Abstract
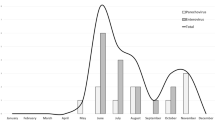
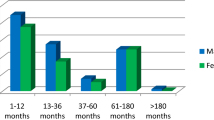
Parechoviruses cause a spectrum of clinical presentations ranging from self-limited to severe encephalitis. In July 2022, state health departments across the USA received an increase in reports of PeV infections among infants. A retrospective cohort study describing the clinical characteristics and outcomes of PeV encephalitis in infants aged < 90 days. Rates of PeV encephalitis were determined based on the number of PeV encephalitis cases out of all meningoencephalitis multiplex polymerase chain reaction panel (MEP) obtained among infants aged < 90 days per year. Out of 2115 infants evaluated for meningoencephalitis, 32 (1.5%) cases of PeV encephalitis were identified. All cases had an absence of pleocytosis and normal protein and glucose levels on CSF analysis. Half of the cases presented with a symptomatic triad (fever, rash, and fussiness). More than one-third of cases (39%) presented with a sepsis-like syndrome, 13% presented with seizures, and 25% were admitted to the pediatric intensive care unit (PICU). MRI of the brain was obtained in four of the cases presented with seizure, all of which demonstrated characteristic radiological findings of the periventricular white matter with frontoparietal predominance and involving the corpus callosum, thalami, and internal and external capsules. Rates of PeV encephalitis varied from year to year, with the highest rates in 2018 and 2022. PeV was the second most detected pathogen in MEP in both 2018 and 2022, and the fifth most detected pathogen in all positive MEP during the study period 2017–2022.
Conclusion: PeV can cause encephalitis and sepsis-like syndrome in infants, and it should be considered even with normal CSF parameters. Prospective studies are needed to better understand PeV epidemiology and to monitor outbreaks.
What is Known: • PeV is a frequent cause of encephalitis and clinical sepsis in infants in the first 90 days. • Normal CSF parameters in PeV encephalitis and diagnostic importance of MEP to avoid unnecessary prolonged antibiotics and hospitalization.. • Centers for Disease Control and Prevention (CDC) issued a Health Advisory alert in Summer 2022 of uptick PeV encephalitis cases in the USA likely secondary of COVID-19 mitigation measures relaxation, but no comparison with previous years.. | |
What is New: • Knowledge of radiological MRI brain characteristics in PeV encephalitis can be a clue diagnosis. • Knowledge of the biennial seasonality pattern in PeV infection. • PeV was the second most detected pathogen in BIOFIRE ME panel in both 2018 and 2022 in our cohort sample. |




Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PeV:
-
Parechovirus encephalitis
- CSF:
-
Cerebrospinal fluid
- PICU:
-
Pediatric intensive care unit
- PCR:
-
Polymerase chain reaction
- CDC:
-
Control and Prevention
- MEP:
-
Meningitis/Encephalitis Panel
- COVID-19:
-
Coronavirus disease 2019
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- ALC:
-
Absolute lymphocyte count
- ANC:
-
Absolute neutrophil count
References
Aizawa Y, Izumita R, Saitoh A (2017) Human parechovirus type 3 infection: an emerging infection in neonates and young infants. J Infect Chemother 23(7):419–426
Black S et al (2019) Comparing the clinical severity of disease caused by enteroviruses and human parechoviruses in neonates and infants. Pediatr Infect Dis J 38(2):e36–e38
Gupta S et al (2010) Extensive white matter abnormalities associated with neonatal parechovirus (PeV) infection. Eur J Paediatr Neurol 14(6):531–534
Harvala H, Wolthers KC, Simmonds P (2010) Parechoviruses in children: understanding a new infection. Curr Opin Infect Dis 23(3):224–230
Renaud C, Harrison CJ (2015) Human parechovirus 3: the most common viral cause of meningoencephalitis in young infants. Infect Dis Clin North Am 29(3):415–428
de Crom SC et al (2016) Enterovirus and parechovirus infection in children: a brief overview. Eur J Pediatr 175(8):1023–1029
Olijve L, Jennings L, Walls T (2018) Human parechovirus: an increasingly recognized cause of sepsis-like illness in young infants. Clin Microbiol Rev 31(1)
Shoji K et al (2013) Dermatologic manifestations of human parechovirus type 3 infection in neonates and infants. Pediatr Infect Dis J 32(3):233–236
Karsch K et al (2015) Human parechovirus infections associated with seizures and rash in infants and toddlers. Pediatr Infect Dis J 34(10):1049–1055
Britton PN et al (2016) Parechovirus encephalitis and neurodevelopmental outcomes. Pediatrics 137(2):e20152848
Verboon-Maciolek MA et al (2008) Human parechovirus causes encephalitis with white matter injury in neonates. Ann Neurol 64(3):266–273
