Abstract
Purpose
The biomarker characteristics of breast cancer plays an important role in predicting treatment sensitivity. The aim of the present study was to compare immunohistochemical profiles (ER, PR, HER2, and Ki67) between the primary tumor and synchronous axillary lymph node metastasis and investigate the subsequent effects on neoadjuvant therapy response.
Methods
A total of 358 patients with pathologically confirmed synchronous axillary lymph node metastasis at first diagnosis and treated by neoadjuvant therapy at Peking University First Hospital from January 1, 2013 to December 31, 2022 were included in this retrospective study. Clinicopathologic data, especially receptor status in primary and metastatic foci, was collected for each case.
Results
Change of ER, PR, HER2, and Ki67 expression was observed in 5.9%, 8.7%, 12.6%, and 17.3% of patients, respectively. HR discordance was observed more frequently when the ER status (p = 0.023) or PR status (p = 0.010) of primary tumor was negative, while HER2 discordance seemed to be more frequent when the HER2 status of primary tumor was HER2-0 or HER2-low (p < 0.001). Patients with loss of HR-positivity (positive to negative) responded to neoadjuvant chemotherapy better compared to those with stable positive HR expression (50% vs. 11.1%, p = 0.0017). A significantly decrease in pCR rate was observed in patients with unstable HER2 status, but not in the HER2-0/HER2-low subgroup.
Conclusion
Receptor discordance between primary tumor and synchronous axillary LNM appears to already exist before any anti-tumor therapy. This instability has limited clinical impact on the choice of neoadjuvant therapy at current stage, but further investigation is warranted with the incremental application of endocrine drugs and ADCs in neoadjuvant therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is recognized as a highly heterogeneous disease that accounts for almost one third (31%) of female cancers (Siegel et al. 2023). In the past decades, the field of breast cancer treatment has gradually entered the era of precision medicine. Oncologists now classify invasive breast cancer based on immunohistochemical analysis of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and proliferation factor Ki67, which not only provides prognostic information but it is also crucial for predicting treatment sensitivity. However, previous studies have reported changes in immunohistochemical expression of these four biomarkers between primary and metastatic tumors, and there may be even a significant prognostic impact of phenotype conversion (Lindstrom et al. 2012; Mellouli et al. 2022). Discordance in these tumor biomarkers has been reported due to analytical error, intratumoral heterogeneity, selective pressure of therapy and cellular clonal evolution (Shiino et al. 2022). Thus, current guidelines recommend biopsy of the first site of metastasis for recurrent or stage IV disease in order to decide on the appropriate first-line systemic therapy (Gradishar et al. 2023; Rugo et al. 2016).
Although the current studies primarily focus on distant metastasis, several studies with small sample size have evaluated the discordance in biomarker status between primary tumors and synchronous axillary lymph node metastasis (LNM) based on surgical specimens, showing lower discordance rate (Falck et al. 2010; Janeva et al. 2023; Li et al. 2016; Weydandt et al. 2022). Actually, the importance of pretherapeutic receptor expression in guiding treatment is increasing, because neoadjuvant chemotherapy has become part of the standard treatment regimen for locally advanced disease. However, in routine clinical practice, management of early invasive breast cancer patients with synchronous LNM is frequently based on the biomarker status of the primary tumor, ignoring the immunohistochemical analysis of LNM. Moreover, the successful development of antibody–drug conjugates (ADCs) challenged the traditional evaluation criteria for HER2 expression (Modi et al. 2022). High instability of HER2-low-positive expression from primary breast cancer to relapse has been reported, but the implications of this alteration in neoadjuvant therapy remain uncertain (Miglietta et al. 2021).
In the present work, we evaluated the prevalence of discordance in biomarker status (ER, PR, HER2, and Ki67) between the primary tumor and synchronous axillary LNM, as well as the impact of such alterations on neoadjuvant therapy response.
