Abstract
Background
The 5-minute APGAR score is clinically used as a screening tool to assess how the newborn has reacted to previous care, remaining relevant for predicting neonatal survival. This study aimed to analyze the determinants of the 5th minute APGAR score, and the factors associated with the death and survival of newborns with low APGAR scores hospitalized in the neonatal intensive care unit (NICU) at a referral public hospital in North Brazil.
Methods
This was a hospital-based retrospective case-control study with 277 medical records. Newborns who presented with a 1-minute APGAR score < 7 followed by a 5-minute APGAR score < 7 were considered cases, while a score ≥ 7 was categorized as controls. Univariate and multivariable logistic regression analyses were used to establish the determinant factors of the low APGAR score and death outcome in this group. Survival curves were obtained using the Kaplan-Meier estimator, and then univariate and multivariate Cox regression was performed.
Results
After adjusted analysis, the factor associated with low APGAR scores was vaginal delivery (OR = 3.25, 95%CI = 1.60–6.62, p = 0.001). Birth injury (OR = 0.39, 95%CI = 0.19–0.83, p = 0.014) was associated with upper APGAR scores. No significant independent associations were observed between the variables analyzed and death in the low APGAR score group. The Kaplan-Meier curve showed that individuals who presented Cesarean delivery had a shorter survival time in the ICU.
Conclusion
In this setting, a 5-minute Apgar score < 7 was associated with the occurrence of vaginal delivery and birth injury with a 5-minute Apgar score ≥ 7. Survival in ICU was lower in newborns that were delivered via cesarean section.
Similar content being viewed by others
Introduction
In Brazil, 303,260 neonatal deaths were recorded from 2007 to 2017, with an average Neonatal Mortality Rate (NMR) of 9.46 per 1000 live births [1]. The country achieved a considerable reduction in the NMR, from 25.33/1000 in 1990 to 8.5/1000 live births in 2019, although it has recently shown a significant deceleration [1, 2]. The improvement of socioeconomic and health policies, such as the implementation of the Unified Health System (SUS) [3]; the “Family Health Strategy” [4], the “Rede Cegonha” strategy, and the “Bolsa Família Program” [5, 6], positively impacted the reduction of mortality rates. Still, the infant and child mortality indicators remain high by international standards, with a concentration of deaths in less developed regions, especially the Northern region of Brazil, which has the highest neonatal mortality rate with 11.02 per 1000 live births [1, 7,8,9,10].
Prematurity is one of the most significant factors contributing to the high rate of neonatal mortality, representing approximately 7.2% of deaths in live births [11, 12], with congenital abnormalities, perinatal asphyxia, birth injury, and lower respiratory tract infections also being frequent causes [13,14,15]. In the northern region, the highest proportion of registered deaths was due to infection (26.9%), followed by prematurity, congenital malformation, and perinatal asphyxia. It should be noted that early NMR associated with perinatal asphyxia in Brazil is still high even in neonates with proper birth weight and without congenital malformations [16, 17].
Prematurity and respiratory problems accounted for the greatest increases in hospitalizations among neonates in the neonatal intensive care unit (NICU), mainly due to inefficient maturity of the respiratory system and greater susceptibility to infection [18,19,20]. In that regard, vaginal delivery accounted for the most vulnerable group to perinatal asphyxia, indicating the importance of avoiding the pilgrimage of women to maternity hospitals, highly skilled personnel trained for resuscitation in the hospital, and greatest intrapartum care (assisted care) [17].
A low Apgar score is an important factor correlated with increased mortality in term and preterm infants without congenital anomalies [21]. It is clinically used to assess hemodynamic impairment such as apnea, bradycardia, cyanosis, hypoperfusion, hypotonia, or respiratory depression. Is used clinically in the first minute as a screening tool to assess the need for early intervention, and in the fifth minute to assess how the newborn reacted to previous care. Still, in the fifth minute, the Apgar score is also relevant for the prediction of neonatal survival [22, 23]. Thus, a cutoff value of 7 points for low and high scores has been discussed by different studies and neurologists [24,25,26,27].
Identifying factors associated with the 5-minute Apgar score and death could be helpful in building strategies to reduce the number of neonatal deaths and morbidity associated with a low Apgar score. Therefore, this study aimed to analyze the determinants of the 5-minute Apgar score and determine the factors associated with death and survival in newborns with low Apgar scores who were hospitalized in the NICU at a referral public hospital in Northern Brazil.
Methods
Study design
This was a hospital-based, unmatched, observational, and retrospective case-control study with descriptive and inferential analyses.
Setting and period of study
The study was conducted using data from medical records of patients treated at a maternal and child health referral hospital in the northern region of Brazil, located in the municipality of Belém (PA), in 2017.
This study took place at a public tertiary-level reference hospital providing maternal-infant care aligned with the Brazilian National Humanization Policy, which aims to implement the SUS principles in daily care and management practices, qualify public health, and encourage solidarity exchanges between managers, workers, and users; the hospital also provided care in line with the Rede Cegonha strategy that encourages humanized care during pregnancy, childbirth, and the puerperium [28]. In addition, the hospital adopts the internal policy of promoting assisted vaginal delivery as it is considered an indicator of the quality of service and referring neonates with a low Apgar score in the 1st minute directly to the NICU where they are monitored, and anthropometrical and postnatal data are recorded according to a specific hospital data instrument.
