Abstract
Digestive neuroendocrine neoplasms (NENs) are a group of heterogeneous neoplasms found throughout the digestive tract, with different behaviour and genetic background. In the last few years, nomenclature and WHO/UICC classifications of digestive NENs have changed, and molecular classifications have emerged, especially in pancreatic locations. Increasing patho-molecular details are needed to diagnose the different categories of NEN, including the use of helpful immunohistochemical markers. In this review, we address these topics in three successive chapters. We first briefly review recent updates in classifications, discuss important grading and proliferating issues and advances in the molecular understanding of NEN. Then, we provide an update on diagnosis, including the most important differential diagnoses of NEN, with a focus on high-grade neoplasms and mixed tumours. Finally, we highlight a variety of currently used and next-generation predictive and prognostic biomarkers as well as biomarkers of tumour origin and describe some site specificities of gastrointestinal NEN. We specifically focus on biomarkers available to pathologists with the potential to change the way patients with NEN are diagnosed and treated.

















Similar content being viewed by others
References
Lokuhetty D, White V, Watanabe R, Cree I (2019) WHO classification of tumours – digestive system tumours, 5th edn. IARC Press, Lyon
Lloyd RV, Osamura RY, Klöppel G, Rosai J (2017) WHO classification of tumours of endocrine organs, 4th edn. IARC Press, Lyon
Botling J, Lamarca A, Bajic D et al (2020) High-grade progression confers poor survival in pancreatic neuroendocrine tumors. Neuroendocrinology 110:891–898. https://doi.org/10.1159/000504392
Panzuto F, Cicchese N, Partelli S et al (2017) Impact of Ki67 re-assessment at time of disease progression in patients with pancreatic neuroendocrine neoplasms. PLoS ONE 12:e0179445. https://doi.org/10.1371/journal.pone.0179445
Zhang X-F, Xue F, Wu Z et al (2020) Development and validation of a modified eighth AJCC staging system for primary pancreatic neuroendocrine tumors. Ann Surg. https://doi.org/10.1097/SLA.0000000000004039
Amin MB, Greene FL, Edge SB et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67:93–99. https://doi.org/10.3322/caac.21388
Brierley J, Gospodarowicz M, Wittekind C (2017) TNM classification of malignant tumours, 8th edn. Wiley Blackwell, Oxford
Dhall D, Mertens R, Bresee C et al (2012) Ki-67 proliferative index predicts progression-free survival of patients with well-differentiated ileal neuroendocrine tumors. Hum Pathol 43:489–495. https://doi.org/10.1016/j.humpath.2011.06.011
Grillo F, Albertelli M, Brisigotti MP et al (2015) Grade increases in gastro-entero-pancreatic neuroendocrine tumor metastases compared to the primary tumor. Neuroendocrinology. https://doi.org/10.1159/000439434
Khan MS, Luong TV, Watkins J et al (2013) A comparison of Ki-67 and mitotic count as prognostic markers for metastatic pancreatic and midgut neuroendocrine neoplasms. Br J Cancer 108:1838–1845. https://doi.org/10.1038/bjc.2013.156
Perren A, Couvelard A, Scoazec J-Y et al (2017) ENETS consensus guidelines for the standards of care in neuroendocrine tumors: pathology: diagnosis and prognostic stratification. Neuroendocrinology 105:196–200. https://doi.org/10.1159/000457956
Owens R, Gilmore E, Bingham V et al (2020) Comparison of different anti-Ki67 antibody clones and hot-spot sizes for assessing proliferative index and grading in pancreatic neuroendocrine tumours using manual and image analysis. Histopathology 77:646–658. https://doi.org/10.1111/his.14200
Tellez-Gabriel M, Ory B, Lamoureux F et al (2016) Tumour heterogeneity: the key advantages of single-cell analysis. Int J Mol Sci 17:E2142. https://doi.org/10.3390/ijms17122142