Method
Patients
The clinicopathological data of early invasive breast cancer patients treated with neoadjuvant therapy from the database of the Breast Disease Center of Peking University First Hospital from January 1, 2013, to December 31, 2022, were retrospectively reviewed. The inclusion criteria were patients with pathologically confirmed synchronous axillary LNM at first diagnosis and treated with neoadjuvant therapy. All patients were diagnosed by core needle biopsy (CNB) of primary breast foci, and lymph nodes were evaluated by needle biopsy if clinically positive or by sentinel lymph node biopsy (SLNB) if clinically negative or needle biopsy negative. The exclusion criteria were as follows: (1) multifocal primary invasive breast cancer lesion with an inconsistent ER, PR, HER2 or Ki67 status; (2) no standardized neoadjuvant therapy or surgery; (3) occult breast cancer; (4) patients only undergoing neoadjuvant endocrine therapy; (5) unavailable ER, PR, HER2 or Ki67 status and inability to retest.
Clinicopathologic data
Clinicopathologic data, including age, menopause status, family history, clinical stage, histological grade, histological type, ER status, PR status, HER2 status, Ki67 status, and anti-tumor treatment regimens, were recorded. Clinical stage was determined according to the American Joint Committee on Cancer (AJCC) stage system (8th edition) (The American College of Surgeons 2017), based on physical examination, mammography, or ultrasonography of the breast and regional nodal at the fist diagnosis.
Immunohistochemistry (IHC) for ER, PR, HER2, and Ki67 was performed for both primary tumor and synchronous axillary LNM using the same automated IHC stainers and antibodies (Supplementary Table 1). According to the 2020 American Society of Clinical Oncology and the College of American Pathologists (ASCO/CAP) guidelines (Allison et al. 2020), ER and PR status were classified as negative (lack of any ER/PR immunoreactivity or < 1% immunoreactivity in tumor cells, with a positive internal control) or positive (≥ 1% immunoreactivity in tumor cells). Hormone receptor (HR) status was considered positive in case of ER and/or PR positivity. The evaluation of HER2 status followed the HER2 diagnostic guidelines revised by ASCO/CAP in 2013 (Wolff et al. 2013). For equivocal IHC results (IHC score 2 +), fluorescence in situ hybridization (FISH) assays were performed to test for HER2 gene amplification. Cases were considered as HER2-positive in case of IHC score 3 + and/or HER2 gene amplification by FISH, HER2-low in case of IHC score 1 + or IHC score 2 + plus the absence of HER2 gene amplification, and HER2-0 in case of IHC score zero (Tarantino et al. 2020). Ki67 was evaluated by the percentage of tumor cell nuclei with positive immunostaining, and ≥ 30% was defined as high (Nielsen et al. 2021). Histological type and grade of primary breast cancer were distinguished based on the World Health Organization (WHO) classification of breast cancer and Nottingham grading by two dedicated breast pathologists.
Neoadjuvant treatment regimens and evaluation criteria
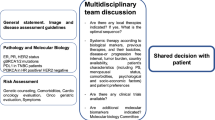
All patients received at least 4 cycles of neoadjuvant treatment which was conducted with reference to the National Comprehensive Cancer Network (NCCN) guidelines or the Chinese Society of Clinical Oncology (CSCO) guidelines. The first choice of treatment regimen was based on taxanes and/or anthracyclines. A subset of HER2-positive patients received HER2-targeted therapy with the TCHP (docetaxel/albumin-bound paclitaxel + carboplatin + trastuzumab + pertuzumab) or TCH (docetaxel/albumin-bound paclitaxel + carboplatin + trastuzumab) regimens.
Early clinical response evaluation was performed after 2–4 treatment cycles in accordance with Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 (Eisenhauer et al. 2009). Complete response (CR) and partial response (PR) were considered effective. All patients underwent local therapy involving either lumpectomy (breast-conserving surgery) or total mastectomy after completion of neoadjuvant treatment, and pathological response was evaluated using Miller-Payne grading system (Ogston et al. 2003). According to the recommendation of Collaborative Trials in Neoadjuvant Breast Cancer (CTNeoBC), pathological complete response (pCR) was defined as the absence of invasive carcinoma in both breast and axillary lymph nodes, irrespective of ductal carcinoma in situ (ypT0/TisypN0) (Cortazar et al. 2014).
