Abstract
Purpose
Hyolaryngeal excursion (HE) is typically assessed via palpation during clinical swallowing exams (CSE) or visually during videofluoroscopy (VFSS). Minimal evidence exists to support the use of these perceptual methods for judging HE. We investigated whether binary judgment of HE differentiates quantitative measures of hyoid movement, using frame-by-frame VFSS analysis to measure anatomically scaled peak hyoid positions.
Methods
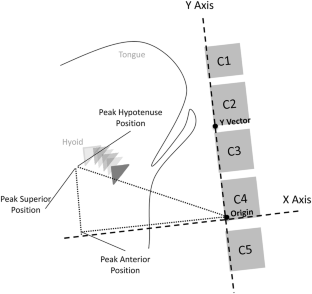
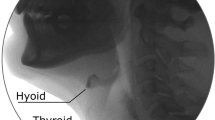
Medical records of patients who received a CSE and VFSS within a 24-h period were reviewed. Clinician ratings of HE (‘reduced’ or ‘normal’) were collected from CSE and VFSS reports, along with rater experience. Five ml puree swallows were extracted from each VFSS for randomized, blinded analysis. Peak hyoid position from C4 was captured in anterior, superior, and hypotenuse positions and expressed relative to C2–C4 length. T-test comparisons of hyoid positions between patients judged to have reduced versus normal HE on palpation and VFSS were conducted.
Results
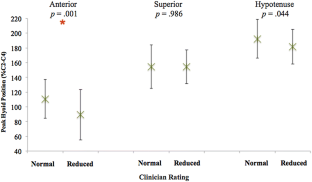
Eighty-seven patients (56 male, mean age 61) met criteria. Peak anterior hyoid position was significantly different between patients judged to have reduced (mean = 89.2% C2–C4) and normal (mean = 110.6% C2–C4) HE on palpation (p = 0.001). Further analysis revealed no effect of clinician experience on differentiation of objective measures based on palpation. No differences were found across any objective measures when compared to clinician VFSS ratings.
Conclusions
Clinicians appeared to be able to differentiate peak anterior hyoid movement but not superior or hypotenuse movement on palpation. On VFSS visualization, no significant differences were found between swallows judged to have reduced versus normal HE in any directional dimension. While perceptual methods may contribute to clinical decision-making, clinicians should remain cautious when making judgments about HE using these methods.
Similar content being viewed by others
Change history
16 September 2020
This letter notifies the readers of the Dysphagia journal of an error in the original published version of this manuscript, for which a previously available open source spreadsheet tool had been used to calculate the position of the hyoid bone or larynx on lateral view videofluoroscopic images. An error in the mathematical formula built into the spreadsheet resulted in a reversal of the results for the X and Y planes of measurement. This erratum provides corrections to the results and interpretations of the original manuscript.
References
Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154(5):953–63. https://doi.org/10.2214/ajr.154.5.2108569.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19(4):691–707. https://doi.org/10.1016/j.pmr.2008.06.001.
Paik NJ, Kim SJ, Lee HJ, Jeon JY, Lim JY, Han TR. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J Electromyogr Kines. 2008;18(2):329–35. https://doi.org/10.1016/j.jelekin.2006.09.011.
Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, Lin S. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol. 1992;262(2 Pt 1):G338–44. https://doi.org/10.1152/ajpgi.1992.262.2.G338.
Jacob P, Kahrilas PJ, Logemann JA, Shah V, Ha T. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989;97(6):1469–78.
McCullough GH, Rosenbek JC, Wertz RT, McCoy S, Mann G, McCullough K. Utility of clinical swallowing examination measures for detecting aspiration post-stroke. J Speech Lang Hear Res. 2005;48(6):1280–93. https://doi.org/10.1044/1092-4388(2005/089).
Ramsey DJC, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003;34(5):1252–7. https://doi.org/10.1161/01.Str.0000066309.06490.B8.
Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin, TX: Pro-Ed; 1998.
McCullough GH, Martino R. Clinical evaluation of patients with dysphagia: importance of history taking and physical exam. In: Shaker EC, Belafsky PC, Postma GN, editors. Manual of diagnostic and therapeutic techniques for disorders of deglutition. New York: Springer; 2013. p. 11–30.
Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002;17(4):262–72. https://doi.org/10.1007/s00455-002-0064-5.
Kim Y, McCullough GH. Maximum hyoid displacement in normal swallowing. Dysphagia. 2008;23(3):274–9. https://doi.org/10.1007/s00455-007-9135-y.
Chi-Fishman G, Sonies BC. Effects of systematic bolus viscosity and volume changes on hyoid movement kinematics. Dysphagia. 2002;17(4):278–87. https://doi.org/10.1007/s00455-002-0070-7.
Nagy A, Molfenter SM, Peladeau-Pigeon M, Stokely S, Steele CM. The effect of bolus volume on hyoid kinematics in healthy swallowing. Biomed Res Int. 2014;2014:738971. https://doi.org/10.1155/2014/738971.
Rofes L, Arreola V, Martin A, Clave P. Natural capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut. 2013;62(9):1280–7. https://doi.org/10.1136/gutjnl-2011-300753.