Shi C, Gonzalez RS, Zhao Z et al (2015) Liver metastases of small intestine neuroendocrine tumors: Ki-67 heterogeneity and World Health Organization grade discordance with primary tumors. Am J Clin Pathol 143:398–404. https://doi.org/10.1309/AJCPQ55SKOCYFZHN
Yang Z, Tang LH, Klimstra DS (2011) Effect of tumor heterogeneity on the assessment of Ki67 labeling index in well-differentiated neuroendocrine tumors metastatic to the liver: implications for prognostic stratification. Am J Surg Pathol 35:853–860. https://doi.org/10.1097/PAS.0b013e31821a0696
Kankava K, Maisonneuve P, Mangogna A et al (2021) Prognostic features of gastro-entero-pancreatic neuroendocrine neoplasms in primary and metastatic sites: grade, mesenteric tumour deposits and emerging novelties. J Neuroendocrinol 33(8):e13000. https://doi.org/10.1111/jne.13000
de Mestier L, Armani M, Cros J et al (2019) Lesion-by-lesion correlation between uptake at FDG PET and the Ki67 proliferation index in resected pancreatic neuroendocrine tumors. Dig Liver Dis 51:1720–1724. https://doi.org/10.1016/j.dld.2019.06.022
Vyas M, Tang LH, Rekhtman N, Klimstra DS (2021) Alterations in Ki67 labeling following treatment of poorly differentiated neuroendocrine carcinomas: a potential diagnostic pitfall. Am J Surg Pathol 45:25–34. https://doi.org/10.1097/PAS.0000000000001602
Govind D, Jen K-Y, Matsukuma K et al (2020) Improving the accuracy of gastrointestinal neuroendocrine tumor grading with deep learning. Sci Rep 10:11064. https://doi.org/10.1038/s41598-020-67880-z
Satturwar SP, Pantanowitz JL, Manko CD et al (2020) Ki-67 proliferation index in neuroendocrine tumors: can augmented reality microscopy with image analysis improve scoring? Cancer Cytopathol 128:535–544. https://doi.org/10.1002/cncy.22272
Di Domenico A, Wiedmer T, Marinoni I, Perren A (2017) Genetic and epigenetic drivers of neuroendocrine tumours (NET). Endocr Relat Cancer 24:R315–R334. https://doi.org/10.1530/ERC-17-0012
Jiao Y, Shi C, Edil BH et al (2011) DAXX/ATRX, MEN1 and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science 331:1199–1203. https://doi.org/10.1126/science.1200609
Scarpa A, Chang DK, Nones K et al (2017) Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 543:65–71. https://doi.org/10.1038/nature21063
Di Domenico A, Pipinikas CP, Maire RS et al (2020) Epigenetic landscape of pancreatic neuroendocrine tumours reveals distinct cells of origin and means of tumour progression. Commun Biol 3:740. https://doi.org/10.1038/s42003-020-01479-y
Lakis V, Lawlor RT, Newell F et al (2021) DNA methylation patterns identify subgroups of pancreatic neuroendocrine tumors with clinical association. Commun Biol 4:155. https://doi.org/10.1038/s42003-020-01469-0
Pipinikas CP, Berner AM, Sposito T, Thirlwell C (2019) The evolving (epi)genetic landscape of pancreatic neuroendocrine tumours. Endocr Relat Cancer 26:R519–R544. https://doi.org/10.1530/ERC-19-0175
Hackeng WM, Brosens LAA, Kim JY et al (2021) Non-functional pancreatic neuroendocrine tumours: ATRX/DAXX and alternative lengthening of telomeres (ALT) are prognostically independent from ARX/PDX1 expression and tumour size. Gut. https://doi.org/10.1136/gutjnl-2020-322595 (gutjnl-2020-322595)
Elvebakken H, Perren A, Scoazec J-Y et al (2020) A consensus developed morphological re-evaluation of 196 high-grade gastroenteropancreatic neuroendocrine neoplasms and its clinical correlations. Neuroendocrinology. https://doi.org/10.1159/000511905
Røge R, Kristoffersen HL, Bzorek M et al (2019) NordiQC assessments of chromogranin A immunoassays. Appl Immunohistochem Mol Morphol 27:258–262. https://doi.org/10.1097/PAI.0000000000000743
Bellizzi AM (2020) Immunohistochemistry in the diagnosis and classification of neuroendocrine neoplasms: what can brown do for you? Hum Pathol 96:8–33. https://doi.org/10.1016/j.humpath.2019.12.002