Statistical analysis
Measurement data were described using the median and interquartile range (IQR) values; count and ranked data were described using the number of cases and percentages. Differences of biomarker status between matched pairs of primary breast cancer and synchronous axillary LNM were evaluated using McNemar-Bowker test. Cohen kappa statistic was calculated to estimate the overall agreement of biomarker status between the primary tumor and LNM. Kappa-values > 0.8, between 0.6 and 0.8, between 0.4 and 0.6, between 0.2 and 0.4, and < 0.2 were classified as very good, good, moderate, fair and poor agreement, respectively. Pearson’s χ2 test or Fisher’s exact test was used for univariate analysis and factors with p < 0.05 were included in the multivariate analysis. Logistic regression was performed to calculated the odds ratio (OR) and corresponding 95% confidence interval (CI). All tests were two-sided and a criterion of p < 0.05 was used for significance. All statistical analysis were performed using R 4.3.2 (http://www.r-project.org).
Results
Baseline clinicopathological characteristics
A total of 833 patients with early invasive breast cancer received neoadjuvant therapy at Peking University First Hospital from January 1, 2013 to December 31, 2022. After the exclusion of ineligible cases, 358 cases with complete data were enrolled in this study (Fig. 1). All the patients were women. The median age of our cohort was 51 years (IQR 42.3–58.0) and 172 patients (48.0%) were postmenopausal when diagnosed with breast cancer. The majority of patients had tumors of ductal histology (n = 319, 89.1%) and poor differentiation (G3, n = 176, 49.2%) on baseline biopsy. There were 294 patients (82.1%) with primary tumor larger than 2.0 cm and 328 patients had clinical positive axillary lymph nodes. More than half of the cases (n = 197, 55.0%) underwent combination anthracycline/taxane based neoadjuvant chemotherapy and 146 patients (40.8%) received anti-HER2 blockade associated with neoadjuvant chemotherapy. Seventy-six patients achieved pCR after neoadjuvant therapy for a pCR rate of 21.2%. The baseline characteristics of the overall population were shown in Table 1.
Discordance in biomarker status between primary breast cancer and LNM
The majority of the primary breast cancer and LNM were ER-Positive (n = 213, 59.5%), PR-Negative (n = 190, 53.1%) and HER2-Positive (n = 156, 43.6%), and so it is with LNM (Table 2). A receptor change occurred either as a receptor gain or as a receptor loss from primary tumor to metastasis (Fig. 2). Discordance in ER status was observed in 21 patients (5.9%, p = 0.663), with ER-gain conversion in 12 patients (3.4%) and ER-loss conversion in 9 patients (2.5%). PR status conversion was detected in 31 of cases (8.7%, p = 0.012), with PR-gain conversion in 8 patients (2.2%) and PR-loss conversion in 23 patients (6.4%). The overall discordance rate of HER2 was 17.3% (n = 45, p = 0.031), most driven by cases switching to or from HER2-low expression. In 18 of the cases (5.0%), HER2 status had changed from HER2-0 in primary tumor to HER2-low in metastatic lesions (23.1% of the HER2-0 primary breast cancer cohort), and in 17 of the cases (4.7%), HER2 status had changed from HER2-low to HER2-0 (13.7% of the HER2-low primary breast cancer cohort). Ki67 changed from low in the primary tumor to high status in LNM for 22 patients (6.1%), while changes from high to low were observed in 40 patients (11.2%). In total, the subtype of the LNM was different in 34 cases (9.5%) compared with paired primary breast cancer (Fig. 3).
Analysis of factors associated with biomarker discordance
Clinical and pathological factors were tested to search for correlation with the biomarker alterations (Table 3). The discordance rate of HR and HER2 appeared similar across different biopsy method of lymph node. HR discordance was observed more frequently when the ER status (p = 0.023) or PR status (p = 0.010) of primary tumor was negative, while HER2 discordance seemed to be more frequent when the HER2 status of primary tumor was HER2-0 or HER2-low (p < 0.001). Tumor stage, histological grade and histological type had no correlation with receptors conversion.
