Abstract
Background
This observational study was conducted to compare the rate of symptomatic anastomotic leakage (AL), as defined by precise criteria, between laparoscopic and open surgery in patients with mid-to-low rectal cancer using a relatively novel statistical technique.
Methods
A total of 1014 consecutive low anterior resection (LAR) patients were registered, of whom 936 were included in this prospective, multicenter, and cohort study (UMIN-CTR, Number 000004017). Patients with rectal cancer within 10 cm from the anal verge underwent either open or laparoscopic LAR at one of the 40 institutions in Japan from June 2010 to February 2013. The primary endpoint of this study was to compare the rate of symptomatic AL between the two groups before and after propensity score matching (PSM). The secondary endpoint was to analyze the risk factors for symptomatic AL in open and laparoscopic surgery.
Results
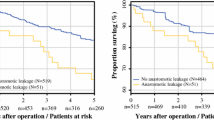
After PSM, the incidence of symptomatic AL in open and laparoscopic surgery was 12.4 and 15.3 %, respectively (p = 0.48). AL requiring relaparotomy occurred after 3.8 % of open surgeries and 6.2 % of laparoscopic surgeries (p = 0.37). Multivariate analysis identified male gender as an independent risk factor for symptomatic AL following laparoscopic surgery (p = 0.001; odds ratio 5.2; 95 % CI 2.0–13.8), and male gender (p = 0.004; odds ratio 2.6; 95 % CI 1.3–5.6), tumor size (p = 0.002; odds ratio 1.2; 95 % CI 0.7–0.9), and number of stapler firing (p = 0.04; odds ratio 4.1; 95 % CI 1.0–15.0) following open surgery.
Conclusion
The rate of symptomatic AL was comparable following laparoscopic and open LAR in this large, multicenter, cohort study after PSM. Male gender was associated with an increased risk of symptomatic AL after laparoscopic LAR.
Similar content being viewed by others
References
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ, Group COcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Yeh CY, Changchien CR, Wang JY, Chen JS, Chen HH, Chiang JM, Tang R (2005) Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg 241:9–13
den Dulk M, Marijnen CA, Collette L, Putter H, Pahlman L, Folkesson J, Bosset JF, Rodel C, Bujko K, van de Velde CJ (2009) Multicentre analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery. Br J Surg 96:1066–1075
Matthiessen P, Hallbook O, Andersson M, Rutegard J, Sjodahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis 6:462–469
Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T, Rutten HJ, van de Velde CJ, Dutch Colorectal Cancer G (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92:211–216
Kingham TP, Pachter HL (2009) Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am Coll Surg 208:269–278
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS, Chang HJ, Lee HS, Kim SY, Jung KH, Hong YS, Kim JH, Sohn DK, Kim DH, Oh JH (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
Arezzo A, Passera R, Scozzari G, Verra M, Morino M (2013) Laparoscopy for rectal cancer reduces short-term mortality and morbidity: results of a systematic review and meta-analysis. Surg Endosc 27:1485–1502
Aziz O, Constantinides V, Tekkis PP, Athanasiou T, Purkayastha S, Paraskeva P, Darzi AW, Heriot AG (2006) Laparoscopic versus open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol 13:413–424
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Buchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
Lunt M (2014) Selecting an appropriate caliper can be essential for achieving good balance with propensity score matching. Am J Epidemiol 179:226–235
Murakawa T, Ichinose J, Hino H, Kitano K, Konoeda C, Nakajima J (2015) Long-term outcomes of open and video-assisted thoracoscopic lung lobectomy for the treatment of early stage non-small cell lung cancer are similar: a propensity-matched study. World J Surg 39:1084–1091
Quan ML, Osman F, McCready D, Fernandes K, Sutradhar R, Paszat L (2014) Postmastectomy radiation and recurrence patterns in breast cancer patients younger than age 35 years: a population-based cohort. Ann Surg Oncol 21:395–400
Rodrigues G, Zindler J, Warner A, Bauman G, Senan S, Lagerwaard F (2013) Propensity-score matched pair comparison of whole brain with simultaneous in-field boost radiotherapy and stereotactic radiosurgery. Radiother Oncol 106:206–209
Hasegawa H, Okabayashi K, Watanabe M, Ashrafian H, Harling L, Ishii Y, Sugiyama D, Seishima R, Darzi A, Athanasiou T, Kitagawa Y (2014) What is the effect of laparoscopic colectomy on pattern of colon cancer recurrence? A propensity score and competing risk analysis compared with open colectomy. Ann Surg Oncol 21:2627–2635