In the year of the study, 10,460 deliveries were performed, with 5263 normal deliveries (50.4%) and 5197 (49.6%) cesarean sections. A neonatal mortality rate of 12,8% was reported. Regarding physical and professional infrastructure, the hospital had 486 beds, 60 of which were exclusive to the NICU, and a total of 2573 servers, with a total of 122 servers in the delivery room (25 pediatricians, 6 gynecologists/obstetricians, 27 nurses, and 51 nursing technicians). The hospital had a general protocol for cardiopulmonary resuscitation, with 565 service employees trained at the time of the study [29], of with 34 delivery room employees were trained by the Neonatal Resuscitation Programme of the Brazilian Pediatric Society in the year of study (21 pediatricians, and 13 nurses).
Population
The study was conducted with neonates of both sexes admitted to the NICU of the referral hospital.
Eligibility criteria
The medical records of neonates who presented with a 1-minute Apgar score < 7 and were referred to the NICU were included, and so the 5-minute Apgar score was assessed.
Of the deliveries performed in 2017, stillbirths, deaths in the delivery room, and other neonates who were not referred to the neonatal ICU were excluded. Incomplete medical records on Apgar scores, patients with major congenital anomalies (such as anencephaly, severe hydrocephalus, and gastroschisis), and newborns of mothers who received general anesthesia were excluded due to the neonate’s increased chances of receiving a low Apgar score.
Sampling
Probabilistic random sampling was used to select patients.
Sample
The sample size calculation considered 80% power of the study, based on a variable determined randomly by Yeshaneh et al. (2021) [30]. This presented an odds ratio (OR) of 2.3 (1.10–4.71) with a p-value < 0.05, indicating a minimum sample size of 242 participants, with a minimum of 81 individuals in group 1 (Apgar Score < 7) and 161 in group 2 (Apgar Score ≥ 7). This was based on the N2 / N1 allocation ratio (0.502) and proportion p2 or control-to-case ratio (0.155), with an α and β error of 0.05 and 0.2, respectively.
The initial sample consisted of 651 medical records, of which 277 were selected after the eligibility criteria. Newborns with a 5-minute Apgar score < 7 were categorized as cases (G1), and newborns with a 5-minute Apgar score ≥ 7 were categorized as controls (G2) (Fig. 1).
Data collection and variables
Data were collected by reviewing medical records. The Apgar score was estimated using five items, and the final score was calculated from the sum of each item [22]. A form developed by the authors was used for data collection. The following data were included: (1) maternal factors: maternal age, number, gestation, deliveries, and abortions; gestation time (extremely preterm: < 28 weeks, very preterm: 28 to 31 weeks, moderate and late preterm: 32 to 36 weeks, term: 37–41 weeks, post-term: 42 weeks or more) [31, 32]; occurrence and number of prenatal care; gestational complications (leukorrhea, hypertensive disorders of pregnancy [HDP], preeclampsia, anemia, bleeding, and urinary tract infections [UTIs]); (2) obstetric conditions: type of delivery (cesarean or vaginal), single birth, and birth injury, defined as “the structural destruction or functional deterioration of the neonate’s body due to a traumatic event at birth” by Akangire and Carter [33] in 2016; (3) anthropometric data: height, weight, cephalic perimeter, thoracic perimeter, abdominal perimeter, and sex; and (4) clinical postnatal data: ventilatory support (continuous positive airway pressure [CPAP], invasive mechanical ventilation [IMV], and surfactant supplementation) and outcomes (discharge or death).
Primary outcomes
The primary outcome considered the association between maternal characteristics and obstetric conditions as determinants of the 5-minute Apgar score < 7.
Statistical analysis
Descriptive statistical analysis was conducted to compute frequency (absolute and relative), mean, and standard deviation (parametric) or medians with interquartile range (IQR, non-parametric) for each group.
Binary logistic regression analysis was used to establish the determinant factors of the low Apgar score and death outcome in the low Apgar score cohort. Initially, we performed a univariate analysis, considering a p-value < 0.25 [30]. To verify the multicollinearity, the Variance Inflation Factor (VIF) was calculated and the variables that presented a VIF value above 10 were removed from the final model. Statistical significance was set at p < 0.05. OR with 95% confidence intervals (95% CI) were used to quantify the degree of association.
Survival curves were obtained using the Kaplan-Meier estimator, and log-rank (initial), Breslow (intermediary), and Tarone-Ware (final) tests were used to identify the occurrence of a statistically significant difference in the different periods [34].
Results
Factors associated with the 5-minute Apgar score
Seventy-nine individuals were included in G1 and 198 in G2, according to the eligibility criteria (Fig. 1).
Table 1 presents the analysis of the variables (maternal, obstetric and postnatal characteristics) and conditions for both groups.