In univariate analysis, positive ER status of primary tumor (21.1% vs. 11.7%, p = 0.030), positive PR status of primary tumor (22.0% vs. 13.2%, p = 0.038), low Ki67 expression (34.9% vs. 13.6, p < 0.001), and the application of SLNB (31.0% vs. 15.5%, p = 0.023), showed association with the change of Ki67 expression between primary breast cancer and axillary LNM. In multivariate analysis, low Ki67 expression of primary tumor (OR 3.15[1.67–5.90], p < 0.001) and the application of SLNB (OR 2.40[1.11–5.01], p = 0.022), remained independent factors that were predictive of the alteration in Ki67 expression.
Exploratory analysis of neoadjuvant therapy response
The evaluation of pCR was conducted on a total of 358 patients, while 19 patients had missing assessments of early clinical response. Exploratory analysis did not reveal any statistically significant difference in neither pathological nor early clinical response to neoadjuvant therapy between the concordant and discordant groups for HR status (Fig. 4). Pathological complete response in concordant vs. discordant groups for HER2 status was observed in 72 of 313 patients vs. 4 of 45 patients (23.0% vs. 8.9%, p = 0.030, Fig. 4). However, no significant difference in early clinical response was observed according to the concordance of HER2 status (47.2% vs. 32.5%, p = 0.080, Fig. 4).
In addition, the subgroup analysis was performed considering the impact of the receptor status in primary breast cancer. Among patients with HR-negative primary tumor, gain of HR-positivity (negative to positive) was associated with a tendency to have lower pCR rate, although the difference between groups was not statistically significant (36.0% vs. 15.4%, p = 0.218, Fig. 5). A significantly increased pCR rate was found in patients with loss of HR-positivity (positive to negative), compared to those with stable positive HR expression (50% vs. 11.1%, p = 0.0017, Fig. 5). When evaluating the potential impact of HER2 expression change in HER2-low cases on the neoadjuvant therapy response, there was no pCR difference for concordant HER2-0 vs. gain of HER2-low expression (15.3% vs. 5.6%, p = 0.437, Fig. 5) or concordant HER2-low vs. loss of HER2-low expression (12.1% vs. 5.9%, p = 0.690, Fig. 5).
The influence of biomarker conversion on neoadjuvant therapy response according to primary tumor subtypes. A pCR in HR-negative primary breast cancer. B pCR in HR-positive primary breast cancer. C pCR in HER-0 primary breast cancer. D pCR in HER2-low primary breast cancer. HR hormone receptor, HER2 human epidermal growth factor 2
The evolution of HER2 expression from baseline biopsy to residual disease after neoadjuvant therapy in patients failing to achieve pCR was analyzed. In particular, among the 17 non-pCR cases with HER2-0 primary tumor and HER2-low axillary LNM, more than a third exhibited HER2-low residual disease which consistent with axillary LNM (Supplementary Table 2).
Discussion
The instability of ER, PR, HER2, and Ki67 expression during the progression of breast cancer have been widely reported, but the primary focus was on postoperative locoregional recurrence or distant metastasis. In our retrospective cohort of 358 breast cancer patients undergoing neoadjuvant treatment, evolution of biomarker expression from primary tumor to synchronous axillary LNM was explored using baseline biopsy specimens instead of the tumor tissue obtained from radical surgery. Change of ER, PR, HER2, and Ki67 expression was observed in 5.9%, 8.7%, 12.6%, and 17.3% of patients, respectively. Therefore, ER appeared to be most stable receptor, whereas HER2-low expression is highly unstable during disease evolution. Our findings demonstrated instability in clinically used markers throughout tumor progression in early stage, which eliminated the impact of selective pressure induced by anti-tumor treatment.
