Abstract
Introduction
Complicated ventral hernias are often referred to tertiary care centers. Hospital costs associated with these repairs include direct costs (mesh materials, supplies, and nonsurgeon labor costs) and indirect costs (facility fees, equipment depreciation, and unallocated labor). Operative supplies represent a significant component of direct costs, especially in an era of proprietary synthetic meshes and biologic grafts. We aim to evaluate the cost-effectiveness of complex abdominal wall hernia repair at a tertiary care referral facility.
Methods
Cost data on all consecutive open ventral hernia repairs (CPT codes 49560, 49561, 49565, and 49566) performed between 1 July 2008 and 31 May 2011 were analyzed. Cases were analyzed based upon hospital status (inpatient vs. outpatient) and whether the hernia repair was a primary or secondary procedure. We examined median net revenue, direct costs, contribution margin, indirect costs, and net profit/loss. Among primary hernia repairs, cost data were further analyzed based upon mesh utilization (no mesh, synthetic, or biologic).
Results
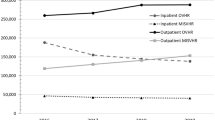
Four-hundred and fifteen patients underwent ventral hernia repair (353 inpatients and 62 outpatients); 173 inpatients underwent ventral hernia repair as the primary procedure; 180 inpatients underwent hernia repair as a secondary procedure. Median net revenue ($17,310 vs. 10,360, p < 0.001) and net losses (3,430 vs. 1,700, p < 0.025) were significantly greater for those who underwent hernia repair as a secondary procedure. Among inpatients undergoing ventral hernia repair as the primary procedure, 46 were repaired without mesh; 79 were repaired with synthetic mesh and 48 with biologic mesh. Median direct costs for cases performed without mesh were $5,432; median direct costs for those using synthetic and biologic mesh were $7,590 and 16,970, respectively (p < .01). Median net losses for repairs without mesh were $500. Median net profit of $60 was observed for synthetic mesh-based repairs. The median contribution margin for cases utilizing biologic mesh was −$4,560, and the median net financial loss was $8,370. Outpatient ventral hernia repairs, with and without synthetic mesh, resulted in median net losses of $1,560 and 230, respectively.
Conclusions
Ventral hernia repair is associated with overall financial losses. Inpatient synthetic mesh repairs are essentially budget neutral. Outpatient and inpatient repairs without mesh result in net financial losses. Inpatient biologic mesh repairs result in a negative contribution margin and striking net financial losses. Cost-effective strategies for managing ventral hernias in a tertiary care environment need to be developed in light of the financial implications of this patient population.




Similar content being viewed by others
References
Wechter ME, Pearlman MD, Hartmann KE. Reclosure of the disrupted laparotomy wound; a systematic review. Obstet Gynecol 2005;106:376–383.
Mudge M, Hughes LE. Incisional hernia: a 10-year prospective study of incidence and attitudes. Br J Surg 1985;72:70–71.
Cengiz Y, Israelsson LA. Incisional hernias in midline incisions: an eight-year follow up. Hernia 1998;2:175–177.
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 2004;240:578–583.
Flum DR, Horvath K, Koepsell T. Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 2003;237:129–135.
Poulose, BK, Shelton J, Phillips S, Moore D, Nealon W, Penson D, Beck W, Holzman MD. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 2012;16:179–183.
Davenport DL, Henderson WG, Khuri SF, Mentzer RM Jr. Preoperative risk factors and surgical complexity are more predictive of costs than postoperative complications: a case study using the National Surgical Quality Improvement Program (NSQIP) Database. Ann Surg 2005;242:463–468.
Albright EL, Davenport Dl, Roth JS. Preoperative functional health status impacts outcomes after ventral hernia repair. Am Surg.2012;78:230–234.
Earle D, Seymour N, Fellinger E, Perez A. Laparoscopic versus open incisional hernia repair: a single institution analysis of hospital resource utilization for 884 consecutive cases. Surg Endosc 2006;20:71–75.
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, Ijzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J. A comparison of suture repair with mesh repair for incisional hernia. N Eng J Med 2000;343:392–398.
Finan KR, Kilgore ML, Hawn MT. Open suture versus mesh repair of primary incisional hernias: a cost-utility analysis. Hernia 2009;13:173–182.
Israelsson LA, Jönsson L, Wimo A. Cost analysis of incisional hernia repair by suture or mesh. Hernia 2003;7:114–117.
Harth C, Rose J, Delaney CP, Blatnik JA, Halaweish I, Rosen MJ. Open versus endoscopic component separation: a cost comparison. Surg Endosc 2011;25:2865–2870.
Kelly ME, Behrman SW. The safety and efficacy of prosthetic hernia repair in clean-contaminated and contaminated wounds. Am Surg 2002;68:524–528.
Rosen MJ. Biologic mesh for abdominal wall reconstruction: a critical appraisal. Am Surg 2010;76:1–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Daniel J. Deziel (Chicago,IL): Dr. Reynolds and colleagues have painted a discouraging financial profile for ventral hernia repair which would become even more grim if the cost of readmissions was added. Related readmissions yield, at best, only commodity level returns and are not in the financial core. Two primary drivers of direct cost were use of mesh, particularly biologic mesh, and length of stay. Perhaps you could clarify whether the mesh cost figures were actual institutional costs or patient charges. Since there is no consensus on the specific value of various biologics, have you done anything to standardize use of these expensive products? With the exception of biologic mesh, all hernia repair categories would have been money makers before indirect costs. Indirect costs are allocated differently at different medical centers and within medical centers. Your indirect costs ranged up to 58 % of direct cost and up to nearly 800 % of OR supply cost (from tables in manuscript). Is an excess of overhead being misallocated to these patients?
Thank you for the privilege of discussion.
Closing Discussant
Dr. Drew Reynolds: Thank you, Dr. Deziel, for your comments and thoughtful critique of our manuscript. To begin with, I wholeheartedly agree with your assessment of the bleak financial picture. I believe it is appropriate to assume that if the cost of readmissions were included, the financial picture would be even more dismal. Analysis of cost data related to readmissions is an area of further investigation for our group. Biologic mesh materials were a significant driver of cost in this analysis. To answer your question, we used actual hospital costs and did not evaluate hospital charges, as these numbers are often inflated and individual insurance contracts result in different negotiated rates. Additionally, in an era of DRG-based hospital reimbursement, actual hospital charges are frequently irrelevant as reimbursements are based upon contractual agreements for the vast majority of patients. With respect to standardization of mesh use, as of 2009, a contractual agreement was made with one company (BARD). And most of the meshes used at our facility are their products. And we only use biologic grafts for ventral hernia when we feel that a synthetic is contraindicated. Indirect costs include overhead depreciation, enterprise transfers, goods and services, and personnel, and are based on direct costs. We agree that contribution margin is a more relevant number in looking at these finances, but hospitals still need to cover indirect costs to remain fiscally solvent. With the help of our finance staff, we have investigated the methodology associated with assigning these indirect costs to each patient and feel that in fact the calculations are appropriate.
Based upon selection, this manuscript was presented as an oral presentation at Digestive Disease Week 2012 in San Diego, California
Rights and permissions
About this article
Cite this article
Reynolds, D., Davenport, D.L., Korosec, R.L. et al. Financial Implications of Ventral Hernia Repair: A Hospital Cost Analysis. J Gastrointest Surg 17, 159–167 (2013). https://doi.org/10.1007/s11605-012-1999-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-1999-y