The overall median number of deliveries was 1, with G1 presenting a lower IQR (p = 0.035) (Table 1). Gestation time showed that neonates with ≤28 weeks of gestation had worse Apgar scores than G2 (G1 = 25.6% vs. G2 = 11.3%) (Table 1). Conversely, neonates with a gestational age between 32 and 36 weeks had better scores concerning the proportion of neonates (p = 0.003) (Table 1).
The other obstetric variables were not significant: mothers’ age (years) (G1: 25 (20, 30), G2: 25 (20, 31); p = 0.700), number of gestations (G1: 2 (1, 3), G2: 2 (1, 3); p = 0.076), number of abortions (G1: 0 (0, 0), G2: 0 (0, 0); p = 0.600), gestation time (continuous) (G1: 34 (26, 37), G2: 33 (30, 35); p > 0.900), prenatal care (G1: 61 (79%), G2: 169 (87%); p = 0.100), number of prenatal care (G1: 2 (1, 4), G2: 3 (2, 4); p = 0.150), UTIs (G1: 28 (35%), G2: 75 (38%); p = 0.700), leukorrhea (G1: 28 (35%), G2: 66 (33%); p = 0.700), anemia (G1: 3 (4.1%), G2: 22 (12%); p = 0.056), bleeding (G1: 7 (9.5%), G2:33 (18%); p = 0.100), preeclampsia (G1: 3 (4.1%), G2: 19 (10%); p = 0.110), HDP (G1: 10 (14%), G2: 29 (16%); p = 0.700).
Cesarean was the overall most frequent type of delivery (58%), although vaginal delivery was the most present in G1 (65%, p < 0.001), birth injury (41%, p = 0.001), IMV (58%, p < 0.001), and death (54%, p < 0.001) were also most common in G1 (Table 1). Surfactant supplementation (53%, p = 0.039) were most common in G1 and CPAP (18%, p = 0.030) in G2 (Table 1). Regarding obstetric conditions, there was no significant difference only for single birth (G1: 68 (86%), G2: 172 (88%); p = 0.700).
Anthropometric characteristics showed no significant differences: weight (g) (G1: 1.612 (899, 2.348), G2: 1.415 (950, 2.075); p = 0.400), height (cm) (G1: 24.0 (11.0, 36.0), G2: 24.0 (14.0, 35.0); p > 0.900), cephalic (cm) (G1: 20.0 (10.0, 27.0), G2: 19.0 (11.0, 25.0); p = 0.700) and thoracic (cm) (G1: 18.0 (10.0, 26.0), G2: 16.0 (11.0, 24.0); p = 0.500), abdominal perimeter (cm) (G1: 19.0 (11.0, 26.0), G2: 17.0 (11.0, 24.0); p = 0.500). In addition, sex (Female G1: 31 (40%), G2: 89 (46%); Male G1: 47 (60%), G2: 104 (54%); p = 0.300) also showed no difference between groups.
Table 2 shows the results of the univariate and multivariate logistic regression analyses. In the univariate analysis, the following variables did not have a p-value to be included in the final model: mothers’ age (years) (OR = 1.00, 95%CI: 0.96–1.03, p = 0.80), number of abortions (OR = 1.11, 95%CI: 0.73–1.63, p = 0.62), gestation time (continuous) (OR = 0.99, 95%CI: 0.93–1.05, p = 0.67), UTIs (OR = 0.90, 95%CI: 0.52–1.54, p = 0.70), leukorrhea (OR = 1.10, 95%CI: 0.63–2.89, p = 0.73), HDP (OR = 0.85, 95%CI: 0.38–1.80, p = 0.68) and single birth (OR = 0.86, 95%CI: 0.41–1.92, p = 0.708). Univariate analysis showed a p < 0.25 for the following variables: number of deliveries, gestation time, prenatal care, number of prenatal care, anemia, bleeding, preeclampsia, vaginal delivery, and birth injury (Table 2). There was no multicollinearity between the variables with p-values < 0.25, therefore, all variables were included. Multivariate analysis showed that vaginal delivery (OR = 3.25, 95%CI = 1.60–6.62, p = 0.001) was associated with a 5-minute Apgar score < 7 and birth injury (OR = 0.39, 95%CI = 0.19–0.83, p = 0.014) was associated with > 7.
Factors associated with mortality and discharge in newborns with a low 5-minute Apgar score
The analysis included 79 newborns with a 5-minute APGAR score < 7, with 42 cases of death, 36 cases of discharge, and 1 case discarded due to missing data (Fig. 1).
Table 3 presents the analysis of each variable category. The overall median number of abortions was 0, with neonates who were discharged presenting a higher IQR (median = 0, IQR = 0–1, p = 0.012) than neonates who died. Gestation time was significantly different between the groups, with death in 37% of neonates with a gestation time between < 28 weeks, and a higher number of discharges between 37 and 41 weeks (p = 0.021).