Compared to the similar studies, the discordance rate of HR was relatively low in our cohort, while changes of HER2 statues in axillary LNM were perceived more frequently. Various discordance rates reported were 1.1–28.8%, 10.6–31.7%, and 2.9–15.9% for ER, PR, and HER2, respectively (Ba et al. 2014; Falck et al. 2010; Janeva et al. 2023; Kinoe et al. 2018; Li et al. 2016; Sujarittanakarn et al. 2020; Weydandt et al. 2022; Zhao et al. 2015). This wide variability of the concordance rates can be associated with the heterogeneity in patient characteristics, biopsy method, or cut-off values for biomarkers. All patients in analysis received neoadjuvant therapy, meaning a higher proportion of HER2-positive and triple-negative subtype in our cohort. And the present study firstly adopted the HER2-low as a distinct category in analyzing receptors discordance between primary breast cancer and synchronous axillary LNM, which may result in elevated discordance rate of HER2. Especially, several previous studies included axillary lymph node specimens that were surgically removed after systemic treatment (Weydandt et al. 2022; Zhao et al. 2015).
Tissue sampling and assay method may be one of explanations for the difference between primary breast cancer and paired metastases in lymph node. Although adequate specimens were obtained from ultrasound-guided CNB and the biopsy method of axillary lymph node was not a predictive factor for ER, PR, and HER2 conversion in our study, the limitations of needle biopsy should not be disregarded (Chen et al. 2012). To minimize the variation potentially caused by assay techniques, the cases included in our study were limited within the past ten years and all assays in our laboratory were performed following proper guidelines. Given that IHC is observer-dependent and semiquantitative, the possibility to perform mRNA testing by real-time quantitative polymerase chain reaction (qPCR) as alternative to IHC to reduce the variability deserves further investigation (Marchio et al. 2021). In clinical practice, however, IHC remains the gold standard for diagnostic purposes.
Biomarker conversion in metastatic breast cancer should be seen more as a true biological phenomenon and not solely the result of limited accuracy of technique. It has been shown that primary breast cancers demonstrate intra-tumor heterogeneity with genetically distinct cellular populations formation as they evolve (Dentro et al. 2021). Genetic changes and phenotypic plasticity may also be involved in subclonal expansion and spread of disseminated tumor cells (DTCs) with various invasion ability. Adapting the epigenetic, transcriptional, and post-transcriptional landscapes is required for metastatic cells to undergo each step of the metastatic cascade (Gerstberger et al. 2023). Actually, breast cancer tends to preferentially relapse in certain organs although DTCs can spread to virtually all organs. Each organ varies in vascular and nutrient supply, immune microenvironment, and stromal composition, thus brings difference influence for infiltrating cancer cells (Obenauf and Massague 2015). This view is supported by the different receptors conversion rates among different metastatic sites and the discordance in receptor profiles among metastatic sites in cases with multi-organ metastasis (Schrijver et al. 2018). Tumor draining lymph node, especially, has been demonstrated as a critical site for inducing tumor immunosuppression. Overall, intrinsic cancer cell traits and composition of host-organ microenvironments together form the metastatic tumors with characteristics different from those of the primary.
The clinical implication of this instability in locally advanced breast cancer is important, whereas gain of HER2 and HR generally means sensitivity to trastuzumab/pertuzumab and endocrine therapy, respectively. In our cohort, the ER positive rates did not show any significant difference between primary tumors and paired axillary LNMs (p = 0.663). In line with other studies, a change of PR was observed more frequently than an ER change in our study, as well as changes of positive to negative PR (6.4%) versus negative to positive (2.2%) were perceived more often (Dieci et al. 2013; Liedtke et al. 2009; Shiino et al. 2016). As an ER-dependent gene product, PR loss in breast cancer metastases without changes in ER status observed is of uncertain clinical significance, as ER is generally considered a stronger indicator of response to endocrine therapy. Our results suggested that patients showing HR conversion responded to neoadjuvant chemotherapy better than patients who remained ER or PR positive in their axillary lymph node metastasis. Meanwhile, loss of HR expression was associated with a significant worse overall survival in previous studies focused on distant metastasis (Dieci et al. 2013; Lindstrom et al. 2012). Overall, a change of HR status during the progression of breast cancer indicates specific biology features, rather than a fortuitous events. The relevance of this phenomenon may be more pronounced in the context of neoadjuvant endocrine therapy, but further research is needed to answer this question.
