Abstract
Background
Cystogastrostomy is commonly performed for internal drainage of pancreatic pseudocysts (PP) and concomitant debridement of walled-off pancreatic necrosis (WOPN). While an open approach to cystogastrostomy is well established, an optimal minimally invasive technique continues to evolve. This laparoscopic transgastric endolumenal cystogastrostomy presented here allows for a large cystogastrostomy with complete debridement of necrosis and internal drainage through a minimally invasive approach.
Methods
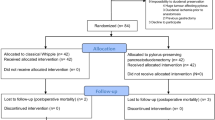
We performed a retrospective review of 22 patients with symptomatic PP/WOPN treated with attempted laparoscopic transgastric endolumenal cystogastrostomy (Lap-TEC) and pancreatic debridement. Short- and long-term outcomes were assessed.
Results
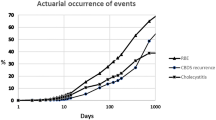
From November 2006 to March 2013, a total of 22 Lap-TEC/pancreatic debridement procedures were attempted; 15 were completed laparoscopically. The median age of the cohort was 49.5 ± 12 years (range = 18–71), average body mass index = 29.1 kg/m2, 77 % had an ASA score ≥3, and 10 were female. Gallstones were the most common etiology (50 %), and median time between initial presentation and surgery was 86 days (range = 0–360). Median operative time and estimated blood loss were 213 min and 100 cc, respectively. Forty-one percent of the patients were admitted to the ICU postoperatively and the average length of stay was 14 days (range = 4–50). Median follow-up was 2 months (range = 0–62.5), with one patient having a procedure-related complication. No other reoperations, late complications, or mortalities occurred. All patients had resolution of their symptoms and fluid collections.
Conclusion
This technique of internal drainage via Lap-TEC and pancreatic debridement has been successful in achieving primary drainage and relieving symptoms of PP/WOPN with no mortality and minimal morbidity.
Similar content being viewed by others
Pancreatic pseudocysts (PP) are a complication of acute (2–10 %) or chronic pancreatitis (10–30 %) and require intervention based on symptoms, growing size (>6 cm), persistence (>6 weeks), and complexity [1–4]. Post-necrotic PP have also been referred to as walled-off pancreatic necrosis (WOPN) since the introduction of the term at Digestive Disease Week in 2006 [2, 5–7]. Internal drainage of PP has traditionally been performed by open surgical drainage via laparotomy with cystogastrostomy or cystenterostomy [8, 9]. This procedure is performed via a generous anterior gastrotomy with the creation of a wide posterior cystogastrostomy, which is then oversewn. The overall complication rate for open surgical drainage and debridement remains about 12–14 %, with a mortality rate of approximately 25 % (range = 15–43 %) and even higher in patients with multisystem organ failure [6, 8, 10, 11]. This is even in the face of technical advancement with linear staplers and resultant smaller gastrotomies.
Over the past decade minimally invasive techniques for pancreatic pseudocyst drainage and debridement have been developed, although no optimal approach has been standard given the range of clinical and anatomic variations [9, 12]. Advantages of a laparoscopic approach to cystogastrostomy and pancreatic debridement (versus an endoscopic approach) include the ability to create a larger anastomosis, obtain hemostasis of incised gastric/cyst walls, and more easily manage complications such as hemorrhage or perforation if it occurs, while still allowing for evaluation and debridement of the inner cyst cavity [10]. It has been argued that there are limitations to the application of a laparoscopic approach due to the need for special expertise and surgical skills [6]. We feel that the technique employed at our institution (laparoscopic transgastric endolumenal cystogastrostomy with trocar placement directly into the gastric lumen) is straightforward, has resulted in excellent outcomes, and can be applied more widely and consistently to advance the surgical treatment of PP. The goals of this article are to describe this technique and evaluate its clinical outcomes.
Materials and methods
Procedure
Our laparoscopic transgastric endolumenal approach is illustrated in Fig. 1 and the steps are listed in Table 1. A standard laparoscopic camera is inserted at the umbilicus using either a Veress needle or an open Hassan technique at the discretion of the surgeon. After a thorough inspection of the abdomen with aspiration of any fluid, three upper abdominal ports are placed. Two 5-mm balloon ports are positioned on the left side and a 12-mm balloon port is placed at the midline in the subxiphoid area. A perioral upper GI endoscopy is then performed with a large-channel, forward-viewing flexible endoscope (GIS-Q180; Olympus, Melville, NY).
