Abstract
With the advancement of imaging technology, systemic disease control rate and survival rate, the morbidity of brain metastases (BMs) from non-small cell lung cancer (NSCLC) has been riding on a steady upward trend (40%), but management of BMs from NSCLC remains obscure. Systemic therapy is anticipated to offer novel therapeutic avenues in the management of NSCLC BMs, and radiotherapy (RT) and immunotherapy have their own advantages. Recently, it was confirmed that immune checkpoint inhibitors (ICIs) and RT could mutually promote the efficacy in the treatment of BMs from NSCLC. In this paper, we provide a review on current understandings and practices of separating or combining ICIs and RT, which could provide a reference for the coming laboratory and clinical studies and contribute to the development of new approaches in NSCLC BMs.

Similar content being viewed by others
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- BMs:
-
Brain metastases
- DCR:
-
Disease control rate
- SRS–SRT:
-
Stereotactic radiosurgery–stereotactic radiotherapy
- BBB:
-
Blood–brain barrier
- WBRT:
-
Whole brain radiotherapy
- EGFR:
-
Epidermal growth factor receptors
- ALK:
-
Anaplastic lymphoma kinase
- TKIs:
-
Tyrosine kinase inhibitors
- CNS:
-
Central nervous system
- RRs:
-
Response rates
- OS:
-
Overall survival
- RT:
-
Radiotherapy
- ICIs:
-
Immune checkpoint inhibitors
- RN:
-
Radiation necrosis
- LR:
-
Local recurrence
- TCP:
-
Tumor control
- HFSRT:
-
Hypofractionated stereotactic radiation therapy
- PS:
-
Performance status
- HR:
-
Hazard ratio
- RCT:
-
Randomized controlled studies
- LMC:
-
Leptomeningeal carcinomatosis
- HVLT-R DR:
-
Hopkins Verbal Learning Test-Revised Delayed Recall
- HS-WBRT:
-
Hippocampal-sparing whole brain radiotherapy
- RTOG:
-
Radiation Therapy Oncology Group
- QOL:
-
Quality-of-life
- EORTC:
-
European Organization for Research and Treatment of Cancer
- BTR:
-
Brain tumor recurrence
- TME:
-
Tumor microenvironment
- ECM:
-
Extracellular matrix
- APC:
-
Antigen-presenting cell
- PD-1:
-
Programmed cell death-1
- PD-L1:
-
Programmed cell death-ligand 1
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated antigen-4
- TILs:
-
Tumor-infiltrating lymphocytes
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- IORR:
-
Intracerebral objective response rate
- PFS:
-
Progression-free survival
- AEs:
-
Adverse events
- Tregs:
-
Regulatory T cells
- Anti-CTLA-4:
-
CTLA-4-blocking antibody
- 18F-FDG PET/CT:
-
18F-flurodeoxyglucose positron emission tomography/computed tomography
- IF:
-
In-fields
- KM:
-
Kaplan–Meier
- RCC:
-
Renal cell carcinoma
- RICT:
-
Radiation-induced cardiotoxicity
References
Ahmed KA et al (2017) Outcomes targeting the PD-1/PD-L1 axis in conjunction with stereotactic radiation for patients with non-small cell lung cancer brain metastases. J Neurooncol 133:331–338. https://doi.org/10.1007/s11060-017-2437-5
Aldarouish M, Wang C (2016) Trends and advances in tumor immunology and lung cancer immunotherapy. J Exp Clin Cancer Res 35:157. https://doi.org/10.1186/s13046-016-0439-3
Aoyama H et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491. https://doi.org/10.1001/jama.295.21.2483
Aoyama H, Tago M, Shirato H (2015) Stereotactic radiosurgery with or without whole-brain radiotherapy for brain metastases: secondary analysis of the JROSG 99-1 randomized clinical trial. JAMA Oncol 1:457–464. https://doi.org/10.1001/jamaoncol.2015.1145
Berghoff AS et al (2016) Density of tumor-infiltrating lymphocytes correlates with extent of brain edema and overall survival time in patients with brain metastases. Oncoimmunology 5:e1057388. https://doi.org/10.1080/2162402x.2015.1057388
Bi WL et al (2019) Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin. https://doi.org/10.3322/caac.21552
