Abstract
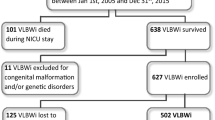
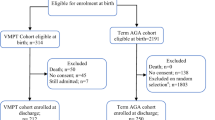
The late preterm infants (34 0/7 to 36 6/7 weeks of gestation) account for at least 70% of all preterm birth. Our aim was to detect growth and neurodevelopment outcome, incidence of neurodevelopmental disability, and its association with maternal and neonatal risk factors among sick late preterm population. Two hundred and ninety-nine late preterm infants were followed up till corrected 2 years of age in this retrospective cohort study. Assessment was done by anthropometry and Developmental Assessment Scale for Indian Infants (DASII) scale at corrected 2 years of age. Presence of visual and hearing impairment, cerebral palsy, and overall neurodevelopmental impairment were also recorded. At 2 years of corrected age, average motor development quotient (DMoQ) was 93.55 (95% CI 90.9 to 96.20) and average mental development quotient (DMeQ) was 89.59 (95% CI 87.13 to 92.04). The incidence of bilateral severe to profound hearing loss and visual loss were found in 6 (2%) and 4 (1.33%) infants, respectively. Severe neurodevelopmental impairment was found in 19 (6.35%) infants. Central nervous system disease and sepsis were found as independent predictors of moderate to severe neurodevelopmental disability.
Conclusion: Late preterm infants admitted in neonatal units were at risk of growth and neurodevelopmental impairment requiring close neurodevelopmental follow-up. In a resource limited setting, this may best be achieved by using DASII in follow-up clinic.
What is Known: • Late preterm infants are at a high risk of prematurity-related morbidities. • There is increased risk of cognitive defect, learning difficulties, and behavior problems found at school age for sick late preterm infants. | |
What is New: • Central nervous system disease and sepsis were found as independent predictors of early moderate to severe neurodevelopmental impairment for sick late preterm infants in developing countries like India. |

Similar content being viewed by others
Data Availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Abbreviations
- ABER:
-
Automated auditory brainstem evoked response
- ANOVA:
-
One-way analysis of variance
- BERA:
-
Brain stem evoked response audiometry
- CI:
-
Confidence interval
- DASII:
-
Developmental Assessment Scale for Indian Infants
- DMoQ:
-
Motor development quotient
- DMeQ:
-
Mental development quotient
- GMFCS:
-
Gross Motor Function Classification System
- LMIC:
-
Low middle income countries
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- OR:
-
Odds ratio
- SCPE:
-
Surveillance of cerebral palsy in Europe
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for the Social Science
References
Hack M, Fanaroff AA (2000) Outcomes of children of extremely low birthweight and gestational age in the 1990s. Semin Neonatol 5:89–106
Liu L, Johnson II, Cousens S et al for the Child Health Epidemiology Reference Group of WHO and UNICEF (2012) Global, regional and national causes of child mortality: an updated systematic review analysis for 2010 with time trends since 2000. Lancet 379(9832):2151–61. https://doi.org/10.1016/S0140-6736(12)60560-1. Epub2012 May 11.
Vohr B (2013) Long term outcomes of moderately preterm, late preterm and early term infants. Clin Perinatol 40:739–751
Engle WA, Tomashek KM, Wallman C, the Committee on Fetus and Newborn (2007) Late-preterm infants: a population at risk. Pediatrics 120:1390–401
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Weiss J, Evans S (2006) Risk factors for neonatal morbidity and mortality among healthy late preterm newborns. Semin Perinatol 30:54–60
Mandruzzato GP, Calì G, Chiaffarino F, Dal Pozzo G, Danti L, Gerosa V et al (2013) Risk factors for late preterm births: a case control study. J Gynecol Obstet 3:182
Escobar GJ, Clark RH, Greene JD (2006) Short-term outcomes of infants born at 35 and 36 weeks gestation: we need to ask more questions. Semin Perinatol 30:28–33
Petrini JR, Dias T, McCormick MC, Massolo ML, Green NS, Escobar GJ (2009) Increased risk of adverse neurological development for late preterm infants. J Pediatr 154:169–176
Kerstjens JM, de Winter AF, Bocca-Tjeertes IF et al (2011) Developmental delay in moderately preterm-born children at school entry. J Pediatr 159:92–98
Boyle EM, Poulsen G, Field DJ et al (2012) Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ 344:e896
Talge NM, Holzman C, Wang J et al (2010) Late-preterm birth and its association with cognitive and socioemotional outcomes at 6 years of age. Pediatrics 126:1124–1131