Birth injury (56%, p = 0.006), surfactant supplementation (64%, p = 0.033), and IMV (69%, p = 0.039) were most frequent in neonates who were discharged. Weight (g) (median = 2.045, 95%CI = 1.436–2.819), height (cm) (median = 45.0, 95%CI = 39.0–48.2), and cephalic (median = 31.8, 95%CI = 28.4–33.6), thoracic (median = 27.0, 95%CI = 24.9–30.0), abdominal (median = 26.5, 95%CI = 23.2–29.8) perimeters and CPAP (17%, p = 0.007) were higher in neonates who died.
The other variables did not show statistically significant differences between the groups. The following maternal characteristics showed no differences: mothers’ age (years) (Death: 26 (20, 31); Discharge: 24 (20, 28); p = 0.300), number of gestations (Death: 1 (1, 4); Discharge: 2 (1, 3); p > 0.900), number of deliveries (Death: 1 (0, 2); Discharge: 1 (0, 1); p = 0.110), number of prenatal care (Death: 3 (1, 5); Discharge: 2 (1, 3); p = 0.100), UTIs (Death: 15 (42%); Discharge: 13 (31%); p = 0.300), leukorrhea (Death: 12 (33%); Discharge: 15 (36%); p = 0.800), Anemia (Death: 1 (3.0%); Discharge: 2 (5.0%); p > 0.900), Bleeding (Death: 1 (3.0%); Discharge: 6 (15%); p = 0.120), Preeclampsia (Death: 3 (9.1%); Discharge: 0 (0%); p = 0.088), HDP (Death: 6 (18%); Discharge: 4 (10%); p = 0.300). The following obstetrical conditions: type of delivery (Cesarean - Death: 11 (26%); Discharge: 17 (47%); Vaginal - Death: 31 (74%); Discharge: 19 (53%); p = 0.054), Single birth (Death: 32 (89%); Discharge: 35 (83%); p = 0.500) showed no differences. Finally, the sex variable (female - Death: 16 (44%), Discharge:14 (34%); Male - Death: 20 (56%); Discharge: 27 (66%); p = 0.400) there was no difference between the outcomes.
Table 4 presents the univariate and multivariable logistic regression analysis. In the univariate analysis, the following variables did not have a p-value to be included in the final model: mothers’ age (years) (OR = 0.97, 95%CI: 0.91–1.03, p = 0.318), number of gestation (OR = 0.96, 95%CI: 0.70–1.31, p = 0.775), prenatal care (OR = 1.35, 95%CI: 0.43–4.29, p = 0.606), UTI (OR = 0.63, 95%CI: 0.24–1.59, p = 0.326), leukorrhea (OR = 1.11, 95%CI: 0.44, 2.87, p = 0.826), anemia (OR = 1.68, 95%CI: 0.15–37.2, p = 0.669), HDP (OR = 0.50, 95%CI: 0.12–1.92, p = 0.312), Single birth (OR = 0.63, 95%CI: 0.15–2.27, p = 0.479), sex (Male) (OR = 1.54, 95%CI: 0.62, 3.92, p = 0.355). Univariate analysis showed a p < 0.25 for the following variables: number of deliveries, number of abortions, gestation time (continuous and in weeks), number of prenatal care, bleeding, preeclampsia, type of delivery (vaginal), birth injury, surfactant supplementation, IMV, CPAP, weight, height, cephalic, thoracic and abdominal perimeters. The final model of the multivariable logistic regression didn’t include the variables weight, gestation time (continuous and in weeks), thoracic and abdominal perimeter, due to multicollinearity (VIF > 10). No significant independent associations were observed in multivariable analysis.
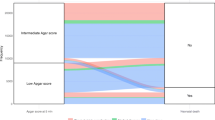
Survival in newborns with a low 5-minute Apgar score
Of the 42 newborns with Apgar < 7 who died, 30 were included in the survival analysis after neonates were excluded because of missing date-of-death data. Figure 2 shows the Kaplan-Meier curve, which indicates that the variable type of cesarean delivery in the middle (p = 0.035) and last (p = 0.041) part of the curve has a shorter survival time in the NICU. There were no significant differences in the other variables (p > 0.05).
Discussion
Among the factors associated with a 5-minute Apgar score < 7, only vaginal delivery had a threefold association. In addition, the presence of birth injury was associated with an Apgar score ≥ 7.
The relationship between vaginal delivery and an Apgar score < 7 may be due to events and complications during childbirth, such as breech presentation and labor duration, which may affect the choice of the delivery method [21, 35, 36].
Birth injury in literature appeared to be associated with the delivery method, birth weight, maternal age, and neonatal cephalic perimeter [35,36,37,38]. Considering that in our study, due to the occurrence of birth injury at higher gestational ages in the neonates with Apgar scores ≥7, it is possible to assume that this group was longer exposed to the possibility of different types of birth injuries, as the most common: scalp injuries, and clavicular fracture [35], which, when not associated with prematurity, did not impact the Apgar score.
It is worth noting that the hospital is a referral hospital for maternal and infant care and has a policy of promoting vaginal delivery, avoiding unnecessary cesarean deliveries, and providing multiprofessional labor management to improve the quality of care.