Bjornhart B, Hansen KH, Jorgensen TL, Herrstedt J, Schytte T (2019) Efficacy and safety of immune checkpoint inhibitors in a Danish real life non-small cell lung cancer population: a retrospective cohort study. Acta Oncol (Stockholm, Sweden) 58:953–961. https://doi.org/10.1080/0284186x.2019.1615636
Borgelt B et al (1980) The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 6:1–9
Borghaei H et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373:1627–1639. https://doi.org/10.1056/NEJMoa1507643
Botticelli A et al (2018) Can IDO activity predict primary resistance to anti-PD-1 treatment in NSCLC? J Transl Med 16:219. https://doi.org/10.1186/s12967-018-1595-3
Brahmer J et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373:123–135. https://doi.org/10.1056/NEJMoa1504627
Britschgi C, Riesterer O, Burger IA, Guckenberger M, Curioni-Fontecedro A (2018) Report of an abscopal effect induced by stereotactic body radiotherapy and nivolumab in a patient with metastatic non-small cell lung cancer. Radiat Oncol (London, England) 13:102. https://doi.org/10.1186/s13014-018-1049-3
Brown PD et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316:401–409. https://doi.org/10.1001/jama.2016.9839
Chang EL et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. https://doi.org/10.1016/s1470-2045(09)70263-3
Chen Y et al (2016) First-line epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitor alone or with whole-brain radiotherapy for brain metastases in patients with EGFR-mutated lung adenocarcinoma. Cancer Sci 107:1800–1805. https://doi.org/10.1111/cas.13079
Chen L et al (2018) Concurrent immune checkpoint inhibitors and stereotactic radiosurgery for brain metastases in non-small cell lung cancer, melanoma, and renal cell carcinoma. Int J Radiat Oncol Biol Phys 100:916–925. https://doi.org/10.1016/j.ijrobp.2017.11.041
Christodoulou C et al (2017) Lapatinib with whole brain radiotherapy in patients with brain metastases from breast and non-small cell lung cancer: a phase II study of the Hellenic Cooperative Oncology Group (HeCOG). J Neurooncol 134:443–451. https://doi.org/10.1007/s11060-017-2548-z
Churilla TM et al (2017a) Whole brain radiotherapy after stereotactic radiosurgery or surgical resection among patients with one to three brain metastases and favorable prognoses: a secondary analysis of EORTC 22952-26001. Ann Oncol 28:2588–2594. https://doi.org/10.1093/annonc/mdx332
Churilla TM et al (2017b) Stereotactic radiosurgery with or without whole-brain radiation therapy for limited brain metastases: a secondary analysis of the North Central Cancer Treatment Group N0574 (Alliance) randomized controlled trial. Int J Radiat Oncol Biol Phys 99:1173–1178. https://doi.org/10.1016/j.ijrobp.2017.07.045
Collen C et al (2014) Phase II study of stereotactic body radiotherapy to primary tumor and metastatic locations in oligometastatic nonsmall-cell lung cancer patients. Ann Oncol 25:1954–1959. https://doi.org/10.1093/annonc/mdu370
Dagogo-Jack I, Gill CM, Cahill DP, Santagata S, Brastianos PK (2017) Treatment of brain metastases in the modern genomic era. Pharmacol Ther 170:64–72. https://doi.org/10.1016/j.pharmthera.2016.10.011
Demaria S, Golden EB, Formenti SC (2015) Role of local radiation therapy in cancer immunotherapy. JAMA Oncol 1:1325–1332. https://doi.org/10.1001/jamaoncol.2015.2756
Deng L et al (2014) Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Investig 124:687–695. https://doi.org/10.1172/jci67313
Doherty MK et al (2017) Treatment options for patients with brain metastases from EGFR/ALK-driven lung cancer. Radiother Oncol 123:195–202. https://doi.org/10.1016/j.radonc.2017.03.007
