Abstract
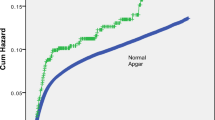
The objective of this study is to investigate whether a significant association exists between low 5-min Apgar scores (< 7) and respiratory morbidity of the offspring. A population-based cohort analysis was performed comparing subtypes of respiratory morbidity leading to hospitalizations among children (up to age 18 years) stratified by their 5 min Apgar scores. Data were collected from two databases of a regional tertiary center. All singleton deliveries occurring between 1991 and 2014 were included in the analysis. A Kaplan-Meier survival curve was constructed to compare cumulative respiratory-related hospitalization incidence and a Cox proportional hazards model to control for confounders. Deliveries (238,622) met the inclusion criteria. Low 5-min Apgar scores were recorded in 742 (0.3%) newborns. Incidence of respiratory hospitalizations was higher among the low 5 min Apgar score group (7.3 vs. 4.8% in the normal [≥ 7] 5 min Apgar score group; OR = 1.5, 95%CI 1.2–2.0, p = 0.003). Association remained significant in the Cox model (aHR = 1.4, 95%CI 1.1–1.9, p = 0.01). Incidence of respiratory-related hospitalizations in preterm born offspring was higher among the low vs. the normal 5 min Apgar score groups (13.4 vs. 7.2%, OR = 2.0, 95%CI 1.2–3.1 , p = 0.008). Association remained significant in the multivariable analysis (aHR = 1.6, 95%CI 1.1–2.5, p = 0.03). The survival curves demonstrated significantly higher cumulative respiratory morbidity in the low Agar score group for the entire cohort and for the preterm born subgroup.
Conclusion: Newborns, of any gestational age, with low 5 min Apgar scores appear to be at an increased risk for pediatric respiratory morbidity.
What is Known: • Apgar score is a method for assessment of the medical condition of a newborn, and of the need for medical intervention and/or resuscitation. Studies assesing the correlation between low Apgar score and short or long term outcomes report a sgnificant correlation with different outcomes including neurological development and more. As two of its five components (color and respiratory effort) are utilizing the respiratory status, low Apgar scoreis associated with a higher risk for immedisate respiratory morbidity. | |
What is New: • Low Apgar score increases the chances for several long-term respiratory-related morbidities, independent of gestational age and other obstetrical circumstances. |



Similar content being viewed by others
References
Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, Souza JP, on behalf of the WHO Multicountry Survey on Maternal and Newborn Health Research Network (2014) Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization multicountry survey on maternal and newborn health. BJOG Int J Obstet Gynaecol 121(s1):14–24
Adams BN, Grunebaum A (2014) Does “pink all over” accurately describe an Apgar color score of 2 in newborns of color? Obstet Gynecol 123:36S
Apgar V (1952) A proposal for a new method of evaluation of the newborn. Classic Pap Crit Care 32(449):97
Beharier O, Sergienko R, Kessous R, Szaingurten-Solodkin I, Walfisch A, Shusterman E, Tsumi E, Sheiner E (2017) Gestational diabetes mellitus is a significant risk factor for long-term ophthalmic morbidity. Arch Gynecol Obstet 295(6):1477–1482
Casey BM, McIntire DD, Leveno KJ (2001) The continuing value of the Apgar score for the assessment of newborn infants. N Engl J Med 344(7):467–471
Cnattingius S, Norman M, Granath F, Petersson G, Stephansson O, Frisell T (2017) Apgar score components at 5 minutes: risks and prediction of neonatal mortality. Paediatr Perinat Epidemiol 31(4):328–337
Dowell A, Darlow B, Macrae J, Stubbe M, Turner N, McBain L (2017) Childhood respiratory illness presentation and service utilisation in primary care: a six-year cohort study in Wellington, New Zealand, using natural language processing (NLP) software. BMJ Open 7(7):e017146
Iliodromiti S, Mackay DF, Smith GCS, Pell JP, Nelson SM (2014) Apgar score and the risk of cause-specific infant mortality: a population-based cohort study. Lancet 384(9956):1749–1755
Islam JY, Keller RL, Aschner JL, Hartert TV, Moore PE (2015) Understanding the short-and long-term respiratory outcomes of prematurity and bronchopulmonary dysplasia. Am J Respir Crit Care Med 192(2):134–156
Jiang ZD, Zang Z, Wilkinson AR (2012) Cochlear function in 1-year-old term infants born with hypoxia-ischaemia or low Apgar scores. J Paediatr Child Health 48(2):160–165
Kasdorf E et al (2014) Improving infant outcome with a 10 min Apgar of 0. Arch Dis Child Fetal Neonatal Ed 100(2):F102–F105
Kvestad E, Lie KK, Eskild A, Engdahl B (2014) Sensorineural hearing loss in children: the association with Apgar score. A registry-based study of 392 371 children in Norway. Int J Pediatr Otorhinolaryngol 78(11):1940–1944
Lagatta J, Yan K, Hoffmann R (2012) The association between 5-min Apgar score and mortality disappears after 24 h at the borderline of viability. Acta Paediatr 101(6):e243–e247