Kim D, Viswanathan K, Goyal A, Rao R (2020) Insulinoma-associated protein 1 (INSM1) is a robust marker for identifying and grading pancreatic neuroendocrine tumors. Cancer Cytopathol 128:269–277. https://doi.org/10.1002/cncy.22242
McHugh KE, Mukhopadhyay S, Doxtader EE et al (2020) INSM1 Is a highly specific marker of neuroendocrine differentiation in primary neoplasms of the gastrointestinal tract, Appendix, and Pancreas. Am J Clin Pathol 153:811–820. https://doi.org/10.1093/ajcp/aqaa014
Mukhopadhyay S, Dermawan JK, Lanigan CP, Farver CF (2019) Insulinoma-associated protein 1 (INSM1) is a sensitive and highly specific marker of neuroendocrine differentiation in primary lung neoplasms: an immunohistochemical study of 345 cases, including 292 whole-tissue sections. Mod Pathol 32:100–109. https://doi.org/10.1038/s41379-018-0122-7
Rooper LM, Sharma R, Li QK et al (2017) INSM1 demonstrates superior performance to the individual and combined use of synaptophysin, chromogranin and CD56 for diagnosing neuroendocrine tumors of the thoracic cavity. Am J Surg Pathol 41:1561–1569. https://doi.org/10.1097/PAS.0000000000000916
Sakakibara R, Kobayashi M, Takahashi N et al (2020) Insulinoma-associated protein 1 (INSM1) is a better marker for the diagnosis and prognosis estimation of small cell lung carcinoma than neuroendocrine phenotype markers such as chromogranin A, synaptophysin, and CD56. Am J Surg Pathol 44:757–764. https://doi.org/10.1097/PAS.0000000000001444
Staaf J, Tran L, Söderlund L et al (2020) Diagnostic value of insulinoma-associated protein 1 (INSM1) and comparison with established neuroendocrine markers in pulmonary cancers. Arch Pathol Lab Med 144:1075–1085. https://doi.org/10.5858/arpa.2019-0250-OA
Zhang Q, Huang J, He Y et al (2021) Insulinoma-associated protein 1(INSM1) is a superior marker for the diagnosis of gastroenteropancreatic neuroendoerine neoplasms: a meta-analysis. Endocrine. https://doi.org/10.1007/s12020-021-02754-6
Bellizzi AM (2020) Pathologic considerations in gastroenteropancreatic neuroendocrine tumors. Surg Oncol Clin N Am 29:185–208. https://doi.org/10.1016/j.soc.2019.11.003
Couvelard A, Cros J, Kasajima A et al (2021) Digestive and lung high-grade neuroendocrine neoplasms: update and challenging issues. Curr Opin Endocr Metab Res 18:224–229. https://doi.org/10.1016/j.coemr.2021.04.002
Digiacomo N, Bolzacchini E, Veronesi G et al (2019) Neuroendocrine differentiation, microsatellite instability, and tumor-infiltrating lymphocytes in advanced colorectal cancer with BRAF mutation. Clin Colorectal Cancer 18:e251–e260. https://doi.org/10.1016/j.clcc.2018.12.003
Fassan M, Milione M, Maddalena G et al (2021) Synaptophysin expression in V600EBRAF-mutated advanced colorectal cancers identifies a new subgroup of tumours with worse prognosis. Eur J Cancer 146:145–154. https://doi.org/10.1016/j.ejca.2021.01.016
La Rosa S, Franzi F, Marchet S et al (2009) The monoclonal anti-BCL10 antibody (clone 331.1) is a sensitive and specific marker of pancreatic acinar cell carcinoma and pancreatic metaplasia. Virchows Arch 454:133–142. https://doi.org/10.1007/s00428-008-0710-x
La Rosa S, Adsay V, Albarello L et al (2012) Clinicopathologic study of 62 acinar cell carcinomas of the pancreas: insights into the morphology and immunophenotype and search for prognostic markers. Am J Surg Pathol. https://doi.org/10.1097/PAS.0b013e318263209d
Uhlig R, Contreras H, Weidemann S et al (2022) Carboxypeptidase A1 (CPA1) immunohistochemistry is highly sensitive and specific for acinar cell carcinoma (acc) of the pancreas. Am J Surg Pathol 46:97–104. https://doi.org/10.1097/PAS.0000000000001817
Kanehira K, Khoury T (2011) Neuroendocrine markers expression in pancreatic serous cystadenoma. Appl Immunohistochem Mol Morphol 19:141–146. https://doi.org/10.1097/PAI.0b013e3181f5023d