Doi H et al (2019) Neutrophil-to-lymphocyte ratio predicts survival after whole-brain radiotherapy in non-small cell lung cancer. In vivo (Athens, Greece) 33:195–201. https://doi.org/10.21873/invivo.11459
Dong H et al (2002) Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med 8:793–800. https://doi.org/10.1038/nm730
Dovedi SJ et al (2014) Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res 74:5458–5468. https://doi.org/10.1158/0008-5472.can-14-1258
Du S et al (2018) PD-1 modulates radiation-induced cardiac toxicity through cytotoxic T lymphocytes. J Thorac Oncol 13:510–520. https://doi.org/10.1016/j.jtho.2017.12.002
Dudnik E et al (2016) Intracranial response to nivolumab in NSCLC patients with untreated or progressing CNS metastases. Lung Cancer 98:114–117. https://doi.org/10.1016/j.lungcan.2016.05.031
Freeman GJ et al (2000) Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med 192:1027–1034
Fridman WH, Pages F, Sautes-Fridman C, Galon J (2012) The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 12:298–306. https://doi.org/10.1038/nrc3245
Fuentes R et al (2018) Surgery versus stereotactic radiotherapy for people with single or solitary brain metastasis. Cochrane Database Syst Rev 8:CD012086. https://doi.org/10.1002/14651858.cd012086.pub2
Garon EB et al (2015) Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 372:2018–2028. https://doi.org/10.1056/NEJMoa1501824
Gauvain C et al (2018) Intracerebral efficacy and tolerance of nivolumab in non-small-cell lung cancer patients with brain metastases. Lung Cancer 116:62–66. https://doi.org/10.1016/j.lungcan.2017.12.008
Gerber DE et al (2017) Treatment design and rationale for a randomized trial of cisplatin and etoposide plus thoracic radiotherapy followed by nivolumab or placebo for locally advanced non-small-cell lung cancer (RTOG 3505). Clin Lung Cancer 18:333–339. https://doi.org/10.1016/j.cllc.2016.10.009
Goldberg SB et al (2016) Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol 17:976–983. https://doi.org/10.1016/s1470-2045(16)30053-5
Gondi V et al (2010a) Hippocampal-sparing whole-brain radiotherapy: a “how-to” technique using helical tomotherapy and linear accelerator-based intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 78:1244–1252. https://doi.org/10.1016/j.ijrobp.2010.01.039
Gondi V, Tome WA, Mehta MP (2010b) Why avoid the hippocampus? A comprehensive review. Radiother Oncol 97:370–376. https://doi.org/10.1016/j.radonc.2010.09.013
Gondi V et al (2014) Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol 32:3810–3816. https://doi.org/10.1200/jco.2014.57.2909
Halasz LM, Weeks JC, Neville BA, Taback N, Punglia RS (2013) Use of stereotactic radiosurgery for brain metastases from non-small cell lung cancer in the United States. Int J Radiat Oncol Biol Phys 85:e109–e116. https://doi.org/10.1016/j.ijrobp.2012.08.007
Halasz LM et al (2016) Comparative effectiveness of stereotactic radiosurgery versus whole-brain radiation therapy for patients with brain metastases from breast or non-small cell lung cancer. Cancer 122:2091–2100. https://doi.org/10.1002/cncr.30009
Hartgerink D et al (2018) Stereotactic radiosurgery in the management of patients with brain metastases of non-small cell lung cancer: indications, decision tools and future directions. Front Oncol 8:154. https://doi.org/10.3389/fonc.2018.00154
Harth S et al (2013) Estimation of intracranial failure risk following hippocampal-sparing whole brain radiotherapy. Radiother Oncol 109:152–158. https://doi.org/10.1016/j.radonc.2013.09.009
Hellman S, Weichselbaum RR (1995) Oligometastases. J Clin Oncol 13:8–10. https://doi.org/10.1200/jco.1995.13.1.8
Hellmann MD et al (2017) Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol 18:31–41. https://doi.org/10.1016/s1470-2045(16)30624-6