Leybovitz-Haleluya N, Wainstock T, Sheiner E, Segal I, Landau D, Walfisch A (2017) Low Apgar scores in term newborns and long-term gastro-intestinal morbidity: a population-based cohort study with up to 18 years of follow-up. J Matern Fetal Neonatal Med 1–6. https://doi.org/10.1080/14767058.2017.1411475
Manuck TA et al (2016) Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol 215(1):103. e1–103. e14
Orbach H et al (2013) Hypertension and antihypertensive drugs in pregnancy and perinatal outcomes. Am J Obstet Gynecol 208(4):301. e1–301. e6
Persson M et al (2014) Maternal overweight and obesity and risks of severe birth-asphyxia-related complications in term infants: a population-based cohort study in Sweden. PLoS Med 11(5):e1001648
Shah P et al (2015) Outcomes of infants with Apgar score of zero at 10 min: the West Australian experience. Arch Dis Child Fetal Neonatal Ed 100(6):F492–F494
Svenvik M, Brudin L, Blomberg M (2015) Preterm birth: a prominent risk factor for low Apgar scores. BioMed Res Int 2015:978079
Thomas M, Bailit J (2016) Decreasing the prematurity rate: how much could earlier prenatal care help?[10K]. Obstet Gynecol 127:91S
Thorngren-Jerneck K, Herbst A (2001) Low 5-minute Apgar score: a population-based register study of 1 million term births1. Obstet Gynecol 98(1):65–70
Troeger C, Forouzanfar M, Rao PC, Khalil I, Brown A, Swartz S, Fullman N, Mosser J, Thompson RL, Reiner RC Jr, Abajobir A, Alam N, Alemayohu MA, Amare AT, Antonio CA, Asayesh H, Avokpaho E, Barac A, Beshir MA, Boneya DJ, Brauer M, Dandona L, Dandona R, Fitchett JRA, Gebrehiwot TT, Hailu GB, Hotez PJ, Kasaeian A, Khoja T, Kissoon N, Knibbs L, Kumar GA, Rai RK, el Razek HMA, Mohammed MSK, Nielson K, Oren E, Osman A, Patton G, Qorbani M, Roba HS, Sartorius B, Savic M, Shigematsu M, Sykes B, Swaminathan S, Topor-Madry R, Ukwaja K, Werdecker A, Yonemoto N, el Sayed Zaki M, Lim SS, Naghavi M, Vos T, Hay SI, Murray CJL, Mokdad AH (2017) Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the global burden of disease study 2015. Lancet Infect Dis 17(11):1133–1161
Walfisch A, Beharier O, Wainstock T, Sergienko R, Landau D, Sheiner E (2017) Early-term deliveries as an independent risk factor for long-term respiratory morbidity of the offspring. Pediatr Pulmonol 52(2):198–204
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, O'Brien KL, Campbell H, Black RE (2013) Global burden of childhood pneumonia and diarrhoea. Lancet 381(9875):1405–1416
Watterberg KL et al (2015) The Apgar score. Pediatrics 136(4):819–822
Li J et al (2012) The 5-minute Apgar score as a predictor of childhood cancer: a population-based cohort study in five million children. BMJ Open 2(4):e001095
Ellwood P et al (2017) The global asthma network rationale and methods for phase I global surveillance: prevalence, severity, management and risk factors. Eur Respir J 49(1):1601605
Author information
Authors and Affiliations
Contributions
Elisha Ernst has participated in all the phases of this study including planning, literature search, data interpretation and has written the first draft of the manuscript.
Tamar Wainstock PhD is an equal first author contributor. Dr. Wainstock is a specialist in performing all aspects of the statistical analysis needed for this study. She has participated in all phases of this study and has performed most of the analyses presented in this paper and has taken a significant part in the manuscript preparation and drafting.
Eyal Sheiner MD PhD has initiated the study and supervised actively throughout its conduct. Specifically, he was involved in the data interpretation, statistical analysis, and has revised the manuscript.
Daniella Landau MD has participated in all phases of this study including literature search and research planning, data collection, and review and took part in the data interpretation and manuscript preparation.
Asnat Walfisch MD has initiated and participated in all phases of this study including study planning, literature search, data collection and review, and interpretation of the results and has supervised and extensively revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Communicated by Peter de Winter
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Accepted for poster presentation at the SMFM annual meeting, February 2019, Las-Vegas, Nevada.
This study was conducted as part of the requirements for MD degree from the Goldman Medical School at the Faculty of Health Sciences, Ben-Gurion University of the Negev.
Electronic supplementary material
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Ernest, E., Wainstock, T., Sheiner, E. et al. Apgar score and long-term respiratory morbidity of the offspring: a population-based cohort study with up to 18 years of follow-up. Eur J Pediatr 178, 403–411 (2019). https://doi.org/10.1007/s00431-018-03311-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-03311-6