Abstract
Background and aims
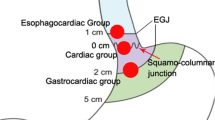
Most submucosal tumors (SMTs) in the esophagogastric junction (EGJ) are irregularly shaped and different from those in the esophagus, where submucosal tunneling endoscopic resection (STER) has been proven effective and safe. However, few reports paid attention to STER for SMTs in the EGJ. The aim of the study was not only to evaluate the effect of STER in patients with SMTs in the EGJ but to analyze the risk factors for failure of en bloc resection.
Methods
A consecutive of 47 patients with SMTs originating from the muscularis propria (MP) layer in the EGJ underwent STER were retrospectively included between September 2012 and December 2016. Thirty-five tumors underwent en bloc resection, and the other 12 tumors received piecemeal resection. The tumor size, operation time, en bloc resection rate, complications, residual, and local recurrence were achieved and compared between the two groups.
Results
Forty-six of 47 lesions (97.9%) were successfully resected. The mean lesion size was 29.7 ± 16.3 mm. Both the en bloc resection rate and complete resection rate were 74.5% (35/47). No severe complications occurred in the 47 patients. Patients in the piecemeal resection group had more irregularly shaped lesions, longer tumor diameter, larger tumor size (≥40 mm), longer operation time, and longer hospital stay after procedure (P < 0.05), and there were no statistically differences between the two groups in in-operative complications, post-operative complications, and residual rate (P > 0.05). By univariate analysis and stepwise logistic regression analysis, irregular shape and tumor diameter ≥20 mm were two risk factors for failure of en bloc resection.
Conclusions
STER is an effective and safe technique for the treatment of SMTs arising from the MP layer in the EGJ. Irregular shape and tumor diameter ≥20 mm are the reliable risk factors for en bloc resection failure.



Similar content being viewed by others
References
Demetri GD, von Mehren M, Antonescu CR, DeMatteo RP, Ganjoo KN, Maki RG, Pisters PW, Raut CP, Riedel RF, Schuetze S, Sundar HM, Trent JC, Wayne JD (2010) NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Cancer Netw 8(Supp 2):S1–41; quiz S42-44
Miettinen M, Sobin LH, Lasota J (2005) Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 29(1):52–68
Ponsaing LG, Kiss K, Hansen MB (2007) Classification of submucosal tumors in the gastrointestinal tract. World J Gastroenterol 13(24):3311–3315
He G, Wang J, Chen B, Xing X, Wang J, Chen J, He Y, Cui Y, Chen M (2016) Feasibility of endoscopic submucosal dissection for upper gastrointestinal submucosal tumors treatment and value of endoscopic ultrasonography in pre-operation assess and post-operation follow-up: a prospective study of 224 cases in a single medical center. Surg Endosc 30(10):4206–4213. doi:10.1007/s00464-015-4729-1
Hwang SH, Park DJ, Kim YH, Lee KH, Lee HS, Kim HH, Lee HJ, Yang HK, Lee KU (2009) Laparoscopic surgery for submucosal tumors located at the esophagogastric junction and the prepylorus. Surg Endosc 23(9):1980–1987. doi:10.1007/s00464-008-9955-3
Goh BK, Chow PK, Chok AY, Chan WH, Chung YF, Ong HS, Wong WK (2010) Impact of the introduction of laparoscopic wedge resection as a surgical option for suspected small/medium-sized gastrointestinal stromal tumors of the stomach on perioperative and oncologic outcomes. World J Surg 34(8):1847–1852. doi:10.1007/s00268-010-0590-5
Milone M, Elmore U, Musella M, Parise P, Zotti MC, Bracale U, Di Lauro K, Manigrasso M, Milone F, Rosati R (2017) Safety and efficacy of laparoscopic wedge gastrectomy for large gastrointestinal stromal tumors. Eur J Surg Oncol 43(4):796–800. doi:10.1016/j.ejso.2017.01.005
Khoo CY, Goh BKP, Eng AKH, Chan WH, Teo MCC, Chung AYF, Ong HS, Wong WK (2017) Laparoscopic wedge resection for suspected large (>/=5 cm) gastric gastrointestinal stromal tumors. Surg Endosc 31(5):2271–2279. doi:10.1007/s00464-016-5229-7
Reinehr R (2015) Endoscopic submucosal excavation (ESE) is a safe and useful technique for endoscopic removal of submucosal tumors of the stomach and the esophagus in selected cases. Z Gastroenterol 53(6):573–578. doi:10.1055/s-0034-1399384
Zhou PH, Yao LQ, Qin XY, Cai MY, Xu MD, Zhong YS, Chen WF, Zhang YQ, Qin WZ, Hu JW, Liu JZ (2011) Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surg Endosc 25(9):2926–2931. doi:10.1007/s00464-011-1644-y
Stavropoulos SN, Modayil R, Friedel D, Brathwaite CE (2014) Endoscopic full-thickness resection for GI stromal tumors. Gastrointest Endosc 80(2):334–335. doi:10.1016/j.gie.2014.05.300
Lu J, Lu X, Jiao T, Zheng M (2014) Endoscopic management of upper gastrointestinal submucosal tumors arising from muscularis propria. J Clin Gastroenterol 48(8):667–673. doi:10.1097/mcg.0000000000000135
