Randomized controlled trial on the effect of coaching in simulated laparoscopic training. Surg Endosc 28(3):979–986
Kirkpatrick JS (2012) A comparison C1-C2 transarticular screw placement after self-education and mentored education of orthopaedic residents. J Spinal Disord Tech 25(6):E155–E160
Porte MC, Xeroulis G, Reznick RK, Dubrowski A (2007) Verbal feedback from an expert is more effective than self-accessed feedback about motion efficiency in learning new surgical skills. Am J Surg 193(1):105–110
Gala R, Orejuela F, Gerten K et al (2013) Effect of validated skills simulation on operating room performance in obstetrics and gynecology residents: a randomized controlled trial. Obstet Gynecol 121(3):578–584
Hamad GG, Brown MT, Clavijo-Alvarez JA (2007) Postoperative video debriefing reduces technical errors in laparoscopic surgery. Am J Surg 194(1):110–114
Grantcharov TP, Schulze S, Kristiansen VB (2007) The impact of objective assessment and constructive feedback on improvement of laparoscopic performance in the operating room. Surg Endosc 21(12):2240–2243
Boyle E, O’Keeffe DA, Naughton PA, Hill AD, McDonnell CO, Moneley D (2011) The importance of expert feedback during endovascular simulator training. J Vasc Surg 54(1):240–248 e241
Trehan A, Barnett-Vanes A, Carty MJ, McCulloch P, Maruthappu M (2015) The impact of feedback of intraoperative technical performance in surgery: a systematic review. BMJ Open 5(6):e006759
Yule S, Parker SH, Wilkinson J et al (2015) Coaching non-technical skills improves surgical residents’ performance in a simulated operating room. J Surg Educ 72(6):1124–1130
Snyder M, Gangestad S (1986) On the nature of self-monitoring: matters of assessment, matters of validity. J Pers Soc Psychol 51(1):125–139
London M, Smither JW (2002) Feedback orientation, feedback culture, and the longitudinal performance management process. Hum Resour Manag Rev 12(1):81–100
Reilly R, Warech M, Reilly S (1993) The influence of self-monitoring on the reliability and validity of upward feedback. Paper presented at: Annual Meeting of the Society for Industrial and Organizational Psychology, San Francisco
Hodges NJ, Franks IM (2002) Modelling coaching practice: the role of instruction and demonstration. J Sports Sci 20(10):793–811
Magill RA, Anderson D (2007) Motor learning and control: concepts and applications. vol 11, McGraw-Hill, New York
Lennox RD, Wolfe RN (1984) Revision of the self-monitoring scale. J Pers Soc Psychol 46(6):1349–1364
Available at: http://www.flsprogram.org. Accessed 23 Jan 2016
Korndorffer JR, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201(1):23–29
Heslin PA, VandeWalle D (2008) Managers’ implicit assumptions about personnel. Curr Dir Psychol Sci 17(3):219–223
Gregory JB, Levy PE (2010) Employee coaching relationships: enhancing construct clarity and measurement. Coaching 3(2):109–123
Bonrath EM, Dedy NJ, Gordon LE, Grantcharov TP (2015) Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg 262(2):205–212
Singh P, Aggarwal R, Tahir M, Pucher PH, Darzi A (2015) A randomized controlled study to evaluate the role of video-based coaching in training laparoscopic skills. Ann Surg 261(5):862–869
Hu Y-Y, Mazer LM, Yule SJ (2016) et al. Complementing operating room teaching with video-based coaching. JAMA Surg. https://doi.org/10.1001/jamasurg.2016.4619
Fitts PM, Posner MI (1967) Human performance. Brooks/Cole Publishing Company, Pacific Grove
O’Connor A, Schwaitzberg S, Cao C (2008) How much feedback is necessary for learning to suture? Surg Endosc 22(7):1614–1619
Francis DO, Eavey RD, Wright HV, Sinard RJ (2016) Incorporating postoperative debriefing into surgical education. J Surg Educ 73(3):448–452
Soucisse ML, Boulva K, Sideris L, Drolet P, Morin M, Dubé P (2016) Video coaching as an efficient teaching method for surgical residents—a randomized controlled trial. J Surg Educ 74(2):365–371
Hmelo-Silver CE, Duncan RG, Chinn CA (2006) Scaffolding and achievement in problem-based and inquiry learning: a response to Kirschner, Sweller, and Clark. Educ Psychol 42(2):99–107
Kirschner PA, Sweller J, Clark RE (2006) Why minimal guidance during instruction does not work: an analysis of the failure of constructivist, discovery, problem-based, experiential, and inquiry-based teaching. Educ Psychol 41(2):75–86
Reeve J, Tseng C-M (2011) Cortisol reactivity to a teacher’s motivating style: the biology of being controlled versus supporting autonomy. Motiv Emot 35(1):63–74
Hooyman A, Wulf G, Lewthwaite R (2014) Impacts of autonomy-supportive versus controlling instructional language on motor learning. Hum Mov Sci 36:190–198
Wulf G, McNevin N, Shea CH (2001) The automaticity of complex motor skill learning as a function of attentional focus. Quart J Exp Psychol 54(4):1143–1154
Zachry T, Wulf G, Mercer J, Bezodis N (2005) Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain Res Bull 67(4):304–309