Odermatt M, Miskovic D, Siddiqi N, Khan J, Parvaiz A (2013) Short- and long-term outcomes after laparoscopic versus open emergency resection for colon cancer: an observational propensity score-matched study. World J Surg 37:2458–2467
Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, Kang SB, Kim JY, Lee KY, Kim BC, Bae BN, Son GM, Lee SI, Kang H (2013) Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg 257:665–671
Kawada K, Hasegawa S, Hida K, Hirai K, Okoshi K, Nomura A, Kawamura J, Nagayama S, Sakai Y (2014) Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis. Surg Endosc 28:2988–2995
Kim JH, Kim HY, Lee IK, Oh ST, Kim JG, Lee YS (2014) Intra-operative double-stapled colorectal or coloanal anastomotic complications of laparoscopic low anterior resection for rectal cancer: double-stapled anastomotic complication could result in persistent anastomotic leakage. Surg Endosc. doi:10.1007/s00464-014-4035-3
Lee WS, Yun SH, Roh YN, Yun HR, Lee WY, Cho YB, Chun HK (2008) Risk factors and clinical outcome for anastomotic leakage after total mesorectal excision for rectal cancer. World J Surg 32:1124–1129
Jung SH, Yu CS, Choi PW, Kim DD, Park IJ, Kim HC, Kim JC (2008) Risk factors and oncologic impact of anastomotic leakage after rectal cancer surgery. Dis Colon Rectum 51:902–908
Shiomi A, Ito M, Maeda K, Kinugasa Y, Ota M, Yamaue H, Shiozawa M, Horie H, Kuriu Y, Saito N (2015) Effects of a diverting stoma on symptomatic anastomotic leakage after low anterior resection for rectal cancer: a propensity score matching analysis of 1,014 consecutive patients. J Am Coll Surg 220:186–194
Ito M, Sugito M, Kobayashi A, Nishizawa Y, Tsunoda Y, Saito N (2008) Relationship between multiple numbers of stapler firings during rectal division and anastomotic leakage after laparoscopic rectal resection. Int J Colorectal Dis 23:703–707
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishiguro M, Kanamitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Takiuchi H, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K, Japanese Society for Cancer of the Colon and Rectum (2012) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol 17:1–29
Acknowledgments
This study was supported by the Japanese Society for Cancer of the Colon and Rectum. Presented here is a list of the participating surgeons and centers: T. Morita (Aomori Prefectural Central Hospital, Aomori), H. Bando (Ishikawa Prefectural Central Hospital, Ishikawa), J. Okuda (Osaka Medical College Hospital, Osaka), K. Otsuka (Iwate Medical University School of Medicine, Iwate), A. Kanazawa (Japanese Red Cross Osaka Hospital, Osaka), M. Ueno (Cancer Institute Hospital, Tokyo), M. Shiozawa (Kanagawa Cancer Center, Kanagawa), M. Watanabe (Kitasato University Hospital, Kanagawa), T. Masaki (Kyorin University Hospital, Tokyo), Y. Sakai (Kyoto University Hospital, Kyoto), E. Otsuji (Kyoto Prefectural University of Medicine, Kyoto), K. Shirouzu (Kurume University Hospital, Fukuoka), T. Kusumi (Keiyukai Sapporo Hospital, Hokkaido), Y. Kinugasa (Shizuoka Cancer Center Hospital, Shizuoka), M. Morita (National Hospital Organization Kyushu Cancer Center, Fukuoka), Y. Kubo (National Hospital Organization Shikoku Cancer Center, Ehime), H. Ike (Saiseikai Nanbu Hospital, Kanagawa), H. Masuko (Sapporo-Kosei General Hospital, Hokkaido), N. Takiguchi (Chiba Cancer Center, Chiba), H. Horie (Jichi Medical University, Tochigi), K. Sugihara (Tokyo Medical and Dental University, Tokyo), S. Kameoka (Tokyo Women’s Medical University Hospital, Tokyo), Y. Takii (Niigata Cancer Center Hospital, Niigata), F. Itani (Fukuyama City Hospital, Hiroshima), N. Tomita (Hyogo College of Medicine, Hyogo), M. Okajima (Hiroshima City Asa Hospital, Hiroshima), T. Sato (Yamagata Prefectural Central Hospital, Yamagata), S. Osada (Yokohama City Minato Red Cross Hospital, Kanagawa), M. Ohue (Osaka Medical Center for Cancer and Cardiovascular Disease, Osaka), S. Fujii (Yokohama City University Medical Center, Kanagawa), H. Yamaue (Wakayama Medical University, Wakayama), and M. Hamada (Kochi Health Sciences Center, Kochi). The authors thank Keita Mori of the Biostatistics Collaboration Unit, Shizuoka Cancer Center, Japan, for his help with statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Hidetoshi Katsuno, Akio Shiomi, Masaaki Ito, Yoshikazu Koide, Koutarou Maeda, Toshimasa Yatsuoka, Kazuo Hase, Koji Komori, Kazuhito Minami, Kazuhiro Sakamoto, Yoshihisa Saida, and Norio Saito have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Katsuno, H., Shiomi, A., Ito, M. et al. Comparison of symptomatic anastomotic leakage following laparoscopic and open low anterior resection for rectal cancer: a propensity score matching analysis of 1014 consecutive patients. Surg Endosc 30, 2848–2856 (2016). https://doi.org/10.1007/s00464-015-4566-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4566-2