Prenatal care is essential in minimizing complications during pregnancy and labor since antenatal care improves the prevention, detection, and treatment of risk factors during pregnancy, thereby decreasing the risk of neonatal mortality. Moreover, access to health services, intervention at the right time, and trained professionals in neonatal resuscitation protocols reduce morbidity and mortality in infants [39,40,41].
The Brazilian Ministry of Health recommends that at least six prenatal care consultations be carried out; however, for prenatal care to be effective, they have also recommended that it is important to assess pregnant women early with adequate frequency and consistency [42]. In this study, even though most of the women in both groups had received prenatal care, none had reached the average number of recommended consultations.
These findings are in agreement with the regional pattern as the overall frequency of adequate prenatal care among women in the northern region is one of the lowest, which directly increases the difficulty in providing medical care at the right time affecting mortality. Poor access to prenatal care is one of the factors, along with poverty and low education status, that leads to a higher risk of neonatal death by perinatal asphyxia, one of the main causes of neonatal deaths in the country [16, 17, 43, 44].
The North region is the most extensive in the country, with a population density slightly above four inhabitants per km2 (almost 16 million people) [45], this characteristic promotes difficulties in spatial distribution and transport to specialized health services leading to limitations to access the health system. Regional inequalities regarding access to health services and quality of prenatal care are directly associated with the pilgrimage to a referral service at the right time. Pilgrimage affected more than 20% of women in the northern region [44].
Although national studies have shown that the largest network of obstetric and neonatal care is outsourced by the SUS, it also has described failures of the public system to adequately provide transfer to center-of-excellence hospitals, which are often located in the capitals [46, 47]. This is the scenario of the institution, which receives women from different regions of the state, often in a complex situation, being an “open door” for women with serious pregnancy complications, which contributes to the results, as the pilgrimage was strongly associated with a premature birth initiated by the provider and an Apgar score < 7 in northern Brazil [44].
Considering that 26% of newborns with Apgar < 7 were term and post-term, it is important to assess the quality of perinatal care at the institution. The hospital has a policy of avoid unnecessary cesarean deliveries and provide assisted and multiprofessional labor management to improve the quality of care. Protocols for maternal and infant care are institutionalized in the obstetric emergency department and the neonatal intensive care unit. There are also institutionalized protocols in the delivery room for continuous monitoring during labor according to the risk classification of pregnant women, including use of obstetric Doppler ultrasound. There are also protocols for the use of prenatal steroids in preterm birth, although in the sample of this study, less than 30% of preterm infants received at least one dose of corticosteroids, which demonstrates the importance of monitoring the effective implementation of these protocols in clinical practice.
Regarding infrastructure and staff, the hospital had an annual occupancy rate of 102.6% due to the use of beds improvised and reserved for surgeries. The northern region of Brazil has one of the highest numbers of beds offered by the SUS, with the state of Pará with 2.02 NICU beds (SUS, non-SUS) per 1000 live births [48]. In addition, the hospital had a total of 122 delivery room staff, 27% of whom were trained according to the Neonatal Resuscitation Programme of the Brazilian Pediatric Society, which is still very low considering that the hospital is a reference for high-risk pregnancies. This also reflects a national scenario, where pediatricians were more often in the delivery room, with 94% of them with at least one training course in neonatal resuscitation, and the nursing team not equally trained [49, 50].
In Brazilian state capitals, studies have shown that the main public maternity hospitals have adequate material and human resources in delivery rooms [49]. Nevertheless, in addition to material support, the implementation of adequate monitoring, and training of delivery room staff in resuscitation are crucial to initiate interventions at the right time, as delays can lead to an Apgar score < 7 and neonatal morbidity and mortality even in term neonates [13, 51,52,53].
The Apgar score contributed to the improvement of perinatal care by converting clinical analyses into quantitative data. Knowing the potential determinants of an Apgar score < 7 is important for the prevention and early identification of risks to decrease morbidity and mortality in newborns.
Considering that this was a retrospective observational study, the quality of the data was subject to the availability and accuracy of the information in the hospital’s original database. Orientation was carried out with the data collectors to ensure the correct use of the hospital’s electronic medical record system, with the head nurse responsible for the sector and researchers responsible for the preparation of the collection instrument used in the study. Nevertheless, our analysis may have been influenced by the loss of information. Therefore, the number of missing observations was added to each variable in the tables.
Conclusion
In our center’s patient population, we found that a 5-minute Apgar score < 7 was associated with the occurrence of vaginal delivery, and birth injury with a 5-minute Apgar score > 7. No significant independent associations were observed between the factors studied and death in the low Apgar score cohort. In addition, survival in the NICU was lower in newborns who were delivered via cesarean section.
Limitation of the study
The main limitation is that the results are restricted to the study setting; therefore, caution must be taken with the generalization of these data in other contexts. The lack of access to data regarding fetal presentation, duration of delivery, and instrumental vaginal delivery can be considered a limitation of the analysis. The investigation of the potential interactions of demographic or socioeconomic aspects with the outcomes was beyond the objective of this study but can be considered a limitation since the literature provided callsigns stating a possible relationship between the two. Information on exposure was subject to observation bias.
Availability of data and materials
The data that support the findings of this study are available from the Fundação Santa Casa de Misericordia do Pará - Brazil, which was used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of the hospital.