Kal E, Van der Kamp J, Houdijk H (2013) External attentional focus enhances movement automatization: a comprehensive test of the constrained action hypothesis. Hum Mov Sci 32(4):527–539
Wulf G, Shea C, Lewthwaite R (2010) Motor skill learning and performance: a review of influential factors. Med Educ 44(1):75–84
Stein PK, Bosner MS, Kleiger RE, Conger BM (1994) Heart rate variability: a measure of cardiac autonomic tone. Am Heart J 127(5):1376–1381
Cardiology TFotESo (1996) Heart rate variability standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17:354–381
Salahuddin L, Cho J, Jeong MG, Kim D (2007) Ultra short term analysis of heart rate variability for monitoring mental stress in mobile settings. Paper presented at: Engineering in Medicine and Biology Society, 2007. EMBS 2007. 29th Annual International Conference of the IEEE
Gharbi A, Hey S, Jatoba L et al. (2008) System for body and mind monitoring in coaching process. Paper presented at: Medical Devices and Biosensors, 2008. ISSS-MDBS 2008. 5th International Summer School and Symposium on 2008
Schaaff K, Adam MT (2013) Measuring emotional arousal for online applications: evaluation of ultra-short term heart rate variability measures. Paper presented at: Affective Computing and Intelligent Interaction (ACII), Humaine Association Conference on 2013
Mayya S, Jilla V, Tiwari VN, Nayak MM, Narayanan R (2015) Continuous monitoring of stress on smartphone using heart rate variability. Paper presented at: Bioinformatics and Bioengineering (BIBE), IEEE 15th International Conference on 2015
Stanley J, D’Auria S, Buchheit M (2015) Cardiac parasympathetic activity and race performance: an elite triathlete case study. Int J Sports Physiol Perform 10(4):528–534
Buchheit M, Chivot A, Parouty J et al (2010) Monitoring endurance running performance using cardiac parasympathetic function. Eur J Appl Physiol 108(6):1153–1167
Yerkes RM, Dodson JD (1908) The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol 18(5):459–482
Leung Y, Salfinger S, Tan JJS, Frazer A (2013) The introduction and the validation of a surgical encounter template to facilitate surgical coaching of gynaecologists at a metropolitan tertiary obstetrics and gynaecology hospital. Aust NZ J Obstet Gynaecol 53(5):477–483
Connolly A, Hansen D, Schuler K, Galvin SL, Wolfe H (2014) Immediate surgical skills feedback in the operating room using “SurF” cards. J Grad Med Educ 6(4):774–778
Min H, Morales DR, Orgill D, Smink DS, Yule S (2015) Systematic review of coaching to enhance surgeons’ operative performance. Surgery 158(5):1168–1191
Shebilskem WL, Regian JW, Arthur W, Jordan JA (1992) A dyadic protocol for training complex skills. Hum Factors 34(3):369–374
Shea CH, Wright DL, Wulf G, Whitacre C (2000) Physical and observational practice afford unique learning opportunities. J Mot Behav 32(1):27–36
Sutkin G, Littleton EB, Kanter SL (2015) How surgical mentors teach: a classification of in vivo teaching behaviors part 1: verbal teaching guidance. J Surg Educ 72(2):243–250
Timberlake MD, Mayo HG, Scott L, Weis J, Gardner AK (2017) What do we know about intraoperative teaching?: a systematic review. Ann Surg 266:251–259
Gardner AK, Timberlake MD, Dunkin BD (2017) Faculty development for the operating room: Examining the impact of an intraoperative teaching course for surgeons. Ann Surg. https://doi.org/10.1097/SLA.0000000000002468
Acknowledgements
We thank Ibrahim I. Jabbour, MD for serving as the coach in this study.
Funding
The study was funded through a departmental educational research grant from the University of Texas Southwestern Department of Surgery to A.K.G.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Gardner has ownership interest in SurgWise Consulting, LLC. Dr. Timberlake, and Dr. Stefanidis has no relevant conflict of interest or financial ties to disclose.
Appendix
Appendix
Coaching quality evaluation
-
1.
My skills coach and I had mutual respect for one another.
-
2.
I believe my skills coach was committed to my training experience.
-
3.
My coach enabled me to develop my lap suturing skills.
-
4.
I felt able to discuss my concerns or troubles with my skills coach.
-
5.
My coach was a good listener.
-
6.
My coach helped me identify and build upon my strengths.
-
7.
My coach was effective at communicating with me.
-
8.
I felt at ease talking to my coach about my suturing performance.
-
9.
I felt safe being open and honest with my skills coach.
-
10.
I believe that my skills coach truly cared about my performance.
-
11.
My coach was easy to talk with.
-
12.
My coach engaged in effective techniques to help me unlock my lap suturing potential.
Rights and permissions
About this article
Cite this article
Timberlake, M.D., Stefanidis, D. & Gardner, A.K. Examining the impact of surgical coaching on trainee physiologic response and basic skill acquisition. Surg Endosc 32, 4183–4190 (2018). https://doi.org/10.1007/s00464-018-6163-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6163-7