Under endoscopic visualization, three small gastrotomies are made and the transabdominal balloon ports are inserted into the gastric lumen (Fig. 2). Endoscopic insufflation of the stomach aids in visualization and also provides some stability for port placement. The 12-mm port should be placed in the distal antrum for optimal positioning. The two 5-mm ports are placed along the greater curvature of the stomach as far from each other as possible for increased ease of movement during debridement and suturing. A fourth port is sometimes needed. It is important to use balloon ports so that the stomach will remain adherent to the abdominal wall throughout the procedure and minimize possible leakage of gastric contents into the peritoneal cavity. With the stomach then retracted in apposition with the anterior abdominal wall, the transgastric ports are carefully inspected to ensure they are within the gastric lumen (Fig. 3). Endolumenal insufflation can then be achieved through the transgastric ports. The endoscope is left in position to be used once the cystogastrostomy is created.
A laparoscopic ultrasound probe is inserted through the 12-mm port and the peripancreatic retrogastric fluid collection is visualized. There usually is hypoechoic fluid with varying degrees of debris and necrosis present. With confirmation of the fluid location by ultrasound, a longitudinal 1-cm posterior gastrotomy along the axis of the pancreas is made using an electrocautery tip or Harmonic Scalpel® (Ethicon EndoSurgery, Cincinnati, OH). Bleeding vessels can be encountered in the posterior gastric wall and are usually fairly easily controlled with electrocautery and/or a vessel-sealing device. Ultrasound again is used to confirm that the cyst wall is being approached (Fig. 4). Once the cyst wall is opened, a linear stapler is used to create the cystogastrostomy. The cystogastrostomy can be extended with multiple firings of the linear stapler as necessary (Fig. 5). Cyst cavity exploration is permitted with either the laparoscope or the endoscope secondary to the wide cystogastrostomy and biopsies of the cyst wall can also be taken at this time. The endoscopic view is often indispensable when necrosis extends far into the pancreatic head.
Next, entrance of the instruments into the cyst cavity is confirmed with ultrasound (Fig. 6). The pancreatic and peripancreatic necrosis is then thoroughly debrided and removed through the 12-mm-port site. We believe it is paramount to debride as much necrosis as possible at the initial operation and have noted that the size of the cystogastrostomy necessary is dictated by the amount of necrosis present. The interior of the cyst cavity can be clearly identified and visualized with an endoscope, and upon surveying the cyst interior, any remaining necrosis is debrided and the cavity copiously irrigated until clean (Fig. 7). During debridement it is critical to remember the large vascular structures posterior to the cyst. When necrotic-appearing tissue can not be pulled away with gentle retraction, it is often because a vascular structure has been encountered.
The cystogastrostomy is then matured using a suturing technique of the surgeon’s preference (Fig. 8 illustrates intracorporeal suturing). Given the angles for suturing circumferentially, the utilization of a suturing device may not be possible and in this situation we prefer to use a hand-sewing method. We recommend placement of interrupted figure-of-eight sutures circumferentially, being careful to anastomose the cyst wall with full-thickness stomach wall. Placement of these sutures can be challenging given the small spaces present and angles required. The suturing ensures that the cyst is anastomosed to the posterior gastric wall so that there is no leak and it also decreases the chance of bleeding from the edges of the posterior gastric wall.
To complete the procedure, a nasogastric tube is inserted through the widely patent cystogastrostomy for postoperative drainage. Balloons are then deflated and ports extracted from the stomach. The anterior gastrotomies are closed with intracorporeal suturing and knot-tying techniques (Fig. 9). Adequate closure is assured by insufflation of the stomach (leak test) following closure of the port sites.
Results
Twenty-two patients underwent attempted laparoscopic transgastric endolumenal drainage of their symptomatic PP from October 2006 until March 2013 (Table 2). Median age was 49.5 ± 12 years (range = 18–71) and 10/22 were female. Average body mass index (BMI) in the group was 29.1 kg/m2 and 77 % had an American Society of Anesthesiologists (ASA) score ≥3. Comorbidities included hypertension (55 %), diabetes mellitus type II (50 %), tobacco use (18 %), and alcohol abuse (5 %). Gallstones were the most common etiology (50 %). Other etiologies included hypertriglyceridemia (14 %) and alcohol (14 %). The remaining 23 % were idiopathic. Fifty-five percent of the pseudocysts were considered to be chronic, and the median time between initial presentation and surgery was 86 days (range = 0–360). Presenting symptoms included abdominal pain in 77 % of patients and associated nausea/emesis in 50 %. Early satiety, diarrhea, and anorexia were reported less frequently. Weight loss was reported by 41 % of the cohort.