References
Bernardino FBS, Gonçalves TM, Pereira TID, Xavier JS, Freitas BHBM, Gaíva MAM. Trends in neonatal mortality in Brazil from 2007 to 2017. Tendência da mortalidade neonatal no Brasil de 2007 a 2017. Cien Saude Colet. 2022;27(2):567–78. https://doi.org/10.1590/1413-81232022272.41192020.
World Health Organization (WHO). Neonatal Mortality Rate. 2019. Available in: https://childmortality.org/?r=site/graph&ID=BRA_Brazil,2019»https://childmortality.org/?r=site/graph&ID=BRA_Brazil.. Acessed in 20 Dec 2019.
Brasil. Lei 8080 de 19 de Setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União 1990.
Brazil. Política Nacional de Atenção Básica. Brasília: Ministry of Health; 2017.
Brazil. PORTARIA N° 1.459, DE 24 DE JUNHO DE 2011: Institui, no âmbito do Sistema Único de Saúde - SUS - a Rede Cegonha. Brasília; 2011.
Bugelli A, Borgès Da Silva R, Dowbor L, Sicotte C. The Determinants of Infant Mortality in Brazil, 2010–2020: A Scoping Review. Int J Environ Res Public Health. 2021;18(12):6464. https://doi.org/10.3390/ijerph18126464.
Carvalho CA, da Silva AAM, Victora C, Goldani M, Bettiol H, Thomaz EBAF, et al. Author correction: changes in infant and neonatal mortality and associated factors in eight cohorts from three Brazilian cities. Sci Rep. 2020;10(1):9481. https://doi.org/10.1038/s41598-020-66188-2.
Victora CG, Barros FC. Infant mortality due to perinatal causes in Brazil: trends, regional patterns and possible interventions. Sao Paulo Med J. 2001;119(1):33–42. https://doi.org/10.1590/s1516-31802001000100009.
da Rêgo MGS, Vilela MBR, de Oliveira CM, do Bonfim CV. Óbitos perinatais evitáveis por intervenções do Sistema Único de Saúde do Brasil. Revista Gaúcha de Enfermagem. Rev Gaúcha Enferm. 2018;39. https://doi.org/10.1590/1983-1447.2018.2017-0084.
Bernardino FBS, Gonçalves TM, Pereira TID, Xavier JS, de Freitas BHBM, Gaiva MAM. Tendência da mortalidade neonatal no Brasil de 2007 a 2017. Ciência Saúde Colet. 2022;27(2):567–78. https://doi.org/10.1590/1413-81232022272.41192020.
Veloso FCS, Kassar LML, Oliveira MJC, Lima THB, Bueno NB, Gurgel RQ, et al. Analysis of neonatal mortality risk factors in Brazil: a systematic review and meta-analysis of observational studies. J Pediatr. 2019;95(5):519–30. https://doi.org/10.1016/j.jped.2018.12.014.
de Souza S, Duim E, Nampo FK. Determinants of neonatal mortality in the largest international border of Brazil: a case-control study. BMC Public Health. 2019;19(1):1304. https://doi.org/10.1186/s12889-019-7638-8.
Guinsburg R, Sanudo A, Kiffer CRV, Marinonio ASS, Costa-Nobre DT, Areco KN, et al. Annual trend of neonatal mortality and its underlying causes: population-based study - São Paulo state, Brazil, 2004-2013. BMC Pediatr. 2021;21(1):54. https://doi.org/10.1186/s12887-021-02511-8.
Bezerra IMP, Ramos JLS, Pianissola MC, Adami F, Rocha JBF, Ribeiro MA, et al. Perinatal mortality analysis in Espírito Santo, Brazil, 2008 to 2017. Int J Environ Res Public Health. 2021;18(21):11671. https://doi.org/10.3390/ijerph182111671.
França EB, Lansky S, Rego MAS, Malta DC, França JS, Teixeira R, et al. Leading causes of child mortality in Brazil, in 1990 and 2015: estimates from the global burden of disease study. Principais causas da mortalidade na infância no Brasil, em 1990 e 2015: estimativas do estudo de Carga global de Doença. Rev Bras Epidemiol. 2017;20(Suppl 01):46–60. https://doi.org/10.1590/1980-5497201700050005.
Almeida MF, Kawakami MD, Moreira LM, Santos RM, Anchieta LM, Guinsburg R. Early neonatal deaths associated with perinatal asphyxia in infants ≥2500g in Brazil. J Pediatr (Rio J). 2017;93:576–84. https://doi.org/10.1016/j.jped.2016.11.008.
Kawakami MD, Sanudo A, Teixeira MLP, Andreoni S, Castro JQX, Waldvogel B, et al. Neonatal mortality associated with perinatal asphyxia: a population-based study in a middle-income country. BMC Pregnancy Childbirth. 2021;21(1):169. https://doi.org/10.1186/s12884-021-03652-5.
Faria TF, Kamada I. Lesiones de la piel en neonatos en cuidados intensivos neonatales. Enferm Glob. 2018;17(49):211–36. https://doi.org/10.6018/eglobal.17.1.273671.