Hirsch FR et al (2017) Lung cancer: current therapies and new targeted treatments. Lancet (London, England) 389:299–311. https://doi.org/10.1016/s0140-6736(16)30958-8
Hodi FS (2007) Cytotoxic T-lymphocyte-associated antigen-4. Clin Cancer Res 13:5238–5242. https://doi.org/10.1158/1078-0432.ccr-07-0813
Hubbeling HG et al (2018) Safety of combined PD-1 pathway inhibition and intracranial radiation therapy in non-small cell lung cancer. J Thorac Oncol 13:550–558. https://doi.org/10.1016/j.jtho.2018.01.012
Iyengar P, Gerber DE (2013) Locally advanced lung cancer: an optimal setting for vaccines and other immunotherapies. Cancer J (Sudbury, Mass.) 19:247–262. https://doi.org/10.1097/ppo.0b013e318292e51a
Jackman D et al (2010) Clinical definition of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. J Clin Oncol 28:357–360. https://doi.org/10.1200/jco.2009.24.7049
Jiang T et al (2016) Radiotherapy plus EGFR TKIs in non-small cell lung cancer patients with brain metastases: an update meta-analysis. Cancer Med 5:1055–1065. https://doi.org/10.1002/cam4.673
Johung KL et al (2016) Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J Clin Oncol 34:123–129. https://doi.org/10.1200/jco.2015.62.0138
Kann BH, Park HS, Johnson SB, Chiang VL, Yu JB (2017) Radiosurgery for brain metastases: changing practice patterns and disparities in the United States. J Natl Compr Cancer Netw 15:1494–1502. https://doi.org/10.6004/jnccn.2017.7003
Keller A et al (2017) Hypofractionated stereotactic radiation therapy to the resection bed for intracranial metastases. Int J Radiat Oncol Biol Phys 99:1179–1189. https://doi.org/10.1016/j.ijrobp.2017.08.014
Khan M et al (2019) Whole brain radiation therapy plus stereotactic radiosurgery in the treatment of brain metastases leading to improved survival in patients with favorable prognostic factors. Front Oncol 9:205. https://doi.org/10.3389/fonc.2019.00205
Khuntia D, Brown P, Li J, Mehta MP (2006) Whole-brain radiotherapy in the management of brain metastasis. J Clin Oncol 24:1295–1304. https://doi.org/10.1200/jco.2005.04.6185
Kiess AP et al (2015) Stereotactic radiosurgery for melanoma brain metastases in patients receiving ipilimumab: safety profile and efficacy of combined treatment. Int J Radiat Oncol Biol Phys 92:368–375. https://doi.org/10.1016/j.ijrobp.2015.01.004
Ko EC, Raben D, Formenti SC (2018) The integration of radiotherapy with immunotherapy for the treatment of non-small cell lung cancer. Clin Cancer Res 24:5792–5806. https://doi.org/10.1158/1078-0432.ccr-17-3620
Kocher M et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29:134–141. https://doi.org/10.1200/jco.2010.30.1655
Langer CJ, Mehta MP (2005) Current management of brain metastases, with a focus on systemic options. J Clin Oncol 23:6207–6219. https://doi.org/10.1200/jco.2005.03.145
Laubli H et al (2017) Cerebral vasculitis mimicking intracranial metastatic progression of lung cancer during PD-1 blockade. J Immunother Cancer 5:46. https://doi.org/10.1186/s40425-017-0249-y
Lesueur P et al (2018) Safety of combined PD-1 pathway inhibition and radiation therapy for non-small-cell lung cancer: a multicentric retrospective study from the GFPC. Cancer Med 7:5505–5513. https://doi.org/10.1002/cam4.1825
Levy A et al (2013) Radiation therapy and immunotherapy: implications for a combined cancer treatment. Crit Rev Oncol/Hematol 85:278–287. https://doi.org/10.1016/j.critrevonc.2012.09.001
Levy A, Massard C, Soria JC, Deutsch E (2016) Concurrent irradiation with the anti-programmed cell death ligand-1 immune checkpoint blocker durvalumab: single centre subset analysis from a phase 1/2 trial. Eur J Cancer 68:156–162. https://doi.org/10.1016/j.ejca.2016.09.013