Wang XY, Xu MD, Yao LQ, Zhou PH, Pleskow D, Li QL, Zhang YQ, Chen WF, Zhong YS (2014) Submucosal tunneling endoscopic resection for submucosal tumors of the esophagogastric junction originating from the muscularis propria layer: a feasibility study (with videos). Surg Endosc 28(6):1971–1977. doi:10.1007/s00464-014-3420-2
Linghu EQZY (2011) Experimental study on resection of the esophageal muscular propria layer by endoscopic tunnel technique. Chin J Laparosc Surg 4(5):293–392
Xu MD, Cai MY, Zhou PH, Qin XY, Zhong YS, Chen WF, Hu JW, Zhang YQ, Ma LL, Qin WZ, Yao LQ (2012) Submucosal tunneling endoscopic resection: a new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos). Gastrointest Endosc 75(1):195–199. doi:10.1016/j.gie.2011.08.018
Xiong Y, Hu H, Gao Y, Linghu E, Wang X, Wang A (2014) Endoscopic esophageal submucosal tunnel resection of cardiac benign tumors originating from muscularis propria. Zhonghua yi xue za zhi 94(46):3655–3657
Zhou DJ, Dai ZB, Wells MM, Yu DL, Zhang J, Zhang L (2015) Submucosal tunneling and endoscopic resection of submucosal tumors at the esophagogastric junction. World J Gastroenterol 21(2):578–583. doi:10.3748/wjg.v21.i2.578
Mao XL, Ye LP, Zheng HH, Zhou XB, Zhu LH, Zhang Y (2016) Submucosal tunneling endoscopic resection using methylene-blue guidance for cardial subepithelial tumors originating from the muscularis propria layer. Dis Esophagus. doi:10.1111/dote.12536
Stein HJ, Feith M, Siewert JR (2000) Cancer of the esophagogastric junction. Surg Oncol 9(1):35–41
Lv XH, Wang CH, Xie Y (2017) Efficacy and safety of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors: a systematic review and meta-analysis. Surg Endosc 31(1):49–63. doi:10.1007/s00464-016-4978-7
Li ZS, Li Q (2011) [The latest 2010 WHO classification of tumors of digestive system]. Zhonghua bing li xue za zhi. Chin J Pathol 40(5):351–354
Wang L, Ren W, Zhang Z, Yu J, Li Y, Song Y (2013) Retrospective study of endoscopic submucosal tunnel dissection (ESTD) for surgical resection of esophageal leiomyoma. Surg Endosc 27(11):4259–4266. doi:10.1007/s00464-013-3035-z
Ye LP, Zhang Y, Mao XL, Zhu LH, Zhou X, Chen JY (2014) Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg Endosc 28(2):524–530. doi:10.1007/s00464-013-3197-8
Zhang C, Hu JW, Chen T, Zhou PH, Zhong YS, Zhang YQ, Chen WF, Li QL, Yao LQ, Xu MD (2015) Submucosal tunneling endoscopic resection for upper gastrointestinal multiple submucosal tumors originating from the muscular propria layer: a feasibility study. Indian J Cancer 51(Suppl 2):e52–e55. doi:10.4103/0019-509x.151989
Liebermann-Meffert D, Allgower M, Schmid P, Blum AL (1979) Muscular equivalent of the lower esophageal sphincter. Gastroenterology 76(1):31–38
Stein HJ, Liebermann-Meffert D, DeMeester TR, Siewert JR (1995) Three-dimensional pressure image and muscular structure of the human lower esophageal sphincter. Surgery 117(6):692–698
Vegesna AK, Sloan JA, Singh B, Phillips SJ, Braverman AS, Barbe MF, Ruggieri MR Sr, Miller LS (2013) Characterization of the distal esophagus high-pressure zone with manometry, ultrasound and micro-computed tomography. Neurogastroenterol Motil 25(1):53–60. doi:10.1111/nmo.12010
Lerche W (1936) The muscular coat of the esophagus and its defects. J Thorac Surg 6(1):1–19
Linghu E (2013) Therapeutics of digestive endoscopic tunnel technique. Springer, Berlin
Li B, Liu J, Lu Y, Hao J, Liu H, Jiang J, Jiang Y, Qin C, Xu H (2016) Submucosal tunneling endoscopic resection for tumors of the esophagogastric junction. Minim Invasive Ther Allied Technol 25(3):141–147. doi:10.3109/13645706.2016.1167085
Zhao H, Sheng H, Huang L, Jiang L, Xie Y, Zhou P (2015) [Submucosal tunneling endoscopic resection in the treatment of esophageal submucosal tumors originating from muscularis propria layer]. Zhonghua wei chang wai ke za zhi = Chinese. J Gastrointest Surg 18(5):478–482
Chen T, Zhang C, Yao LQ, Zhou PH, Zhong YS, Zhang YQ, Chen WF, Li QL, Cai MY, Chu Y, Xu MD (2016) Management of the complications of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors. Endoscopy 48(2):149–155. doi:10.1055/s-0034-1393244
Acknowledgement
This study was supported by research grants from two Chinese People’s Liberation Army General Hospital Clinical Researches (2012FC-TSYS-3035 and YS201404).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Zhenjuan Li, Ying Gao, Ningli Chai, Ying Xiong, Lianjun Ma, Wengang Zhang, Chen Du and Enqiang Linghu have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Li, Z., Gao, Y., Chai, N. et al. Effect of submucosal tunneling endoscopic resection for submucosal tumors at esophagogastric junction and risk factors for failure of en bloc resection. Surg Endosc 32, 1326–1335 (2018). https://doi.org/10.1007/s00464-017-5810-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5810-8