Mamilla D, Manukyan I, Fetsch PA et al (2020) Immunohistochemical distinction of paragangliomas from epithelial neuroendocrine tumors-gangliocytic duodenal and cauda equina paragangliomas align with epithelial neuroendocrine tumors. Hum Pathol 103:72–82. https://doi.org/10.1016/j.humpath.2020.07.010
Basturk O, Yang Z, Tang LH et al (2015) The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol 39:683–690. https://doi.org/10.1097/PAS.0000000000000408
Fazio N, Milione M (2016) Heterogeneity of grade 3 gastroenteropancreatic neuroendocrine carcinomas: new insights and treatment implications. Cancer Treat Rev 50:61–67. https://doi.org/10.1016/j.ctrv.2016.08.006
Heetfeld M, Chougnet CN, Olsen IH et al (2015) Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer 22:657–664. https://doi.org/10.1530/ERC-15-0119
Pellat A, Cottereau AS, Palmieri L-J et al (2021) Digestive well-differentiated grade 3 neuroendocrine tumors: current management and future directions. Cancers (Basel) 13:2448. https://doi.org/10.3390/cancers13102448
Pellat A, Coriat R (2020) Well differentiated grade 3 neuroendocrine tumors of the digestive tract: a narrative review. J Clin Med 9(6):1677. https://doi.org/10.3390/jcm9061677
Sorbye H, Kong G, Grozinsky-Glasberg S (2020) PRRT in high-grade gastroenteropancreatic neuroendocrine neoplasms (WHO G3). Endocr Relat Cancer 27:R67–R77. https://doi.org/10.1530/ERC-19-0400
Busico A, Maisonneuve P, Prinzi N et al (2020) Gastroenteropancreatic high-grade neuroendocrine neoplasms: histology and molecular analysis, two sides of the same coin. Neuroendocrinology 110:616–629. https://doi.org/10.1159/000503722
Shi H, Chen L, Zhang Q et al (2020) Concordance between the Ki-67 index cutoff value of 55% and differentiation in neuroendocrine tumor and neuroendocrine carcinoma in grade 3 pancreatic neuroendocrine neoplasms. Pancreas 49:1378–1382. https://doi.org/10.1097/MPA.0000000000001693
Sorbye H, Welin S, Langer SW et al (2013) Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol 24:152–160. https://doi.org/10.1093/annonc/mds276
Ali AS, Grönberg M, Federspiel B et al (2017) Expression of p53 protein in high-grade gastroenteropancreatic neuroendocrine carcinoma. PLoS ONE 12:e0187667. https://doi.org/10.1371/journal.pone.0187667
Hadoux J, Kanaan C, Durand A et al (2021) Prognostic factors of metastatic neuroendocrine carcinoma under first-line treatment with platinum etoposide with a focus on NEC score and Rb expression: results from the multicentre RBNEC study of the Groupe d’Etude des Tumeurs Endocrines (GTE) and the ENDOCAN-RENATEN network. Eur J Cancer 152:100–115. https://doi.org/10.1016/j.ejca.2021.04.030
Konukiewitz B, Schlitter AM, Jesinghaus M et al (2017) Somatostatin receptor expression related to TP53 and RB1 alterations in pancreatic and extrapancreatic neuroendocrine neoplasms with a Ki67-index above 20. Mod Pathol 30:587–598. https://doi.org/10.1038/modpathol.2016.217
Yachida S, Vakiani E, White CM et al (2012) Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol 36:173–184. https://doi.org/10.1097/PAS.0b013e3182417d36
Cros J, Théou-Anton N, Gounant V et al (2021) Specific genomic alterations in high-grade pulmonary neuroendocrine tumours with carcinoid morphology. Neuroendocrinology 111:158–169. https://doi.org/10.1159/000506292
Yeo M-K, Yoon N, Bae GE (2021) Clinicopathologic and molecular characteristics of gastrointestinal MiNENs. Front Oncol 11:709097. https://doi.org/10.3389/fonc.2021.709097
Luong TV, Nisa Z, Watkins J, Hayes AR (2020) Should immunohistochemical expression of mismatch repair (MMR) proteins and microsatellite instability (MSI) analysis be routinely performed for poorly differentiated colorectal neuroendocrine carcinomas? Endocrinol Diabetes Metab Case Rep 2020:EDM200058. https://doi.org/10.1530/EDM-20-0058