Angelica D, Roberta W, Crislaine P. Profile of neonates hospitalized at a neonatal intensive care unit: a cross-sectional study. Arq Ciênc Saúde. 2016;23(2):100–5. https://doi.org/10.17696/2318-3691.23.2.2016.308.
Ministério da Saúde. Atenção à saúde do recém-nascido: guia para os profissionais de saúde [monografia na Internet]. 2nd ed. Brasília; 2012. Available in: http://bvsms.saude.gov.br/bvs/publicacoes/atencao_saude_recem_nascido_profissionais_v1.p. Acessed in 06 Apr 2022
Gudayu TW. Proportion and factors associated with low fifth minute Apgar score among singleton newborn babies in Gondar University referral hospital, North West Ethiopia. Afr Health Sci. 2017;17(1):1–6. https://doi.org/10.4314/ahs.v17i1.2.
Simon LV, Hashmi MF, Bragg BN. APGAR Score. In: StatPearls; 2022. Available in: https://www.ncbi.nlm.nih.gov/books/NBK470569/.
Casey BM, McIntire DD, Leveno KJ. The continuing value of the Apgar score for the assessment of newborn infants. N Engl J Med. 2001;344(7):467–71.
Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. N Engl J Med. 2020;383(1):49–57. https://doi.org/10.1056/NEJMoa1915075.
Razaz N, Cnattingius S, Joseph KS. Association between Apgar scores of 7 to 9 and neonatal mortality and morbidity: population-based-low-risk study of term infants in Sweden. BMJ. 2019;365:l1656. https://doi.org/10.1136/bmj.l1656.
Silva LV, Araújo LB, Azevedo VMGO. Assessment of the neuropsychomotor development in the first year of life of premature infants with and without bronchopulmonary dysplasia. Rev Bras Ter Intens. 2018;30(2):174–80. https://doi.org/10.5935/0103-507X.20180023.
Apgar V. A proposal for a new method of evaluation of the newborn infant. Originally published in July 1953, volume 32, pages 250–259. Anesth Analg. 2015;120(5):1056–9. https://doi.org/10.1213/ANE.0b013e31829bdc5c.
Brasil. Ministério da Saúde Gabinete do Ministro. PORTARIA N° 1.459, DE 24 DE JUNHO DE 2011.
Fundação Santa Casa de Misericórdia do Pará. Relatório de Gestão. 2017. Available in: https://santacasa.pa.gov.br/wp-content/uploads/2020/09/RELAT%C3%93RIO-2017-JURISDICIONADO.pdf Acessed in 04 June 2022.
Yeshaneh A, Kassa A, Kassa Z, Adane D, Fikadu Y, Wassei SH, et al. The determinants of 5th minute low Apgar score among newborns who delivered at public hospitals in Hawassa City, South Ethiopia. BMC Pediatr. 2021;21:266. https://doi.org/10.1186/s12887-021-02745-6.
Neligan GA, Ballabriga A, Beutnagel H, Bucci G, Dunn PM, Ewerbeck H, et al. Working party to discuss nomenclature based on gestational age and birthweight. Arch Dis Child. 1970;45:730.
Quinn JA, Munoz FM, Gonik B, Frau L, Cutland C, Mallett-Moore T, et al. Preterm birth: case definition & guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine. 2016;34(49):6047–56. https://doi.org/10.1016/j.vaccine.2016.03.045.
Akangire G, Carter B. Birth injuries in neonates. Pediatr Rev. 2016;37(11):451–62. https://doi.org/10.1542/pir.2015-0125.
Tonin FS, Araujo AG, Fachi MM, Ferreira VL, Pontarolo R, Fernandez-Llimos F. Lag times in the publication of network meta-analyses: a survey. BMJ Open. 2021;11:e048581. https://doi.org/10.1136/bmjopen-2020-048581.
Linder N, Linder I, Fridman E, Kouadio F, Lubin D, Merlob P, et al. Birth trauma – risk factors and short-term neonatal outcome. J Matern Fetal Neonatal Med. 2013;26(15):1491–5. https://doi.org/10.3109/14767058.2013.789850.
Duarte G, da Cunha SP, Shimazaki WS, Marcolino AC, Nogueira AA, Berezowski AT, et al. Tocotraumatismo com repercussäo neonatal. Rev Bras Ginecol Obstet. 1997;19(1):7–11.
Wang H, Luo B, Tong XM. A single-center study of the incidence of neonatal birth trauma and its risk factors. Zhongguo Dang Dai Er Ke Za Zhi. 2019;21(3):249–52. https://doi.org/10.7499/j.issn.1008-8830.2019.03.012.
Wen Q, Muraca GM, Ting J, Coad S, Lim KI, Lisonkova S. Temporal trends in severe maternal and neonatal trauma during childbirth: a population-based observational study. BMJ Open. 2018;8(3):e020578. https://doi.org/10.1136/bmjopen-2017-020578.