Pseudocyst characteristics were examined as well (Table 3). They were found to have an average size of 13.72 ± 4.71 cm (range = 3.7–25 cm) and were located in the body, with or without tail or neck involvement, in 18 patients, and in the tail with or without head or neck involvement in the remaining 5 patients. Gutter extension of the pseudocyst was present 32 % of the time. There was a failed attempt at endoscopic cystogastrostomy in one patient but a second attempt was successful but did not resolve the patient’s symptoms. The splenic vein was thrombosed in four patients. Finally, seven patients had positive cultures from the pancreatic necrosis taken at the time of operation.
Seven patients required conversion to an open procedure. Three patients had multiple dense adhesions and in another patient fluid was unable to be clearly aspirated from the pseudocyst, even under ultrasound guidance. A fifth patient’s body habitus prevented adequate pneumoperitoneum. In the sixth patient, the cystogastrostomy was made and the majority of the debridement completed. However, it was noted that despite multiple maneuvers, the head of the pancreas could not be reached for adequate debridement. This was felt to be due to difficult angles, likely related to the superior and anterior displacement of the stomach, even after cyst fluid evacuation. The seventh patient required conversion secondary to inability to sufficiently angle the laparoscopic stapler to create the cystogastrostomy. In addition, eight patients also had a cholecystectomy as part of their procedure.
Mean operative time was 220 ± 65 min (median = 213) and was not substantially affected by the addition of a cholecystectomy (mean operative time = 215 ± 54 min). The mean estimated blood loss was 223 ± 259 cc (median = 100; range = 20–1,000) and eight patients received an intraoperative blood transfusion. Forty-one percent of patients went to the intensive care unit postoperatively and the overall average length of stay was 14.9 days (median = 7.5; range = 4–50) Table 4.
Eight patients had complications within the 30-day postoperative period. One was procedure-related with bleeding from the cystogastrostomy staple line which was not oversewn during the initial operation. The patient underwent an upper endoscopy with clip placement on postoperative day (POD) 4, but rebled on POD 10. An emergent laparotomy was performed and the bleeding suture line was oversewn; the patient subsequently had an uneventful recovery. The other six complications were not procedure-related. One patient had seizures on POD 14, which were thought to be a reaction to levofloxacin. During this time she was also plagued with a persistent biliary stricture that was treated with percutaneous transhepatic cholecystostomy tube placement for a septic episode. This was followed by definitive treatment with creation of a side-to-side choledochoduodenostomy 4 months after laparoscopic cystogastrostomy and pancreatic debridement. A second patient had changes in mental status on POD 14 with respiratory distress and required reintubation for 48 h. He was found to have a urinary tract infection as well. A third patient had prolonged hospitalization complicated by line sepsis, ventilator dependence, deconditioning, and dysphagia requiring short-term total parenteral nutrition. Two patients had postoperative dysphagia requiring PEG placement. Five patients required readmission for dehydration, two of which additionally required antibiotics for urinary tract infections.
Two patients were not seen after discharge from the hospital. The average follow-up for the remaining 20 patients was 3.4 months (median = 2; range = 1–11). Eleven had follow-up abdominal imaging that demonstrated substantial or complete resolution of their PP. There were no late recurrences, complications, or mortalities. All patients had resolution of their symptoms.
Discussion
Laparoscopic transgastric cystogastrostomy techniques are reported to result in adequate internal drainage and debridement of PP with minimal morbidity and mortality. However, experience with these techniques is limited and reported long-term clinical outcomes following laparoscopic drainage are lacking [13]. Conversely, low complication rates and good outcomes are reported for the immediate postoperative period and appear to be reproducible even though the number of cases is small [4, 12]. It is important to recognize that this approach does not compete with interventional radiology or endoscopy [12]. Rather, the laparoscopic transgastric cystogastrostomy and pancreatic debridement procedure bridges the wide gap between interventional techniques and conventional surgery [12].
There are several good reasons to use laparoscopic transgastric endolumenal cystogastrostomy and pancreatic debridement. First, the complete removal of necrosis is possible as well as a wide cystogastrostomy opening [10, 14, 15]. In our experience we have found this to consistently be the case. Second, access to the lesser sac, paracolic gutters, perinephric space, and retroduodenal space for drainage is possible as well. Finally, for the large majority of patients, one procedure will relieve symptoms and a shorter length of stay is noted compared to open cystogastrostomy [1, 9, 10, 12, 15–20].