Sahnane N, Furlan D, Monti M et al (2015) Microsatellite unstable gastrointestinal neuroendocrine carcinomas: a new clinicopathologic entity. Endocr Relat Cancer 22:35–45. https://doi.org/10.1530/ERC-14-0410
Merola E, Zandee W, de Mestier L et al (2021) Histopathological revision for gastroenteropancreatic neuroendocrine neoplasms in expert centers: does it make the difference? Neuroendocrinology 111:170–177. https://doi.org/10.1159/000507082
Lemelin A, Barritault M, Hervieu V et al (2019) O6-methylguanine-DNA methyltransferase (MGMT) status in neuroendocrine tumors: a randomized phase II study (MGMT-NET). Dig Liver Dis 51:595–599. https://doi.org/10.1016/j.dld.2019.02.001
Frizziero M, Chakrabarty B, Nagy B et al (2020) Mixed neuroendocrine non-neuroendocrine neoplasms: a systematic review of a controversial and underestimated diagnosis. J Clin Med 9:E273. https://doi.org/10.3390/jcm9010273
Uccella S, La Rosa S (2020) Looking into digestive mixed neuroendocrine - nonneuroendocrine neoplasms: subtypes, prognosis, and predictive factors. Histopathology 77:700–717. https://doi.org/10.1111/his.14178
Milione M, Maisonneuve P, Pellegrinelli A et al (2018) Ki67 proliferative index of the neuroendocrine component drives MANEC prognosis. Endocr Relat Cancer 25:583–593. https://doi.org/10.1530/ERC-17-0557
Jesinghaus M, Konukiewitz B, Keller G et al (2017) Colorectal mixed adenoneuroendocrine carcinomas and neuroendocrine carcinomas are genetically closely related to colorectal adenocarcinomas. Mod Pathol 30:610–619. https://doi.org/10.1038/modpathol.2016.220
Scardoni M, Vittoria E, Volante M et al (2014) Mixed adenoneuroendocrine carcinomas of the gastrointestinal tract: targeted next-generation sequencing suggests a monoclonal origin of the two components. Neuroendocrinology 100:310–316. https://doi.org/10.1159/000369071
Woischke C, Schaaf CW, Yang H-M et al (2017) In-depth mutational analyses of colorectal neuroendocrine carcinomas with adenoma or adenocarcinoma components. Mod Pathol 30:95–103. https://doi.org/10.1038/modpathol.2016.150
La Rosa S (2021) Challenges in high-grade neuroendocrine neoplasms and mixed neuroendocrine/non-neuroendocrine neoplasms. Endocr Pathol 32:245–257. https://doi.org/10.1007/s12022-021-09676-z
Hechtman JF, Klimstra DS, Nanjangud G et al (2019) Performance of DAXX immunohistochemistry as a screen for DAXX mutations in pancreatic neuroendocrine tumors. Pancreas 48:396–399. https://doi.org/10.1097/MPA.0000000000001256
Marinoni I, Kurrer AS, Vassella E et al (2014) Loss of DAXX and ATRX are associated with chromosome instability and reduced survival of patients with pancreatic neuroendocrine tumors. Gastroenterology 146:453-460.e5. https://doi.org/10.1053/j.gastro.2013.10.020
Singhi AD, Liu T-C, Roncaioli JL et al (2017) Alternative lengthening of telomeres and loss of DAXX/ATRX expression predicts metastatic disease and poor survival in patients with pancreatic neuroendocrine tumors. Clin Cancer Res 23:600–609. https://doi.org/10.1158/1078-0432.CCR-16-1113
Luchini C, Lawlor RT, Bersani S et al (2021) Alternative Lengthening of telomeres (ALT) in pancreatic neuroendocrine tumors: ready for prime-time in clinical practice? Curr Oncol Rep 23:106. https://doi.org/10.1007/s11912-021-01096-w
Marinoni I (2021) Prognostic value of DAXX/ATRX loss of expression and ALT activation in PanNETs: is it time for clinical implementation? Gut. https://doi.org/10.1136/gutjnl-2021-324664 (gutjnl-2021-324664)
Hackeng WM, Morsink FHM, Moons LMG et al (2020) Assessment of ARX expression, a novel biomarker for metastatic risk in pancreatic neuroendocrine tumors, in endoscopic ultrasound fine-needle aspiration. Diagn Cytopathol 48:308–315. https://doi.org/10.1002/dc.24368