Lipkind HS, Slopen ME, Pfeiffer MR et al (2012) School-age outcomes of late preterm infants in New York City. Am J Obstet Gynecol 206(222):e1-6
Quigley MA, Poulsen G, Boyle E et al (2012) Early term and late preterm birth are associated with poorer school performance at age 5 years: a cohort study. Arch Dis Child Fetal Neonatal Ed 97:F167–F173
McGowan JE, Alerdice FA, Holmes VA et al (2011) Early childhood development of late-preterm infants: a systematic review. Pediatrics 127:1111–1124
Woythaler MA, McCormick MC, Smith VC (2011) Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics 127:e622–e629
Nepomnyaschy L, Hegyi T, Ostfeld BM et al (2012) Developmental outcomes of late-preterm infants at 2 and 4 years. Matern Child Health J 16:1612–1624
Romeo DM, Di Stefano A, Conversano M et al (2010) Neurodevelopmental outcome at 12 and 18 months in late preterm infants. Eur J Paediatr Neurol 14:503–507
Hughes A, Greisen G, Arce JC et al (2014) Late preterm birth is associated with short-term morbidity but not with adverse neurodevelopmental and physical outcomes at 1 year. Acta Obstet Gynecol Scand 93:109–112
Gupta P, Mital R, Kumar B, Yadav A, Jain M, Upadhyay A (2017) Physical growth, morbidity profile and mortality among healthy late preterm neonates. Indian Pediatr 54:629–634
Lee JS, Polin RA (2003) Treatment and prevention of necrotizing enterocolitis. Semin Neonatol 8:449–459
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729
Definitions of indicators for child anthropometry. Available fromhttp://www.who.int/nutrition/nlis_interpretation_guide.pdf. Accessed 18 Sep 2016
Phatak P (1997) Development assessment scales for Indian infants (DASII). Revised Baroda Norms Manual
Surveillance of Cerebral palsy network in Europe (2000) Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol 42:816–824
Palisano RJ, Rosenbaum PL, Walters SD, Russell D, Wood E, Galuppi B (1997) Development and reliability of a system to clarify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39:214–223
Romeo DM, Guzzardi S, Ricci D, Cilauro S, Brogna C, Cowan F, Romeo MG, Mercuri E (2012) Longitudinal cognitive assessment in healthy late preterm infants. Eur J Paediatr Neurol 16(3):243–7
Johnson S, Evans TA, Draper ES, Field DJ, Manktelow BN, Marlow N, Matthews R, Petrou S, Seaton SE, Smith LK, Boyle EM (2015) Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed 100(4):F301–F308
Ramdin T, Ballot D, Rakotsoane D, Madzudzo L, Brown N, Chirwa T, Cooper P, Davies V (2018) Neurodevelopmental outcome of late preterm infants in Johannesburg, South Africa. BMC Pediatr 18(1):326
Santos IS, Matijasevich A, Domingues MR, Barros AJD, Victora CG, Barros FC (2009) Late preterm birth is a risk factor for growth faltering in early childhood: a cohort study. BMC Pediatr 9:71
Dwivedi D, Singh S, Singh J, Bajaj N, Singh HP (2018) Neurodevelopmental status of children aged 6–30 months with severe acute malnutrition. Indian Pediatr 55(2):131–133
Sujatha R, Jain N (2016) Prediction of neurodevelopmental outcome of preterm babies using risk stratification score. Indian J Pediatr 83(7):640–644
Bhave A, Bhargava R, Kumar R (2011) Correlation between developmental quotients (DASII) and social quotient (Malin’s VSMS) in Indian children aged 6 months to 2 years. J Paediatr Child Health 47(3):87–91
Madaan P, Saini L, Sondhi V (2021) Development assessment scale for Indian infants: a systematic review and perspective on dwindling cutoffs. Indian J Pediatr 88(9):918–920
Saini L, Madaan P, Naik MRR (2019) General movements: longitudinal assessment better than cross-sectional. Brain Dev 41:563–564
Acknowledgements
We would like to thank all patients and doctors who participated in this study for their cooperation. We also would like to express our gratitude to all the staffs of neurodevelopment clinic of our department.
Author information
Authors and Affiliations
Contributions
Suchandra Mukherjee contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Anindya Kumar Saha and Suchandra Mukherjee. The first draft of the manuscript was written by Anindya Kumar Saha. Both the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was obtained from Institutional Ethics Committee (vide IPGME&R/IEC/2018/574 dated 29.09.2018).
Consent to participate
Written informed consent was taken from caregiver/parents.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saha, A.K., Mukherjee, S. Neurodevelopment outcome of late prematurity: a retrospective cohort study from a developing country. Eur J Pediatr 182, 2715–2722 (2023). https://doi.org/10.1007/s00431-023-04953-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04953-x