The use of intraoperative laparoscopic ultrasound is extremely useful in avoiding hemorrhage as blood vessels in the cyst wall can be visualized intraoperatively and precisely avoided. Intraoperative ultrasound is also helpful in locating the pseudocyst, if it does not bulge into the stomach, and in excluding pseudoaneurysms [1, 2]. Others have taken the position that intraoperative laparoscopic ultrasound is unnecessary if preoperative CT scans are carefully evaluated [1]. However, the procedure adds minimal time and minimal, if any, morbidity. Furthermore, in our experience real-time information is exceedingly useful to the operating surgeon.
There are variations in the reported surgical techniques for laparoscopic transgastric cystogastrostomy and pancreatic debridement. Some authors state that a single port of entry into the stomach is all that is required if the gastroscope is used as the camera source [19]. In our opinion, using the laparoscope gives us a view that is more familiar and also of higher resolution. This makes the operation easier and allows for a wider view and more thorough debridement. Also, the use of one, two, or three intragastric ports has been reported [10, 12, 19, 20]. In our experience three intragastric ports decreased the technical difficulty of suturing and allowed for a more complete debridement. No increased morbidity or substantial increase in operative time has been noted.
There have been various debates in the literature regarding the advantages and disadvantages of both the anterior and the posterior approach to PP [16]. The anterior approach is similar to the technique we used in this case series. The posterior approach is performed by directly visualizing the posterior wall of the stomach and the pseudocyst, opening and draining the pseudocyst, and then using a stapler and running sutures for closure [16]. The anterior approach is felt to be the technically easier procedure but requires two anastomoses: posterior staple line between stomach and cyst and anterior gastric wall gastrostomy closures [13, 16]. On the other hand, the posterior approach is reported to have better visualization and allow for a large anastomosis but is felt to be more difficult to learn [13]. A retroperitoneal approach has also been described; however, its effectiveness needs to be confirmed and its reported advantages of decreased need for dilation procedures, multiple procedures, and feasibility in patients who cannot tolerate pneumoperitoneum need to be further evaluated [5]. Future randomized trials will be needed to determine which approach is truly superior.
Opponents of the laparoscopic transgastric approach argue that the need to induce pneumoperitoneum and the potential risk of infection and bowel injury limit the usefulness of this technique in critically ill patients [6]. Difficulty with tolerance of pneumoperitoneum was not observed in our experience and has not been reported to date in the literature in regard to this technique. No infections resulted from surgery and no bowel was injured in our experience. Furthermore, none of the ten other case series reported occurrence of either of these potential complications. It would not be unreasonable to presume that the risk would likely be comparable to that associated with any other laparoscopic abdominal procedure. Some opponents also cite cost and requirement of special instruments as disadvantages to laparoscopic cystogastrostomy [19]. While this may have been true in the past, we have demonstrated consistently, along with others, that routine laparoscopic instruments can be used to complete this procedure.
This study does have a few limitations. We had a small sample size with short-term follow-up and reviewed cases in a retrospective fashion. We also did not evaluate cost or perform a quality-of-life survey. However, given that laparoscopic transgastric endolumenal cystogastrostomy is a promising technique for cystogastrostomy creation, it should be regarded as a valid therapeutic option for necrotizing pancreatitis with resultant pseudocyst or WOPN formation because validation in a randomized trial will be limited for reasons previously discussed.
In summary, we have demonstrated that laparoscopic transgastric endolumenal cystogastrostomy with pancreatic debridement is feasible, highly effective, and safe in our limited number of patients. Strong consideration should be given to this straightforward and successful minimally invasive technique for cystogastrostomy creation and pancreatic debridement.