VandenBussche CJ, Allison DB, Graham MK et al (2017) Alternative lengthening of telomeres and ATRX/DAXX loss can be reliably detected in FNAs of pancreatic neuroendocrine tumors. Cancer Cytopathol 125:544–551. https://doi.org/10.1002/cncy.21857
Cavalcanti E, Armentano R, Valentini AM et al (2017) Role of PD-L1 expression as a biomarker for GEP neuroendocrine neoplasm grading. Cell Death Dis 8:e3004. https://doi.org/10.1038/cddis.2017.401
Milione M, Miceli R, Barretta F et al (2019) Microenvironment and tumor inflammatory features improve prognostic prediction in gastro-entero-pancreatic neuroendocrine neoplasms. J Pathol Clin Res 5:217–226. https://doi.org/10.1002/cjp2.135
Young K, Lawlor RT, Ragulan C et al (2020) Immune landscape, evolution, hypoxia-mediated viral mimicry pathways and therapeutic potential in molecular subtypes of pancreatic neuroendocrine tumours. Gut. https://doi.org/10.1136/gutjnl-2020-321016 (gutjnl-2020-321016)
Bösch F, Brüwer K, Altendorf-Hofmann A et al (2019) Immune checkpoint markers in gastroenteropancreatic neuroendocrine neoplasia. Endocr Relat Cancer 26:293–301. https://doi.org/10.1530/ERC-18-0494
Vanoli A, Perfetti V, Furlan D et al (2020) Long survival and prolonged remission after surgery and chemotherapy in a metastatic mismatch repair deficient pancreatic neuroendocrine carcinoma with MLH1/PMS2 immunodeficiency and minimal microsatellite shift. Endocr Pathol 31:411–417. https://doi.org/10.1007/s12022-020-09622-5
de Mestier L, Couvelard A, Blazevic A et al (2020) Critical appraisal of MGMT in digestive NET treated with alkylating agents. Endocr Relat Cancer 27:R391–R405. https://doi.org/10.1530/ERC-20-0227
Campana D, Walter T, Pusceddu S et al (2018) Correlation between MGMT promoter methylation and response to temozolomide-based therapy in neuroendocrine neoplasms: an observational retrospective multicenter study. Endocrine 60:490–498. https://doi.org/10.1007/s12020-017-1474-3
Walter T, van Brakel B, Vercherat C et al (2015) O6-methylguanine-DNA methyltransferase status in neuroendocrine tumours: prognostic relevance and association with response to alkylating agents. Br J Cancer 112:523–531. https://doi.org/10.1038/bjc.2014.660
Cros J, Hentic O, Rebours V et al (2016) MGMT expression predicts response to temozolomide in pancreatic neuroendocrine tumors. Endocr Relat Cancer 23:625–633. https://doi.org/10.1530/ERC-16-0117
De Rycke O, Walter T, Perrier M et al (2021) Alkylating agent rechallenge in metastatic pancreatic neuroendocrine tumors. Endocr Relat Cancer 28:457–466. https://doi.org/10.1530/ERC-21-0034
Lacombe C, De Rycke O, Couvelard A et al (2021) Biomarkers of response to etoposide-platinum chemotherapy in patients with grade 3 neuroendocrine neoplasms. Cancers (Basel) 13:643. https://doi.org/10.3390/cancers13040643
Hijioka S, Hosoda W, Matsuo K et al (2017) Rb loss and KRAS mutation are predictors of the response to platinum-based chemotherapy in pancreatic neuroendocrine neoplasm with grade 3: a Japanese multicenter pancreatic NEN-G3 study. Clin Cancer Res 23:4625–4632. https://doi.org/10.1158/1078-0432.CCR-16-3135
Tanaka H, Hijioka S, Hosoda W et al (2020) Pancreatic neuroendocrine carcinoma G3 may be heterogeneous and could be classified into two distinct groups. Pancreatology 20:1421–1427. https://doi.org/10.1016/j.pan.2020.07.400
Fraune C, Simon R, Hube-Magg C et al (2020) Homogeneous MMR deficiency throughout the entire tumor mass occurs in a subset of colorectal neuroendocrine carcinomas. Endocr Pathol 31:182–189. https://doi.org/10.1007/s12022-020-09612-7
Mehnert JM, Bergsland E, O’Neil BH et al (2020) Pembrolizumab for the treatment of programmed death-ligand 1-positive advanced carcinoid or pancreatic neuroendocrine tumors: results from the KEYNOTE-028 study. Cancer 126:3021–3030. https://doi.org/10.1002/cncr.32883