Leow LP, Huckabee ML, Sharma S, Tooley TP. The influence of taste on swallowing apnea, oral preparation time, and duration and amplitude of submental muscle contraction. Chem Senses. 2007;32(2):119–28. https://doi.org/10.1093/chemse/bjl037.
Leonard RJ, Kendall KA, McKenzie S, Goncalves MI, Walker A. Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia. 2000;15(3):146–52. https://doi.org/10.1007/s004550010017.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000;43(5):1264–74.
Molfenter SM, Steele CM. Physiological variability in the deglutition literature: hyoid and laryngeal kinematics. Dysphagia. 2011;26(1):67–74. https://doi.org/10.1007/s00455-010-9309-x.
McCullough GH, Wertz RT, Rosenbek JC, Dinneen C. Clinicians’ preferences and practices in conducting clinical-bedside and videofluoroscopic swallowing examinations in an adult, neurogenic population. Am J Speech Lang Pathol. 1999;8(2):149–63.
Mann G. MASA: the Mann assessment of swallowing ability. Boston: Cengage Learning; 2002.
McCullough GH, Wertz RT, Rosenbek JC, Mills RH, Ross KB, Ashford JR. Inter- and intrajudge reliability of a clinical examination of swallowing in adults. Dysphagia. 2000;15(2):58–67. https://doi.org/10.1007/s004550010002.
Rangarathnam B, McCullough GH. Utility of a clinical swallowing exam for understanding swallowing physiology. Dysphagia. 2016;31(4):491–7. https://doi.org/10.1007/s00455-016-9702-1.
Lee JW, Randall DR, Evangelista LM, Kuhn MA, Belafsky PC. Subjective assessment of videofluoroscopic swallow studies. Otolaryngol Head Neck Surg. 2017;156(5):901–5. https://doi.org/10.1177/0194599817691276.
Schneider CA, Rasband WS, Eliceiri KW. NIH image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9(7):671–5.
Molfenter SM, Steele CM. Use of an anatomical scalar to control for sex-based size differences in measures of hyoid excursion during swallowing. J Speech Lang Hear Res. 2014;57(3):768–78. https://doi.org/10.1044/2014_Jslhr-S-13-0152.
Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995;38(3):579–85.
Thompson TZ, Obeidin F, Davidoff AA, Hightower CL, Johnson CZ, Rice SL, Sokolove RL, Taylor BK, Tuck JM, Pearson WG Jr. Coordinate mapping of hyolaryngeal mechanics in swallowing. J Vis Exp. 2014. https://doi.org/10.3791/51476.
Fleiss JL. The design and analysis of clinical experiments. New York, NY: Wiley; 1986.
Steele CM, Bailey GL, Chau T, Molfenter SM, Oshalla M, Waito AA, Zoratto DC. The relationship between hyoid and laryngeal displacement and swallowing impairment. Clin Otolaryngol. 2011;36(1):30–6. https://doi.org/10.1111/j.1749-4486.2010.02219.x.
World Health Organization. Physical status: the use and interpretation of anthropometry. Technical Report Series. Geneva: WHO; 1995.
Molfenter SM, Steele CM. Use of an anatomical scalar to control for sex-based size differences in measures of hyoid excursion during swallowing. J Speech Lang Hear Res. 2014;57(3):768–78. https://doi.org/10.1044/2014_JSLHR-S-13-0152.
Benoist M. Natural history of the aging spine. Eur Spine J. 2003;12(Suppl 2):S86–9. https://doi.org/10.1007/s00586-003-0593-0.
Malcolm GP. Surgical disorders of the cervical spine: presentation and management of common disorders. J Neurol Neurosurg Psychiatry. 2002;73(Suppl 1):i34–41.
Ezra D, Masharawi Y, Salame K, Slon V, Alperovitch-Najenson D, Hershkovitz I. Demographic aspects in cervical vertebral bodies’ size and shape (C3–C7): a skeletal study. Spine J. 2017;17(1):135–42. https://doi.org/10.1016/j.spinee.2016.08.022.
Palmer JB, Tanaka E, Ensrud E. Motions of the posterior pharyngeal wall in human swallowing: a quantitative videofluorographic study. Arch Phys Med Rehabil. 2000;81(11):1520–6. https://doi.org/10.1053/apmr.2000.17829.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS measurement tool for swallow impairment—MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405. https://doi.org/10.1007/s00455-008-9185-9.
Acknowledgements
The authors would like to thank James C. Borders for his assistance during data collection, Glen Leverson and Sharon Weinberg for their assistance during data analysis, and the speech-language pathologists at UW-Madison Voice and Swallow clinics. Portions of this work were presented at the 2018 Dysphagia Research Society meeting.
Funding
Diane M. Bless Endowed Chair in Otolaryngology, University of Wisonsin-Madison.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The research conducted by the first author was supported by funding from the Diane M. Bless Endowed Chair in Otolaryngology. The authors declare no conflict of interest to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was waived with IRB approval for retrospective medical chart review data collection.
Rights and permissions
About this article
Cite this article
Brates, D., Molfenter, S.M. & Thibeault, S.L. Assessing Hyolaryngeal Excursion: Comparing Quantitative Methods to Palpation at the Bedside and Visualization During Videofluoroscopy. Dysphagia 34, 298–307 (2019). https://doi.org/10.1007/s00455-018-9927-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9927-2