The evolution of HER2 expression from primary breast cancer to axillary LNMs deserves more attention because of the introduction of the newly proposed HER2-low category. In our study, the overall rate of HER2 discordance was 12.6%, mostly represented by HER2-0 switching to HER2-low (5.0%) and HER2-low switching to HER2-0 (4.7%). Such high instability of HER2-low expression during disease evolution has been reported in advanced disease stage (Bergeron et al. 2023; Miglietta et al. 2021). Despite the hypothesis that the complex crosstalk between HR and HER2 pathways, HR status of primary tumor did not show any association with HER2 heterogeneity. A significantly decrease in pCR rate was observed in patients with unstable HER2 status, but not in the HER2-0/HER2-low subgroup. The possible explanation for such observation is that the instability was mostly driven by cases with HER2-0/HER2-low phenotype, which is known to be not appropriate for trastuzumab/pertuzumab. Actually, HER2-low status is not an independent predictor of pCR in current neoadjuvant setting, while a limited number of cases experience the conversion from HER2-negative to HER2-positive (Li et al. 2023). So, it is appropriate to determine the administration of neoadjuvant anti-HER2 targeted therapy based on the HER2 status of the primary tumor at present stage. However, the use of anti-HER2 ADCs in the treatment of early HER2-low breast cancer is still far from implementation in the clinical practice, which may obscure the clinical implication of evolution of HER2-low in locally advanced breast cancer.
It should be noted that the ASCO/CAP guideline recommendations were optimized to identify HER2-positive tumors (Anderson et al. 2023). Before the development of ADCs, HER2 IHC 0 and 1 + scores were both considered to be HER2-negative, and discriminating between the two had no clinical implications. So, it is not surprising that the scoring accuracy for HER2 IHC in the low range (0 and 1 +) is suboptimal (Fernandez et al. 2022). The research findings related to HER2-low should be reviewed with caution before new clinical applicable assays to reproducibly identify HER2-low tumors is provided.
Our study presented the largest cohort to provide additional date on receptor conversion in axillary lymph node metastasis of breast cancer, and investigate the predictive value of this instability on neoadjuvant treatment for the first time. However, this study has the following limitations. First, this was a single-institution retrospective study based on medical records. Second, the sample size was considered to be relatively low because of the low discordant rate, although many of the studies discussing this topic had cohorts with less than 200 patients. Third, we excluded ninety-four patients with unavailable ER, PR, HER2, or Ki67 status, which may introduce selection bias. However, most of these patients were diagnosed by fine needle aspiration (FNB), and the specimens were actually insufficient to preform accurate IHC. Another limitation of the present study is the lack of long-term prognostic information and molecular data (e.g., PAM50), which is a topic with worthy of researching farther.
Conclusion
Receptor discordance between primary tumor and synchronous axillary LNM appears to already exist before any anti-tumor therapy, which might reflect intra-tumor heterogeneity and phenotypic plasticity of breast cancer. The instability of ER, PR, and HER2 expression has limited clinical impact on neoadjuvant therapy at current stage, but further investigation is warranted with the incremental application of endocrine drugs and ADCs in neoadjuvant therapy.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, Hayes DF, Lakhani SR, Chavez-MacGregor M, Perlmutter J et al (2020) Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J Clin Oncol 38:1346–1366
Anderson S, Bartow BB, Siegal GP, Huang X, Wei S (2023) The dynamics of HER2-low expression during breast cancer progression. Breast Cancer Res Treat 201:437–446