Strosberg J, Mizuno N, Doi T et al (2020) Efficacy and safety of pembrolizumab in previously treated advanced neuroendocrine tumors: results from the phase II KEYNOTE-158 study. Clin Cancer Res 26:2124–2130. https://doi.org/10.1158/1078-0432.CCR-19-3014
MacFarlane AW, Yeung H-M, Alpaugh RK et al (2021) Impacts of pembrolizumab therapy on immune phenotype in patients with high-grade neuroendocrine neoplasms. Cancer Immunol Immunother 70:1893–1906. https://doi.org/10.1007/s00262-020-02811-5
De Dosso S, Treglia G, Pascale M et al (2019) Detection rate of unknown primary tumour by using somatostatin receptor PET/CT in patients with metastatic neuroendocrine tumours: a meta-analysis. Endocrine 64:456–468. https://doi.org/10.1007/s12020-019-01934-9
Imperiale A, Rust E, Gabriel S et al (2014) 18F-fluorodihydroxyphenylalanine PET/CT in patients with neuroendocrine tumors of unknown origin: relation to tumor origin and differentiation. J Nucl Med 55:367–372. https://doi.org/10.2967/jnumed.113.126896
Bellizzi AM (2020) SATB2 in neuroendocrine neoplasms: strong expression is restricted to well-differentiated tumours of lower gastrointestinal tract origin and is most frequent in Merkel cell carcinoma among poorly differentiated carcinomas. Histopathology 76:251–264. https://doi.org/10.1111/his.13943
Yang Z, Klimstra DS, Hruban RH, Tang LH (2017) Immunohistochemical characterization of the origins of metastatic well-differentiated neuroendocrine tumors to the liver. Am J Surg Pathol 41:915–922. https://doi.org/10.1097/PAS.0000000000000876
Zhao L-H, Chen C, Mao C-Y et al (2019) Value of SATB2, ISL1, and TTF1 to differentiate rectal from other gastrointestinal and lung well-differentiated neuroendocrine tumors. Pathol Res Pract 215:152448. https://doi.org/10.1016/j.prp.2019.152448
Hermann G, Konukiewitz B, Schmitt A et al (2011) Hormonally defined pancreatic and duodenal neuroendocrine tumors differ in their transcription factor signatures: expression of ISL1, PDX1, NGN3, and CDX2. Virchows Arch 459:147–154. https://doi.org/10.1007/s00428-011-1118-6
Samdani RT, Wasylishen AR, Halperin DM et al (2019) Loss of menin expression by immunohistochemistry in pancreatic neuroendocrine tumors: comparison between primary and metastatic tumors. Pancreas 48:510–513. https://doi.org/10.1097/MPA.0000000000001274
Simbolo M, Barbi S, Fassan M et al (2019) Gene expression profiling of lung atypical carcinoids and large cell neuroendocrine carcinomas identifies three transcriptomic subtypes with specific genomic alterations. J Thorac Oncol 14:1651–1661. https://doi.org/10.1016/j.jtho.2019.05.003
Tirosh A, Killian JK, Petersen D et al (2020) Distinct DNA methylation signatures in neuroendocrine tumors specific for primary site and inherited predisposition. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgaa477
Gehrcken L, Sauerer T, Schaft N, Dörrie J (2021) T-cell responses in Merkel cell carcinoma: implications for improved immune checkpoint blockade and other therapeutic options. Int J Mol Sci 22:8679. https://doi.org/10.3390/ijms22168679
Shalhout SZ, Emerick KS, Kaufman HL, Miller DM (2021) Immunotherapy for non-melanoma skin cancer. Curr Oncol Rep 23:125. https://doi.org/10.1007/s11912-021-01120-z
Kervarrec T, Tallet A, Miquelestorena-Standley E et al (2019) Diagnostic accuracy of a panel of immunohistochemical and molecular markers to distinguish Merkel cell carcinoma from other neuroendocrine carcinomas. Mod Pathol 32:499–510. https://doi.org/10.1038/s41379-018-0155-y
Yu S, Hornick JL, Gonzalez RS (2021) An algorithmic approach utilizing CK7, TTF1, beta-catenin, CDX2, and SSTR2A can help differentiate between gastrointestinal and pulmonary neuroendocrine carcinomas. Virchows Arch. https://doi.org/10.1007/s00428-021-03085-7
Ahmed M (2020) Gastrointestinal neuroendocrine tumors in 2020. World J Gastrointest Oncol 12:791–807. https://doi.org/10.4251/wjgo.v12.i8.791