Levy A et al (2018) Diversity of brain metastases screening and management in non-small cell lung cancer in Europe: results of the European Organisation for Research and Treatment of Cancer Lung Cancer Group survey. Eur J Cancer 93:37–46. https://doi.org/10.1016/j.ejca.2018.01.067
Li YS et al (2016) Leptomeningeal metastases in patients with NSCLC with EGFR mutations. J Thorac Oncol 11:1962–1969. https://doi.org/10.1016/j.jtho.2016.06.029
Liao BC, Lin CC, Yang JC (2018) Treating brain metastases in non-small cell lung cancer patients: what have we learnt from pharmaceutical recent clinical trials? Expert Opin Pharmacother 19:851–864. https://doi.org/10.1080/14656566.2018.1472765
Linskey ME et al (2010) The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:45–68. https://doi.org/10.1007/s11060-009-0073-4
Ma TM et al (2017) A prospective evaluation of hippocampal radiation dose volume effects and memory deficits following cranial irradiation. Radiother Oncol 125:234–240. https://doi.org/10.1016/j.radonc.2017.09.035
Maemondo M et al (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362:2380–2388. https://doi.org/10.1056/NEJMoa0909530
Magnuson WJ et al (2016) Impact of deferring radiation therapy in patients with epidermal growth factor receptor-mutant non-small cell lung cancer who develop brain metastases. Int J Radiat Oncol Biol Phys 95:673–679. https://doi.org/10.1016/j.ijrobp.2016.01.037
Magnuson WJ et al (2017) Management of brain metastases in tyrosine kinase inhibitor-naive epidermal growth factor receptor-mutant non-small-cell lung cancer: a retrospective multi-institutional analysis. J Clin Oncol 35:1070–1077. https://doi.org/10.1200/jco.2016.69.7144
Mak KS et al (2015) Significance of targeted therapy and genetic alterations in EGFR, ALK, or KRAS on survival in patients with non-small cell lung cancer treated with radiotherapy for brain metastases. Neuro-oncology 17:296–302. https://doi.org/10.1093/neuonc/nou146
Mansfield AS et al (2016) Temporal and spatial discordance of programmed cell death-ligand 1 expression and lymphocyte tumor infiltration between paired primary lesions and brain metastases in lung cancer. Ann Oncol 27:1953–1958. https://doi.org/10.1093/annonc/mdw289
Mansfield AS et al (2018) Contraction of T cell richness in lung cancer brain metastases. Sci Rep 8:2171. https://doi.org/10.1038/s41598-018-20622-8
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454:436–444. https://doi.org/10.1038/nature07205
Marchetti M et al (2019) Multisession radiosurgery for perioptic meningiomas: medium-to-long term results from a CyberKnife cooperative study. J Neurooncol 143:597–604. https://doi.org/10.1007/s11060-019-03196-x
Martin AM et al (2018) Immunotherapy and symptomatic radiation necrosis in patients with brain metastases treated with stereotactic radiation. JAMA Oncol 4:1123–1124. https://doi.org/10.1001/jamaoncol.2017.3993
Martinez P, Mak RH, Oxnard GR (2017) Targeted therapy as an alternative to whole-brain radiotherapy in EGFR-mutant or ALK-positive non-small-cell lung cancer with brain metastases. JAMA Oncol 3:1274–1275. https://doi.org/10.1001/jamaoncol.2017.1047
Mehta MP et al (2002) Lead-in phase to randomized trial of motexafin gadolinium and whole-brain radiation for patients with brain metastases: centralized assessment of magnetic resonance imaging, neurocognitive, and neurologic end points. J Clin Oncol 20:3445–3453. https://doi.org/10.1200/jco.2002.07.500
Mehta MP et al (2003) Survival and neurologic outcomes in a randomized trial of motexafin gadolinium and whole-brain radiation therapy in brain metastases. J Clin Oncol 21:2529–2536. https://doi.org/10.1200/jco.2003.12.122
Minniti G et al (2016) Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (> 2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys 95:1142–1148. https://doi.org/10.1016/j.ijrobp.2016.03.013