Ba JL, Liu CG, Jin F (2014) Alterations in hormonal receptor expression and HER2 status between primary breast tumors and paired nodal metastases: discordance rates and prognosis. Asian Pac J Cancer Prev 15:9233–9239
Bergeron A, Bertaut A, Beltjens F, Charon-Barra C, Amet A, Jankowski C, Desmoulins I, Ladoire S, Arnould L (2023) Anticipating changes in the HER2 status of breast tumours with disease progression-towards better treatment decisions in the new era of HER2-low breast cancers. Br J Cancer 129:122–134
Chen X, Yuan Y, Gu Z, Shen K (2012) Accuracy of estrogen receptor, progesterone receptor, and HER2 status between core needle and open excision biopsy in breast cancer: a meta-analysis. Breast Cancer Res Treat 134:957–967
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384:164–172
Dentro SC, Leshchiner I, Haase K, Tarabichi M, Wintersinger J, Deshwar AG, Yu K, Rubanova Y, Macintyre G, Demeulemeester J et al (2021) Characterizing genetic intra-tumor heterogeneity across 2,658 human cancer genomes. Cell 184(2239–2254):e2239
Dieci MV, Barbieri E, Piacentini F, Ficarra G, Bettelli S, Dominici M, Conte PF, Guarneri V (2013) Discordance in receptor status between primary and recurrent breast cancer has a prognostic impact: a single-institution analysis. Ann Oncol 24:101–108
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Falck AK, Ferno M, Bendahl PO, Ryden L (2010) Does analysis of biomarkers in tumor cells in lymph node metastases give additional prognostic information in primary breast cancer? World J Surg 34:1434–1441
Fernandez AI, Liu M, Bellizzi A, Brock J, Fadare O, Hanley K, Harigopal M, Jorns JM, Kuba MG, Ly A et al (2022) Examination of Low ERBB2 Protein Expression in Breast Cancer Tissue. JAMA Oncol 8:1–4
Gerstberger S, Jiang Q, Ganesh K (2023) Metastasis Cell 186:1564–1579
Gradishar WJ, Moran MS, Abraham J, Abramson V, Aft R, Agnese D, Allison KH, Anderson B, Burstein HJ, Chew H et al (2023) NCCN Guidelines(R) Insights: Breast Cancer, Version 4.2023. J Natl Compr Canc Netw 21:594–608
Janeva S, Parris TZ, Krabbe E, Sundquist M, Karlsson P, Audisio RA, Olofsson Bagge R, Kovacs A (2023) Clinical relevance of biomarker discordance between primary breast cancers and synchronous axillary lymph node metastases. Clin Exp Metastasis 40:299–308
Kinoe H, Yamanouchi K, Kuba S, Morita M, Sakimura C, Kanetaka K, Takatsuki M, Abe K, Yano H, Matsumoto M et al (2018) Discordance of hormone receptor, human epidermal growth factor receptor-2, and Ki-67 between primary breast cancer and synchronous axillary lymph node metastasis. J BUON 23:60–66
Li MH, Hou CL, Wang C, Sun AJ (2016) HER-2, ER, PR status concordance in primary breast cancer and corresponding metastatic lesion in lymph node in Chinese women. Pathol Res Pract 212:252–257
Li Y, Maimaitiaili A, Qu F, Li G, Shi B, Wang Y, Zhang J, He J, Fan Z, Zhang H (2023) Effect of HER2-low-positive status on neoadjuvant chemotherapy and survival outcome of breast cancer: a 10-year dual-center retrospective study. Am J Cancer Res 13:3571–3581
Liedtke C, Broglio K, Moulder S, Hsu L, Kau SW, Symmans WF, Albarracin C, Meric-Bernstam F, Woodward W, Theriault RL et al (2009) Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 20:1953–1958
Lindstrom LS, Karlsson E, Wilking UM, Johansson U, Hartman J, Lidbrink EK, Hatschek T, Skoog L, Bergh J (2012) Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol 30:2601–2608
Marchio C, Annaratone L, Marques A, Casorzo L, Berrino E, Sapino A (2021) Evolving concepts in HER2 evaluation in breast cancer: Heterogeneity, HER2-low carcinomas and beyond. Semin Cancer Biol 72:123–135
Mellouli M, Graja S, Kridis WB, Ayed HB, Makni S, Triki M, Charfi S, Khanfir A, Boudawara TS, Kallel R (2022) Discordance in receptor status between primary and metastatic breast cancer and overall survival: A single-center analysis. Ann Diagn Pathol 61:152044
Miglietta F, Griguolo G, Bottosso M, Giarratano T, Lo Mele M, Fassan M, Cacciatore M, Genovesi E, De Bartolo D, Vernaci G et al (2021) Evolution of HER2-low expression from primary to recurrent breast cancer. NPJ Breast Cancer 7:137