Trinh VQ-H, Shi C, Ma C (2020) Gastric neuroendocrine tumours from long-term proton pump inhibitor users are indolent tumours with good prognosis. Histopathology 77:865–876. https://doi.org/10.1111/his.14220
McCarthy DM (2020) Proton pump inhibitor use, hypergastrinemia, and gastric carcinoids-what is the relationship? Int J Mol Sci 21:E662. https://doi.org/10.3390/ijms21020662
Rais R, Trikalinos NA, Liu J, Chatterjee D (2021) Enterochromaffin-like cell hyperplasia-associated gastric neuroendocrine tumors may arise in the setting of proton pump inhibitor use: the need for a new clinicopathologic category. Arch Pathol Lab Med. https://doi.org/10.5858/arpa.2020-0315-OA
de Herder WW, Zandee WT, Hofland J (2000) Somatostatinoma. In: Feingold KR, Anawalt B, Boyce A, et al (eds) Endotext. MDText.com, Inc., South Dartmouth (MA)
Vanoli A, La Rosa S, Klersy C et al (2017) Four neuroendocrine tumor types and neuroendocrine carcinoma of the duodenum: analysis of 203 cases. Neuroendocrinology 104:112–125. https://doi.org/10.1159/000444803
Zakaria A, Hammad N, Vakhariya C, Raphael M (2019) Somatostatinoma presented as double-duct sign. Case Rep Gastrointest Med 2019:9506405. https://doi.org/10.1155/2019/9506405
Wonn SM, Ratzlaff AN, Pommier SJ et al (2021) Evaluation of the prognosis for N2 status in patients with small bowel neuroendocrine tumors. Am J Surg 221:1135–1140. https://doi.org/10.1016/j.amjsurg.2021.03.036
Wu L, Chen F, Chen S, Wang L (2018) The lymph node ratio optimizes staging in patients with small intestinal neuroendocrine tumors. Neuroendocrinology 107:209–217. https://doi.org/10.1159/000491017
Xiao C, Song B, Yi P et al (2020) Deaths of colon neuroendocrine tumors are associated with increasing metastatic lymph nodes and lymph node ratio. J Gastrointest Oncol 11:1146–1154. https://doi.org/10.21037/jgo-20-444
Elias E, Ardalan A, Lindberg M et al (2021) Independent somatic evolution underlies clustered neuroendocrine tumors in the human small intestine. Nat Commun 12:6367. https://doi.org/10.1038/s41467-021-26581-5
Samsom KG, Levy S, van Veenendaal LM et al (2021) Driver mutations occur frequently in metastases of well-differentiated small intestine neuroendocrine tumours. Histopathology 78:556–566. https://doi.org/10.1111/his.14252
Noor M, Huber AR, Cates JMM, Gonzalez RS (2021) Risk factors for progression of appendiceal neuroendocrine tumours: low-stage tumours <5 mm appear to be overwhelmingly indolent and may merit a separate designation. Histopathology 79:416–426. https://doi.org/10.1111/his.14369
Volante M, Grillo F, Massa F et al (2021) Neuroendocrine neoplasms of the appendix, colon and rectum. Pathologica 113:19–27. https://doi.org/10.32074/1591-951X-230
de Mestier L, Lorenzo D, Fine C et al (2019) Endoscopic, transanal, laparoscopic, and transabdominal management of rectal neuroendocrine tumors. Best Pract Res Clin Endocrinol Metab 33:101293. https://doi.org/10.1016/j.beem.2019.101293
Chida K, Watanabe J, Hirasawa K et al (2020) A novel risk-scoring system for predicting lymph node metastasis of rectal neuroendocrine tumors. Ann Gastroenterol Surg 4:562–570. https://doi.org/10.1002/ags3.12355
Author information
Authors and Affiliations
Contributions
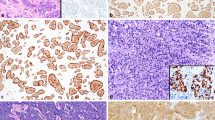
AC and JC were both involved in writing the review, preparing the figures, and correcting the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The authors declare that they have followed the principles of ethical and professional conduct.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Couvelard, A., Cros, J. An update on the development of concepts, diagnostic criteria, and challenging issues for neuroendocrine neoplasms across different digestive organs. Virchows Arch 480, 1129–1148 (2022). https://doi.org/10.1007/s00428-022-03306-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03306-7