Minniti G et al (2019) Comparative effectiveness of multi-fraction stereotactic radiosurgery for surgically resected or intact large brain metastases from non-small-cell lung cancer (NSCLC). Lung Cancer (Amsterdam, Netherlands) 132:119–125. https://doi.org/10.1016/j.lungcan.2019.04.021
Mulvenna P et al (2016) Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet (London, England) 388:2004–2014. https://doi.org/10.1016/s0140-6736(16)30825-x
Niibe Y et al (2016) Oligo-recurrence predicts favorable prognosis of brain-only oligometastases in patients with non-small cell lung cancer treated with stereotactic radiosurgery or stereotactic radiotherapy: a multi-institutional study of 61 subjects. BMC Cancer 16:659. https://doi.org/10.1186/s12885-016-2680-8
Otake S, Goto T (2019) Stereotactic radiotherapy for oligometastasis. Cancers. https://doi.org/10.3390/cancers11020133
Ou SH, Klempner SJ, Azada MC, Rausei-Mills V, Duma C (2015) Radiation necrosis presenting as pseudoprogression (PsP) during alectinib treatment of previously radiated brain metastases in ALK-positive NSCLC: implications for disease assessment and management. Lung Cancer 88:355–359. https://doi.org/10.1016/j.lungcan.2015.03.022
Ozdemir Y, Yildirim BA, Topkan E (2016) Whole brain radiotherapy in management of non-small-cell lung carcinoma associated leptomeningeal carcinomatosis: evaluation of prognostic factors. J Neurooncol 129:329–335. https://doi.org/10.1007/s11060-016-2179-9
Passariello M et al (2019) Novel human anti-PD-L1 mAbs inhibit immune-independent tumor cell growth and PD-L1 associated intracellular signalling. Sci Rep 9:13125. https://doi.org/10.1038/s41598-019-49485-3
Patchell RA (2003) The management of brain metastases. Cancer Treat Rev 29:533–540
Pentcheva-Hoang T, Corse E, Allison JP (2009) Negative regulators of T-cell activation: potential targets for therapeutic intervention in cancer, autoimmune disease, and persistent infections. Immunol Rev 229:67–87. https://doi.org/10.1111/j.1600-065X.2009.00763.x
Pike LRG et al (2017) Radiation and PD-1 inhibition: favorable outcomes after brain-directed radiation. Radiother Oncol 124:98–103. https://doi.org/10.1016/j.radonc.2017.06.006
Prabhu RS et al (2017) Single-fraction stereotactic radiosurgery (SRS) alone versus surgical resection and SRS for large brain metastases: a multi-institutional analysis. Int J Radiat Oncol Biol Phys 99:459–467. https://doi.org/10.1016/j.ijrobp.2017.04.006
Prabhu RS et al (2018) Preoperative stereotactic radiosurgery before planned resection of brain metastases: updated analysis of efficacy and toxicity of a novel treatment paradigm. J Neurosurg. https://doi.org/10.3171/2018.7.jns181293
Quail DF, Joyce JA (2013) Microenvironmental regulation of tumor progression and metastasis. Nat Med 19:1423–1437. https://doi.org/10.1038/nm.3394
Quail DF, Joyce JA (2017) The microenvironmental landscape of brain tumors. Cancer Cell 31:326–341. https://doi.org/10.1016/j.ccell.2017.02.009
Rajakesari S et al (2014) Local control after fractionated stereotactic radiation therapy for brain metastases. J Neurooncol 120:339–346. https://doi.org/10.1007/s11060-014-1556-5
Sacher AG, Gandhi L (2016) Biomarkers for the clinical use of PD-1/PD-L1 inhibitors in non-small-cell lung cancer: a review. JAMA Oncol 2:1217–1222. https://doi.org/10.1001/jamaoncol.2016.0639
Salama AK, Hodi FS (2011) Cytotoxic T-lymphocyte-associated antigen-4. Clin Cancer Res 17:4622–4628. https://doi.org/10.1158/1078-0432.ccr-10-2232
Serizawa T et al (2019) Local tumor progression treated with Gamma Knife radiosurgery: differences between patients with 2–4 versus 5–10 brain metastases based on an update of a multi-institutional prospective observational study (JLGK0901). J Neurosurg. https://doi.org/10.3171/2019.1.jns183085