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, Tsurutani J, Ueno NT, Prat A, Chae YS et al (2022) Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med 387:9–20
Nielsen TO, Leung SCY, Rimm DL, Dodson A, Acs B, Badve S, Denkert C, Ellis MJ, Fineberg S, Flowers M et al (2021) Assessment of Ki67 in Breast Cancer: Updated Recommendations From the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst 113:808–819
Obenauf AC, Massague J (2015) Surviving at a Distance: Organ-Specific Metastasis. Trends Cancer 1:76–91
Ogston KN, Miller ID, Payne S, Hutcheon AW, Sarkar TK, Smith I, Schofield A, Heys SD (2003) A new histological grading system to assess response of breast cancers to primary chemotherapy: prognostic significance and survival. Breast 12:320–327
Rugo HS, Rumble RB, Macrae E, Barton DL, Connolly HK, Dickler MN, Fallowfield L, Fowble B, Ingle JN, Jahanzeb M et al (2016) Endocrine therapy for hormone receptor-positive metastatic breast cancer: American society of clinical oncology guideline. J Clin Oncol 34:3069–3103
Schrijver W, Suijkerbuijk KPM, van Gils CH, van der Wall E, Moelans CB, van Diest PJ (2018) Receptor conversion in distant breast cancer metastases: a systematic review and meta-analysis. J Natl Cancer Inst 110:568–580
Shiino S, Kinoshita T, Yoshida M, Jimbo K, Asaga S, Takayama S, Tsuda H (2016) Prognostic impact of discordance in hormone receptor status between primary and recurrent sites in patients with recurrent breast cancer. Clin Breast Cancer 16:e133-140
Shiino S, Ball G, Syed BM, Kurozumi S, Green AR, Tsuda H, Takayama S, Suto A, Rakha EA (2022) Prognostic significance of receptor expression discordance between primary and recurrent breast cancers: a meta-analysis. Breast Cancer Res Treat 191:1–14
Siegel RL, Miller KD, Wagle NS, Jemal A (2023) Cancer statistics, 2023. CA Cancer J Clin 73:17–48
Sujarittanakarn S, Himakhun W, Worasawate W, Prasert W (2020) The Case to Case Comparison of Hormone Receptors and HER2 Status between Primary Breast Cancer and Synchronous Axillary Lymph Node Metastasis. Asian Pac J Cancer Prev 21:1559–1565
Tarantino P, Hamilton E, Tolaney SM, Cortes J, Morganti S, Ferraro E, Marra A, Viale G, Trapani D, Cardoso F et al (2020) HER2-Low Breast Cancer: Pathological and Clinical Landscape. J Clin Oncol 38:1951–1962
The American College of Surgeons (2017) AJCC Cancer Staging Manual. Springer, Berlin
Weydandt L, Nel I, Kreklau A, Horn LC, Aktas B (2022) Heterogeneity between Core Needle Biopsy and Synchronous Axillary Lymph Node Metastases in Early Breast Cancer Patients-A Comparison of HER2, Estrogen and Progesterone Receptor Expression Profiles during Primary Treatment Regime. Cancers (basel) 14(8):1863
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013
Zhao S, Xu L, Liu W, Lv C, Zhang K, Gao H, Wang J, Ma R (2015) Comparison of the expression of prognostic biomarkers between primary tumor and axillary lymph node metastases in breast cancer. Int J Clin Exp Pathol 8:5744–5748
Acknowledgements
Not applicable.
Funding
This work is supported by Beijing Health Technologies Promotion Program (BHTPP2022067). The funders had no role in the study design, data collection, analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
MD and LX contributed to conception and design of the study. MD, ML, and QL performed the data analysis and interpretation. MD wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Biomedical Research Ethics Committee of Peking University First Hospital (No. 2024 research 111–002).
Consent to participate and publish
Patient consent was waived as this was a retrospective cohort study. All data were analyzed and published anonymously.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ding, M., Li, M., Liu, Q. et al. Biomarker conversion from primary breast cancer to synchronous axillary lymph node metastasis and neoadjuvant therapy response: a single-center analysis. J Cancer Res Clin Oncol 150, 297 (2024). https://doi.org/10.1007/s00432-024-05834-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05834-y