References
Hamza N, Ammori BJ (2010) Laparoscopic drainage of pancreatic pseudocysts: a methodological approach. J Gastrointest Surg 14:148–155
Fischer A, Schrag HJ, Keck T, Hopt UT, Utzolino S (2008) Debridement and drainage of walled-off pancreatic necrosis by a novel laparoendoscopic rendezvous maneuver: experience with six cases. Gastrointest Endosc 67:871–878
Aljarabah M, Ammori BJ (2007) Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. Surg Endosc 21:1936–1944
Aghdassi A, Mayerle J, Kraft M, Sielenkamper AW, Heidecke CD, Lerch MM (2008) Diagnosis and treatment of pancreatic pseudocysts in chronic pancreatitis. Pancreas 36:105–112
Munene G, Dixon E, Sutherland F (2011) Open transgastric debridement and internal drainage of symptomatic non-infected walled-off pancreatic necrosis. HPB (Oxford) 13:234–239
Navaneethan U, Vege SS, Chari ST, Baron TH (2009) Minimally invasive techniques in pancreatic necrosis. Pancreas 38:867–875
Stamatakos M, Stefanaki C, Kontzoglou K, Stergiopoulos S, Giannopoulos G, Safioleas M (2010) Walled-off pancreatic necrosis. World J Gastroenterol 16:1707–1712
Bucher P, Pugin F, Morel P (2008) Minimally invasive necrosectomy for infected necrotizing pancreatitis. Pancreas 36:113–119
Melman L, Azar R, Beddow K, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Edmundowicz S, Jonnalagadda S, Matthews BD (2009) Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystogastrostomy for pancreatic pseudocysts. Surg Endosc 23:267–271
Libby ED, Taylor J, Mysh D, Schwaitzberg SD (1999) Combined laparoendoscopic cystogastrostomy. Gastrointest Endosc 50:416–419
Amano H, Takada T, Isaji S, Takeyama Y, Hirata K, Yoshida M, Mayumi T, Yamanouchi E, Gabata T, Kadoya M, Hattori T, Hirota M, Kimura Y, Takeda K, Wada K, Sekimoto M, Kiriyama S, Yokoe M, Arata S (2010) Therapeutic intervention and surgery of acute pancreatitis. J Hepatobiliary Pancreat Sci 17:53–59
Mori T, Abe N, Sugiyama M, Atomi Y (2002) Laparoscopic pancreatic cystogastrostomy. J Hepatobiliary Pancreat Surg 9:548–554
Matsutani T, Sasajima K, Miyamoto M, Yokoyama T, Hiroi M, Maruyama H, Suzuki S, Tajiri T (2007) Pancreatic cyst associated with pancreas divisum treated by laparoscopy-assisted cystogastrostomy in the intragastric approach: a case report and a review of the literature. J Laparoendosc Adv Surg Tech A 17:317–320
Hauters P, Weerts J, Peillon C, Champault G, Bokobza B, Roeyen G, Totte E, Siriser F (2004) Treatment of pancreatic pseudocysts by laparoscopic cystogastrostomy. Ann Chir 129:347–352
Park AE, Heniford BT (2002) Therapeutic laparoscopy of the pancreas. Ann Surg 236:149–158
Barragan B, Love L, Wachtel M, Griswold JA, Frezza EE (2005) A comparison of anterior and posterior approaches for the surgical treatment of pancreatic pseudocyst using laparoscopic cystogastrostomy. J Laparoendosc Adv Surg Tech A 15:596–600
Owera AM, Ammori BJ (2008) Laparoscopic endogastric and transgastric cystogastrostomy and pancreatic necrosectomy. Hepatogastroenterology 55:262–265
Hauters P, Weerts J, Navez B, Champault G, Peillon C, Totte E, Barthelemy R, Siriser F (2004) Laparoscopic treatment of pancreatic pseudocysts. Surg Endosc 18:1645–1648
Ramachandran CS, Goel D, Arora V, Kumar M (2002) Gastroscopic-assisted laparoscopic cystogastrostomy in the management of pseudocysts of the pancreas. Surg Laparosc Endosc Percutan Tech 12:433–436
Gagner M (1996) Laparoscopic treatment of acute necrotizing pancreatitis. Semin Laparosc Surg 3:21–28
Disclosures
Drs. Simo, Niemeyer, Swan, Sindram, Martinie, and Iannitti have no financial, consultant, institutional, or other relationships with any company, including pharmaceutical or device companies, that might create bias or a conflict of interest regarding this manuscript. No funding was received for this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Accepted as an oral poster at the 2012 AHPBA meeting, Miami, FL, and the 2012 IHPBA meeting, Paris, France.
Rights and permissions
About this article
Cite this article
Simo, K.A., Niemeyer, D.J., Swan, R.Z. et al. Laparoscopic transgastric endolumenal cystogastrostomy and pancreatic debridement. Surg Endosc 28, 1465–1472 (2014). https://doi.org/10.1007/s00464-013-3317-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3317-5