Shaverdian N et al (2017) Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol 18:895–903. https://doi.org/10.1016/s1470-2045(17)30380-7
Shepard MJ et al (2019) Stereotactic radiosurgery with and without checkpoint inhibition for patients with metastatic non-small cell lung cancer to the brain: a matched cohort study. J Neurosurg. https://doi.org/10.3171/2019.4.jns19822
Shien K, Papadimitrakopoulou VA, Wistuba II (2016) Predictive biomarkers of response to PD-1/PD-L1 immune checkpoint inhibitors in non-small cell lung cancer. Lung Cancer 99:79–87. https://doi.org/10.1016/j.lungcan.2016.06.016
Shukuya T et al (2011) Continuous EGFR-TKI administration following radiotherapy for non-small cell lung cancer patients with isolated CNS failure. Lung Cancer 74:457–461. https://doi.org/10.1016/j.lungcan.2011.04.007
Shuryak I, Carlson DJ, Brown JM, Brenner DJ (2015) High-dose and fractionation effects in stereotactic radiation therapy: analysis of tumor control data from 2965 patients. Radiother Oncol 115:327–334. https://doi.org/10.1016/j.radonc.2015.05.013
Shuto T et al (2018) Multiinstitutional prospective observational study of stereotactic radiosurgery for patients with multiple brain metastases from non-small cell lung cancer (JLGK0901 study-NSCLC). J Neurosurg 129:86–94. https://doi.org/10.3171/2018.7.gks181378
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67:7–30. https://doi.org/10.3322/caac.21387
Soon YY, Leong CN, Koh WY, Tham IW (2015) EGFR tyrosine kinase inhibitors versus cranial radiation therapy for EGFR mutant non-small cell lung cancer with brain metastases: a systematic review and meta-analysis. Radiother Oncol 114:167–172. https://doi.org/10.1016/j.radonc.2014.12.011
Stamell EF, Wolchok JD, Gnjatic S, Lee NY, Brownell I (2013) The abscopal effect associated with a systemic anti-melanoma immune response. Int J Radiat Oncol Biol Phys 85:293–295. https://doi.org/10.1016/j.ijrobp.2012.03.017
Svokos KA, Salhia B, Toms SA (2014) Molecular biology of brain metastasis. Int J Mol Sci 15:9519–9530. https://doi.org/10.3390/ijms15069519
Swanton C, Govindan R (2016) Clinical implications of genomic discoveries in lung cancer. N Engl J Med 374:1864–1873. https://doi.org/10.1056/NEJMra1504688
Takamori S et al (2017) Discrepancy in programmed cell death-ligand 1 between primary and metastatic non-small cell lung cancer. Anticancer Res 37:4223–4228. https://doi.org/10.21873/anticanres.11813
Tang C et al (2017) Ipilimumab with stereotactic ablative radiation therapy: phase I results and immunologic correlates from peripheral T cells. Clin Cancer Res 23:1388–1396. https://doi.org/10.1158/1078-0432.ccr-16-1432
Teglasi V et al (2017) Evaluating the significance of density, localization, and PD-1/PD-L1 immunopositivity of mononuclear cells in the clinical course of lung adenocarcinoma patients with brain metastasis. Neuro-oncology 19:1058–1067. https://doi.org/10.1093/neuonc/now309
Tran TT et al (2019) Perilesional edema in brain metastases: potential causes and implications for treatment with immune therapy. J Immunother Cancer 7:200. https://doi.org/10.1186/s40425-019-0684-z
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015) Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol 10:1240–1242. https://doi.org/10.1097/jto.0000000000000663
Ulahannan D, Khalifa J, Faivre-Finn C, Lee SM (2017) Emerging treatment paradigms for brain metastasis in non-small-cell lung cancer: an overview of the current landscape and challenges ahead. Ann Oncol 28:2923–2931. https://doi.org/10.1093/annonc/mdx481
Vecht CJ et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33:583–590. https://doi.org/10.1002/ana.410330605