Esposito S et al (2014) Pediatric parechovirus infections. J Clin Virol 60(2):84–89
Tao L et al (2022) Notes from the field: cluster of parechovirus central nervous system infections in young infants - Tennessee, 2022. MMWR Morb Mortal Wkly Rep 71(30):977–978
Thomson J et al (2018) Cerebrospinal fluid reference values for young infants undergoing lumbar puncture. Pediatrics 141(3)
Molloy TJHHKKLMM (2022) The Harriet Lane handbook, 22nd edn
Yum S et al (2021) Trends in viral respiratory infections during COVID-19 pandemic. South Korea Emerg Infect Dis 27(6):1685–1688
Mosscrop LG, Williams TC, Tregoning JS (2022) Respiratory syncytial virus after the SARS-CoV-2 pandemic - what next? Nat Rev Immunol 22(10):589–590
Escuret A et al (2013) Epidemiology of parechovirus infections of the central nervous system in a French pediatric unit. Arch Pediatr 20(5):470–475
Fischer TK et al (2014) Human parechovirus infection. Denmark Emerg Infect Dis 20(1):83–87
Selvarangan R et al (2011) Human parechovirus 3 causing sepsis-like illness in children from midwestern United States. Pediatr Infect Dis J 30(3):238–242
van der Sanden SM, Koopmans MP, van der Avoort HG (2013) Detection of human enteroviruses and parechoviruses as part of the national enterovirus surveillance in the Netherlands, 1996–2011. Eur J Clin Microbiol Infect Dis 32(12):1525–1531
Holmes CW et al (2017) Human parechovirus cluster in the UK, 8 May-2 August 2016-sequence analysis. J Clin Virol 93:37–39
Calvert J et al (2010) Recombination dynamics of human parechoviruses: investigation of type-specific differences in frequency and epidemiological correlates. J Gen Virol 91(Pt 5):1229–1238
Watanabe K, Hirokawa C, Tazawa T (2016) Seropositivity and epidemiology of human parechovirus types 1, 3, and 6 in Japan. Epidemiol Infect 144(16):3451–3460
Seo JH et al (2015) Prevalence of human parechovirus and enterovirus in cerebrospinal fluid samples in children in Jinju. Korea Korean J Pediatr 58(3):102–107
Khatami A et al (2020) Epidemic and inter-epidemic burden of pediatric human parechovirus infection in New South Wales, Australia, 2017–2018. Pediatr Infect Dis J 39(6):507–511
Obermeier PE et al (2016) Acute disseminated encephalomyelitis after human parechovirus infection. Pediatr Infect Dis J 35(1):35–38
van Zwol AL et al (2009) Fatal neonatal parechovirus encephalitis. BMJ Case Rep 2009
Volpe JJ (2008) Neonatal encephalitis and white matter injury: more than just inflammation? Ann Neurol 64(3):232–236
Harvala H et al (2009) Specific association of human parechovirus type 3 with sepsis and fever in young infants, as identified by direct typing of cerebrospinal fluid samples. J Infect Dis 199(12):1753–1760
Felsenstein S et al (2014) Human parechovirus central nervous system infections in southern California children. Pediatr Infect Dis J 33(4):e87-91
Sharp J et al (2013) Characteristics of young infants in whom human parechovirus, enterovirus or neither were detected in cerebrospinal fluid during sepsis evaluations. Pediatr Infect Dis J 32(3):213–216
Nielsen NM et al (2016) Severe human parechovirus infections in infants and the role of older siblings. Am J Epidemiol 183(7):664–670
Tierradentro-Garcia LO et al (2022) Neuroimaging findings in parechovirus encephalitis: a case series of pediatric patients. Pediatr Neurol 130:41–45
Sarma A et al (2019) Human parechovirus meningoencephalitis: neuroimaging in the era of polymerase chain reaction-based testing. AJNR Am J Neuroradiol 40(8):1418–1421
Aldriweesh MA et al (2020) Viruses causing aseptic meningitis: a tertiary medical center experience with a multiplex PCR assay. Front Neurol 11:602267
Author information
Authors and Affiliations
Contributions
Dr. Muayad Alali and Dr. Kiet Tat drafted the initial manuscript and conducted data collection. Dr. Streicher created the figure MRI brain imaging, with caption, and critically reviewed and revised the manuscript. Dr. Hamilton reviewed and revised the manuscript and helped with tables and figures formatting. Dr. Carlucci and Dr. Alali critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree for all content of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of conflicts.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Article Summary
This is a description of an uptick infantile parechovirus encephalitis (PeV) cases in the summer of 2022 and highlighting important clinical characteristics and outcomes of PeV encephalitis.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alali, M., Tat, K., Hamilton, S. et al. Human parechovirus encephalitis in infants: a retrospective single-center study (2017–2022). Eur J Pediatr 182, 4457–4465 (2023). https://doi.org/10.1007/s00431-023-05117-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05117-7