Abstract
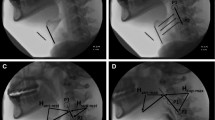
Videofluoroscopic swallow studies are widely used in clinical and research settings to assess swallow function and to determine physiological impairments, diet recommendations, and treatment goals for people with dysphagia. Videofluoroscopy can be used to analyze biomechanical events of swallowing, including hyoid bone displacement, to differentiate between normal and disordered swallow functions. Previous research has found significant associations between hyoid bone displacement and penetration/aspiration during swallowing, but the predictive value of hyoid bone displacement during swallowing has not been explored. The primary objective of this study was to build a model based on aspects of hyoid bone displacement during swallowing to predict the extent of airway penetration or aspiration during swallowing. Aspects of hyoid bone displacement from 1433 swallows from patients referred for videofluoroscopy were analyzed to determine which aspects predicted risk of penetration and aspiration according to the Penetration–Aspiration Scale. A generalized estimating equation incorporating components of hyoid bone displacement and variables shown to impact penetration and aspiration (such as age, bolus volume, and viscosity) was used to evaluate penetration and aspiration risk. Results indicated that anterior-horizontal hyoid bone displacement was the only aspect of hyoid bone displacement predictive of penetration and aspiration risk. Further research should focus on improving the model performance by identifying additional physiological swallowing events that predict penetration and aspiration risk. The model built for this study, and future modified models, will be beneficial for clinicians to use in the assessment and treatment of people with dysphagia, and for potentially tracking improvement in hyolaryngeal excursion resulting from dysphagia treatment, thus mitigating adverse outcomes that can occur secondary to dysphagia.

Similar content being viewed by others
References
Clavé P, Shaker R. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015;12(5):259–70.
Dudik JM, Coyle JL, El-Jaroudi A, Sun M, Sejdić E. A matched dual-tree wavelet denoising for tri-axial swallowing vibrations. Biomed Signal Process Control. 2016;27:112–21.
Miller AJ. The neurobiology of swallowing and dysphagia. Dev Disabil Res Rev. 2008;14(2):77–86.
Movahedi F, Kurosu A, Coyle JL, Perera S, Sejdić E. Anatomical directional dissimilarities in tri-axial swallowing accelerometry signals. IEEE Trans Neural Syst Rehabilit Eng. 2017;25(5):447–58.
Bhattacharyya N. The prevalence of dysphagia among adults in the United States. Otolaryngol Head Neck Surg. 2014;151(5):765–9.
Murray J. Manual of dysphagia assessment in adults. Boston: Cengage Learning; 1999.
Lazarus C, Logemann A. Swallowing disorders in closed head trauma patients. Arch Phys Med Rehabil. 1987;68(2):79–84.
Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116(2):455–78.
Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. Br Med J. 1987;295(6595):411–4.
Humbert IA, Robbins J. Dysphagia in the elderly. Phys Med Rehabil Clin N Am. 2008;19(4):853–66.
Gorell JM, Johnson CC, Rybicki BA. Parkinson’s disease and its comorbid disorders An analysis of Michigan mortality data, 1970 to 1990. Neurology. 1994;44(10):1865–1865.
Coyle JL, Davis LA, Easterling C, Graner DE, Langmore S, Leder SB, Lefton-Greif MA, Leslie P, Logemann JA, Mackay L, Martin-Harris B, Murray JT, Sonies B, Steele CM. Oropharyngeal dysphagia assessment and treatment efficacy: setting the record straight (response to Campbell–Taylor). J Am Med Directors Assoc. 2009;10(1):62–6.
Rugiu M. Role of videofluoroscopy in evaluation of neurologic dysphagia. Acta Otorhinolaryngol Ital. 2007;27(6):306.
Molfenter SM, Steele CM. Physiological variability in the deglutition literature: hyoid and laryngeal kinematics. Dysphagia. 2011;26(1):67–74.
Kim Y, McCullough GH. Maximum hyoid displacement in normal swallowing. Dysphagia. 2008;23(3):274–9.
Kang B-S, Oh B-M, Kim IS, Chung SG, Kim SJ, Han TR. Influence of aging on movement of the hyoid bone and epiglottis during normal swallowing: a motion analysis. Gerontology. 2010;56(5):474–82.
Martin-Harris B, Jones B. The videofluorographic swallowing study. Phys Med Rehabil Clin N Am. 2008;19(4):769–85.
Zhang Z, Kurosu A, Coyle J, Perera S, Sejdić E. Hyoid displacement during swallowing is related to penetration–aspiration scores. Under Review.
Kendall KA, Leonard RJ. Hyoid movement during swallowing in older patients with dysphagia. Arch Otolaryngol Head Neck Surg. 2001;127(10):1224–9.
Perlman AL, Booth B, Grayhack J. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994;9(2):90–5.
Su J, Yuan C, Shu K. Hyoid bone displacement during swallowing have no association with penetration/aspiration severity in dysphagic stroke patients. Arch Phys Med Rehabil. 2014;95(10):e16.
Molfenter SM, Steele CM. Kinematic and temporal factors associated with penetration–aspiration in swallowing liquids. Dysphagia. 2014;29(2):269–76.
Seo HG, Oh B-M, Han TR. Swallowing kinematics and factors associated with laryngeal penetration and aspiration in stroke survivors with dysphagia. Dysphagia. 2016;31(2):160–8.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11(2):93–8.
Lof GL, Robbins J. Test–retest variability in normal swallowing. Dysphagia. 1990;4(4):236–42.
Wang M. Generalized estimating equations in longitudinal data analysis: a review and recent developments. Adv Stat. 2014. https://doi.org/10.1155/2014/303728.
Acknowledgement
The authors acknowledge Dr. Aliaa Elbahnasy Sabry for her critical review and suggestions on the final manuscript.
Funding
This study was funded by two grants from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD092239, while the data was collected under Award Number R01HD074819. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Prediction equation steps:
- 1.
Let \(XB=-3.479-0.0583\times (x1_min2max_distance)+ 0.0265\times (age)-0.0004\times (duration)\)
- 2.
Subtract from XB 0.4435 if the swallow is single, add to XB 0.4545 if the swallow is multiple 1, or do nothing if multiple 2.
- 3.
Subtract from XB 0.1398 if the \(\hbox {sex}=2(\hbox {female}?)\), or do nothing if \(\hbox {sex}=1(\hbox {male}?)\).
- 4.
Add 1.2862 to XB if \(\hbox {viscosity}=\hbox {thin}\), add 0.7049 if nectar, subtract 0.5334 if pudding, and do nothing if cookie.
- 5.
Add to XB 0.1622 if spoon, or do nothing if cup.
- 6.
Add to XB 0.0994 if chin down, or do nothing if head position is neutral.
- 7.
Compute the probability of a high PA swallow as \(exp(XB)/(1+exp(XB))\).
Rights and permissions
About this article
Cite this article
Zhang, Z., Perera, S., Donohue, C. et al. The Prediction of Risk of Penetration–Aspiration Via Hyoid Bone Displacement Features. Dysphagia 35, 66–72 (2020). https://doi.org/10.1007/s00455-019-10000-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10000-5