Vogelbaum MA et al (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104:907–912. https://doi.org/10.3171/jns.2006.104.6.907
Wang X, Xu Y, Tang W, Liu L (2018a) Efficacy and safety of radiotherapy plus EGFR-TKIs in NSCLC patients with brain metastases: a meta-analysis of published data. Transl Oncol 11:1119–1127. https://doi.org/10.1016/j.tranon.2018.07.003
Wang C, Lu X, Lyu Z, Bi N, Wang L (2018b) Comparison of up-front radiotherapy and TKI with TKI alone for NSCLC with brain metastases and EGFR mutation: a meta-analysis. Lung Cancer 122:94–99. https://doi.org/10.1016/j.lungcan.2018.05.014
Wang Y et al (2018c) Continued EGFR-TKI with concurrent radiotherapy to improve time to progression (TTP) in patients with locally progressive non-small cell lung cancer (NSCLC) after front-line EGFR-TKI treatment. Clin Transl Oncol 20:366–373. https://doi.org/10.1007/s12094-017-1723-1
Wang Y et al (2019) New insight on the correlation of metabolic status on (18)F-FDG PET/CT with immune marker expression in patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-019-04500-7
Xu Q et al (2018) Consolidative local ablative therapy improves the survival of patients with synchronous oligometastatic NSCLC harboring EGFR activating mutation treated with first-line EGFR-TKIs. J Thorac Oncol 13:1383–1392. https://doi.org/10.1016/j.jtho.2018.05.019
Yamamoto M et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases: a case-matched study comparing treatment results for patients with 2–9 versus 10 or more tumors. J Neurosurg 121(Suppl):16–25. https://doi.org/10.3171/2014.8.gks141421
Yang JJ et al (2017) Icotinib versus whole-brain irradiation in patients with EGFR-mutant non-small-cell lung cancer and multiple brain metastases (BRAIN): a multicentre, phase 3, open-label, parallel, randomised controlled trial. Lancet 5:707–716. https://doi.org/10.1016/s2213-2600(17)30262-x
Yang WC et al (2018) Epidermal growth factor receptor mutation predicts favorable outcomes in non-small cell lung cancer patients with brain metastases treated with stereotactic radiosurgery. Radiother Oncol 126:368–374. https://doi.org/10.1016/j.radonc.2017.10.010
Yi M et al (2018) Biomarkers for predicting efficacy of PD-1/PD-L1 inhibitors. Mol Cancer 17:129. https://doi.org/10.1186/s12943-018-0864-3
Zhu Q et al (2017) Clinical outcome of tyrosine kinase inhibitors alone or combined with radiotherapy for brain metastases from epidermal growth factor receptor (EGFR) mutant non small cell lung cancer (NSCLC). Oncotarget 8:13304–13311. https://doi.org/10.18632/oncotarget.14515
Zhuang Y et al (2018) PD-1 blockade enhances radio-immunotherapy efficacy in murine tumor models. J Cancer Res Clin Oncol 144:1909–1920. https://doi.org/10.1007/s00432-018-2723-4
Zindler JD et al (2017) Whole brain radiotherapy versus stereotactic radiosurgery for 4–10 brain metastases: a phase III randomised multicentre trial. BMC Cancer 17:500. https://doi.org/10.1186/s12885-017-3494-z
Acknowledgements
We thank all the members of Radiation Oncology Department of Thoracic Cancer for kind support.
Funding
This work was supported by the National Natural Science Foundation of Liaoning (2015020263).
Author information
Authors and Affiliations
Contributions
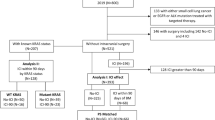
WL and HY designed and wrote the paper; WL collected and read the references, and made the figures and tables.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, W., Yu, H. Separating or combining immune checkpoint inhibitors (ICIs) and radiotherapy in the treatment of NSCLC brain metastases. J Cancer Res Clin Oncol 146, 137–152 (2020). https://doi.org/10.1007/s00432-019-03094-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-03094-9