Abstract
Introduction
The incidence of incisional hernia(IH) may be affected by the choice of specimen extraction incision. The objective of this study was to perform a systematic review and meta-analysis comparing the incidence of IH after midline and off-midline incisions in patients undergoing laparoscopic colorectal surgery.
Methods
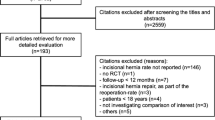
A systematic search was performed according to PRISMA guidelines to identify all comparative studies from January 1991–August 2016 on the incidence of IH after midline and off-midline(transverse or Pfannenstiel) incisions in patients undergoing laparoscopic colorectal surgery. Case series and studies reporting the IH after stoma site extraction, SILS, or NOTES were excluded. The MINORS instrument was used for quality assessment for observational studies. Weighted estimates were calculated using a random-effects model.
Results
A total of 17 articles were identified and included for meta-analysis, 16 of which were observational studies and 1 was an RCT. The mean MINORS score for observational studies was 12.9 (SD 3.2, range 7–17). Sample sizes in the midline (mean 185, range 20–995) and off-midline(mean 184, range 20–903) groups were similar. Follow-up ranged from 17.3 to 42 months. The pooled incidence of IH was 10.6% (338/3177) in midline, 3.7% (48/1314) in transverse, and 0.9% (9/956) in Pfannenstiel incisions. IH was significantly higher in the midline compared to off-midline groups (weighted OR 4.1, 95% CI 2.0–8.3, I 2 = 79.7%, p for heterogeneity <0.001). Midline incisions were also at higher risk of IH versus transverse (weighted OR 3.0, 95% CI 1.4–6.7, I 2 = 72.7%, p for heterogeneity <0.001) and Pfannenstiel (weighted OR 8.6, 95% CI 3.0–24.6, I 2 = 43.5%, p for heterogeneity = 0.101) incisions. There was no publication bias according the funnel plot or statistically (Egger’s p = 0.336).
Conclusions
Midline incisions for specimen extraction in laparoscopic colorectal surgery are at significantly higher risk of IH compared to off-midline (transverse or Pfannenstiel) incisions, but these data are of poor quality and heterogeneous.





Similar content being viewed by others
References
van Ramshorst GH, Eker HH, Hop WC, Jeekel J, Lange JF (2012) Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg 204:144–150
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642
Funk LM, Perry KA, Narula VK, Mikami DJ, Melvin WS (2013) Current national practice patterns for inpatient management of ventral abdominal wall hernia in the United States. Surg Endosc 27:4104–4112
Reynolds D, Davenport DL, Korosec RL, Roth JS (2013) Financial implications of ventral hernia repair: a hospital cost analysis. J Gastrointest Surg 17:159–166 discussion p 166–157
Kossler-Ebs JB, Grummich K, Jensen K, Huttner FJ, Muller-Stich B, Seiler CM, Knebel P, Buchler MW, Diener MK (2016) Incisional hernia rates after laparoscopic or open abdominal surgery—a systematic review and meta-analysis. World J Surg 40(10):2319–2330
Pecorelli N, Greco M, Amodeo S, Braga M (2016) Small bowel obstruction and incisional hernia after laparoscopic and open colorectal surgery: a meta-analysis of comparative trials. Surg Endosc 31(1):85–99
Sajid MS, Bhatti MI, Sains P, Baig MK (2014) Specimen retrieval approaches in patients undergoing laparoscopic colorectal resections: a literature-based review of published studies. Gastroenterol Rep (Oxf) 2:251–261
Benlice C, Stocchi L, Costedio MM, Gorgun E, Kessler H (2016) Impact of the specific extraction-site location on the risk of incisional hernia after laparoscopic colorectal resection. Dis Colon Rectum 59:743–750
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, Fried GM, Feldman LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26:3180–3185
Halm JA, Lip H, Schmitz PI, Jeekel J (2009) Incisional hernia after upper abdominal surgery: a randomised controlled trial of midline versus transverse incision. Hernia 13:275–280
Fassiadis N, Roidl M, Hennig M, South LM, Andrews SM (2005) Randomized clinical trial of vertical or transverse laparotomy for abdominal aortic aneurysm repair. Br J Surg 92:1208–1211
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Riley RD, Higgins JP, Deeks JJ (2011) Interpretation of random effects meta-analyses. Bmj 342:d549
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 295:676–680
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, Fried GM, Feldman LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26:3180–3185
Lim SW, Huh JW, Kim YJ, Kim HR (2013) Vertical transumbilical incision versus left lower transverse incision for specimen retrieval during laparoscopic colorectal surgery. Tech Coloproctol 17:59–65
Tan WS, Chew MH, Ho KS, Yatim JB, Lai JS, Tang CL (2015) Short and long-term outcomes of a randomised controlled trial of vertical periumbilical wound versus transverse left iliac fossa wound for specimen retrieval in laparoscopic anterior resections. Surg Endosc 29:2720–2727
Harr JN, Juo YY, Luka S, Agarwal S, Brody F, Obias V (2016) Incisional and port-site hernias following robotic colorectal surgery. Surg Endosc 30:3505–3510
Pares D, Shamali A, Stefan S, Flashman K, O’Leary D, Conti J, Senapati A, Parvaiz A, Khan J (2016) Predictive factors for extraction site hernia after laparoscopic right colectomy. Int J Colorectal Dis 31:1323–1328
Sadava EE, Kerman Cabo J, Galvan MA, Grzona EG, Canelas AG, Bun ME, Rotholtz NA (2015) Incisional hernia after laparoscopic colorectal surgery is there any factor associated? Surg Endosc 29:S79
Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D (2016) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short- and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 30:3823–3829
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
DeSouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H (2011) Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 25:1031–1036
Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, Leitman IM (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 200:265–269
Morita Y, Yamaguchi S, Ishii T, Tashiro J, Kondo H, Suzuki A, Hara K, Koyama I (2015) Does transumbilical incision increase incisional hernia at the extraction site of laparoscopic anterior resection? Am J Surg 209:1048–1052
Campagnacci R, Baldoni A, Ghiselli R, Cappelletti-Trombettoni MM, Guerrieri M (2015) Prevention of hernia incision in laparoscopic left colon resection. Minerva Chir 70:155–160
Navaratnam AV, Ariyaratnam R, Smart NJ, Parker M, Motson RW, Arulampalam TH (2015) Incisional hernia rate after laparoscopic colorectal resection is reduced with standardisation of specimen extraction. Ann R Coll Surg Engl 97:17–21
Samia H, Lawrence J, Nobel T, Stein S, Champagne BJ, Delaney CP (2013) Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg 205:264–267
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA (1998) Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc 12:1334–1340
Hollander JE, Singer AJ, Valentine S, Henry MC (1995) Wound registry: development and validation. Ann Emerg Med 25:675–685
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Seiler CM, Deckert A, Diener MK, Knaebel HP, Weigand MA, Victor N, Buchler MW (2009) Midline versus transverse incision in major abdominal surgery: a randomized, double-blind equivalence trial (POVATI: ISRCTN60734227). Ann Surg 249:913–920
Millbourn D, Cengiz Y, Israelsson LA (2009) Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg 144:1056–1059
Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, van Doorn HC, Heisterkamp J, Wijnhoven BP, Schouten WR, Cense HA, Stockmann HB, Berends FJ, Dijkhuizen FP, Dwarkasing RS, Jairam AP, van Ramshorst GH, Kleinrensink GJ, Jeekel J, Lange JF (2015) Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet 386:1254–1260
Millbourn D, Cengiz Y, Israelsson LA (2011) Risk factors for wound complications in midline abdominal incisions related to the size of stitches. Hernia 15:261–266
Israelsson LA, Jonsson T (1993) Suture length to wound length ratio and healing of midline laparotomy incisions. Br J Surg 80:1284–1286
Muysoms FE, Antoniou SA, Bury K, Campanelli G, Conze J, Cuccurullo D, de Beaux AC, Deerenberg EB, East B, Fortelny RH, Gillion JF, Henriksen NA, Israelsson L, Jairam A, Janes A, Jeekel J, Lopez-Cano M, Miserez M, Morales-Conde S, Sanders DL, Simons MP, Smietanski M, Venclauskas L, Berrevoet F, European Hernia S (2015) European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia 19:1–24
Rahbari NN, Knebel P, Diener MK, Seidlmayer C, Ridwelski K, Stoltzing H, Seiler CM (2009) Current practice of abdominal wall closure in elective surgery—is there any consensus? BMC Surg 9:8
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev
Murray BW, Cipher DJ, Pham T, Anthony T (2011) The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg 202:558–560
Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, Kono H, Yamamoto H, Ando M, Nagino M (2014) Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg 101:1439–1447
Israelsson LA, Jonsson T (1996) Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 162:125–129
Fink C, Baumann P, Wente MN, Knebel P, Bruckner T, Ulrich A, Werner J, Buchler MW, Diener MK (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101:51–54
Hoer J, Lawong G, Klinge U, Schumpelick V (2002) Factors influencing the development of incisional hernia. A retrospective study of 2983 laparotomy patients over a period of 10 years. Chirurg 73:474–480
Baucom RB, Beck WC, Holzman MD, Sharp KW, Nealon WH, Poulose BK (2014) Prospective evaluation of surgeon physical examination for detection of incisional hernias. J Am Coll Surg 218:363–366
Naguib N, Rafique H, Dhruva Rao PK, Longworth T, Soukias JM, Masoud A (2015) A review of the incidence of iatrogenic hernia in both laparoscopic and open colorectal surgery: using CT as the gold standard of detection, cohort study. Int J Surg 19:87–90
Bloemen A, van Dooren P, Huizinga BF, Hoofwijk AG (2012) Comparison of ultrasonography and physical examination in the diagnosis of incisional hernia in a prospective study. Hernia 16:53–57
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583 discussion 583–575
Rogmark P, Petersson U, Bringman S, Ezra E, Osterberg J, Montgomery A (2016) Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair: PROLOVE: a randomized controlled trial. Ann Surg 263:244–250
Marchesi F, Pinna F, Percalli L, Cecchini S, Ricco M, Costi R, Pattonieri V, Roncoroni L (2013) Totally laparoscopic right colectomy: theoretical and practical advantages over the laparo-assisted approach. J Laparoendosc Adv Surg Tech A 23:418–424
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J (2008) Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg 143:762–767 discussion 768
Bartels SA, Vlug MS, Hollmann MW, Dijkgraaf MG, Ubbink DT, Cense HA, van Wagensveld BA, Engel AF, Gerhards MF, Bemelman WA, Collaborative LSG (2014) Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br J Surg 101:1153–1159
Aquina CT, Rickles AS, Probst CP, Kelly KN, Deeb AP, Monson JRT, Fleming FJ, Marc (2015) Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon Rectum 58:220–227
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Feldman reports Grant support from Covidien. Dr. Liberman reports consultant’s fees from Merck. Drs. Lee, Abou-Khalil, Boutros, and Fried have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lee, L., Abou-Khalil, M., Liberman, S. et al. Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: systematic review and meta-analysis. Surg Endosc 31, 5083–5093 (2017). https://doi.org/10.1007/s00464-017-5573-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5573-2