Salustiano EM, Campos JA, Ibidi SM, Ruano R, Zugaib M. Low Apgar scores at 5 minutes in a low risk population: maternal and obstetrical factors and postnatal outcome. Rev Assoc Med Bras (1992). 2012;58(5):587–93. https://doi.org/10.1590/S0104-42302012000500017.
Wondemagegn AT, Alebel A, Tesema C, Abie W. The effect of antenatal care follow-up on neonatal health outcomes: a systematic review and meta-analysis. Public Health Rev. 2018;39:33. https://doi.org/10.1186/s40985-018-0110-y.
Patel D, Piotrowski ZH, Nelson MR, Sabich R. Effect of a statewide neonatal resuscitation training program on Apgar scores among high-risk neonates in Illinois. Pediatrics. 2001;107(4):648–55. https://doi.org/10.1542/peds.107.4.648 PMID: 11335738.
Brazil, Ministério da Saúde (BR), Secretaria de Atenção à Saúde, Departamento de Atenção Básica. Atenção ao pré-natal de baixo risco. Brasília; 2012. (Série A. Normas e Manuais Técnicos) (Cadernos de Atenção Básica, 32)
Mario DB, Rigo L, Boclin KLS, Malvestio LMM, Anziliero D, Horta BL, et al. Qualidade do Pré-Natal no Brasil: Pesquisa Nacional de Saúde 2013. Ciência Saúde Coletiva. 2019;24(3):1223–32. https://doi.org/10.1590/1413-81232018243.13122017.
Leal MDC, Esteves-Pereira AP, Viellas EF, Domingues RMSM, Gama SGND. Prenatal care in the Brazilian public health services. Rev Saude Publica. 2020;54:08. https://doi.org/10.11606/s1518-8787.2020054001458.
IBGE, Censo Demográfico 1872, 1890, 1900, 1920, 1940, 1950, 1960, 1970, 1980, 1991, 2000 e 2010. https://censo2010.ibge.gov.br/sinopse/index.php?dados=10&uf=00
Bittencourt SDA, Reis LGC, Ramos MM, Rattner D, Rodrigues PL, Neves DCO, et al. Estrutura das maternidades: aspectos relevantes para a qualidade da atenção ao parto e nascimento. Cadernos Saúde Pública. 2014;30(1):S208–19. https://doi.org/10.1590/0102-311X00176913.
Bittencourt SD, Domingues RM, Reis LG, Ramos MM, Leal MD. Adequacy of public maternal care services in Brazil. Reprod Health. 2016;13(3):120. https://doi.org/10.1186/s12978-016-0229-6.
Almeida MC, Gomes CM, Nascimento LF. Spatial distribution of number of Neonatal Intensive Care Units beds in Brazil and its association with child mortality rate. Saúde Pesquisa. 2021;14(4):e8442. https://doi.org/10.17765/2176-9206.
Almeida MFB, et al. Material and human resources for neonatal resuscitation in public maternity hospitals in Brazilian state capitals. Sao Paulo Med J. 2008;126(3):156–60. https://doi.org/10.1590/S1516-31802008000300004.
Moshiro R, Ersdal HL, Mdoe P, Kidanto HL, Mbekenga C. Factors affecting effective ventilation during newborn resuscitation: a qualitative study among midwives in rural Tanzania. Glob Health Action. 2018;11(1):1423862. https://doi.org/10.1080/16549716.2018.1423862.
Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. 2017;1(1):e000183. https://doi.org/10.1136/bmjpo-2017-000183.
Bajaj M, Natarajan G, Shankaran S, et al. Reanimação na Sala de Parto e Resultados a Curto Prazo em Recém-nascidos Moderadamente Prematuros. J Pediatr. 2018;195:33–8.e2. https://doi.org/10.1016/j.jpeds.2017.11.039.
Maier B, Georgoulopoulos A, Zajc M, Jaeger T, Zuchna C, Hasenoehrl G. Fetal outcome for infants in breech by method of delivery: experiences with a stand-by service system of senior obstetricians and women's choices of mode of delivery. J Perinat Med. 2011;39(4):385–90. https://doi.org/10.1515/jpm.2011.044.
Acknowledgments
We thank the Tertiary Reference Hospital in maternal and child health Fundação Santa Casa de Misericordia do Pará - Brazil and the Laboratory of Clinical and Experimental Research of the Urogenital System (UPCEURG - UFPA).
Funding
None declared.
Author information
Authors and Affiliations
Contributions
ESR, LFGR, LFCM, GCSC, SSA: data collection, investigation. VBT, JSS, MVGA: investigation, writing, review, and editing. PFMN, FCG: review support. JSMN: project administration, supervision, review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations under Resolution 466/12 of the National Health Council of Brazil. The Research Ethics Committee of the Santa Casa de Misericórdia do Pará Foundation (n. 2,442,015), approved this research and considered the need for informed written consent to participate unnecessarily due to the use of secondary data and according to the aforementioned resolution.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tavares, V.B., e Souza, J.d., Affonso, M. et al. Factors associated with 5-min APGAR score, death and survival in neonatal intensive care: a case-control study. BMC Pediatr 22, 560 (2022). https://doi.org/10.1186/s12887-022-03592-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03592-9