Abstract
Background
The neutrophil–lymphocyte ratio (NLR) and platelet distribution width (PDW) are associated with poor prognosis in various cancers. We aimed to analyze the prognostic value of the combination of preoperative NLR and PDW in patients with gallbladder carcinoma (GBC).
Methods
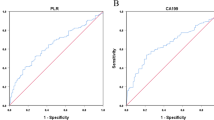
A total of 287 GBC patients who underwent curative-intent surgery in our institution was included. The relationship between NLR and PDW and clinicopathological features were analyzed. The receiver operating characteristic (ROC) curves were used to determine the optimal cutoff value for NLR and PDW. Overall survival (OS) was estimated using the Kaplan–Meier method. Meanwhile, the univariate and multivariate Cox regression models were used to assess the risk factors for OS.
Results
The optimal cutoff value of NLR and PDW was 3.00 and 14.76, respectively. In addition, survival analysis demonstrated that patients with NLR > 3.00 and PDW > 14.76 had a worse prognosis than patients with NLR ≤ 3.00 and PDW ≤ 14.76, respectively. The multivariate analysis showed that NLR and PDW were independent prognostic factors in the patients with GBC. When we combined NLR and PDW, the area under the ROC curve increased from 0.665 (NLR) and 0.632 (PDW) to 0.676. Moreover, the 1-, 3-, and 5-year OS of group A (patients with NLR ≤ 3.00 and PDW ≤ 14.76), group B (patients with either of NLR > 3.00 or PDW > 14.76) and group C (patients with NLR > 3.00 and PDW > 14.76) were 88.7%, 62.6%, 28.1%, 65.1%, 26.9%, 13.1%, and 34.8%, 8.3%, 0%, respectively.
Conclusion
The combination of NLR and PDW may serve as a significant prognostic biomarker for GBC patients superior to either NLR or PDW alone.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. All data generated and analyzed during the current study are included in this article and available from the corresponding author on reasonable request.
References
Roa JC, García P, Kapoor VK, Maithel SK, Javle M, Koshiol J (2022) Gallbladder cancer. Nat Rev Dis Primers 8(1):69
Gunasekaran G, Bekki Y, Lourdusamy V, Schwartz M (2021) Surgical treatments of hepatobiliary cancers. Hepatology (Baltimore, Md.) 73(Suppl 1):128–136
Hickman L, Contreras C (2019) Gallbladder cancer: diagnosis, surgical management, and adjuvant therapies. Surg Clin North America 99(2):337–355
Butte JM, Matsuo K, Gönen M, D’Angelica MI, Waugh E, Allen PJ, Fong Y, DeMatteo RP, Blumgart L, Endo I, De La Fuente H, Jarnagin WR (2011) Gallbladder cancer: differences in presentation, surgical treatment, and survival in patients treated at centers in three countries. J Am Coll Surg 212(1):50–61
Hakeem AR, Papoulas M, Menon KV (2019) The role of neoadjuvant chemotherapy or chemoradiotherapy for advanced gallbladder cancer - A systematic review, European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of. Surg Oncol 45(2):83–91
Abdel-Rahman O, Elsayed Z, Elhalawani H (2018) Gemcitabine-based chemotherapy for advanced biliary tract carcinomas. Cochr Database Syst Rev 4(4):Cd011746
Yifan T, Zheyong L, Miaoqin C, Liang S, Xiujun C (2018) A predictive model for survival of gallbladder adenocarcinoma. Surg Oncol 27(3):365–372
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Grivennikov SI, Greten FR, Karin M (2010) Immunity, inflammation, and cancer. Cell 140(6):883–899
Zhang L, Wang R, Chen W, Xu X, Dong S, Fan H, Liu C (2016) Prognostic significance of neutrophil to lymphocyte ratio in patients with gallbladder carcinoma. HPB (Oxford) 18(7):600–607
Jeong JH, Lim SM, Yun JY, Rhee GW, Lim JY, Cho JY, Kim YR (2012) Comparison of two inflammation-based prognostic scores in patients with unresectable advanced gastric cancer. Oncology 83(5):292–299
He W, Yin C, Guo G, Jiang C, Wang F, Qiu H, Chen X, Rong R, Zhang B, Xia L (2013) Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol (Northwood, London, England) 30(1):439
Stone RL, Nick AM, McNeish IA, Balkwill F, Han HD, Bottsford-Miller J, Rupairmoole R, Armaiz-Pena GN, Pecot CV, Coward J, Deavers MT, Vasquez HG, Urbauer D, Landen CN, Hu W, Gershenson H, Matsuo K, Shahzad MM, King ER, Tekedereli I, Ozpolat B, Ahn EH, Bond VK, Wang R, Drew AF, Gushiken F, Lamkin D, Collins K, DeGeest K, Lutgendorf SK, Chiu W, Lopez-Berestein G, Afshar-Kharghan V, Sood AK (2012) Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med 366(7):610–618
Li N (2016) Platelets in cancer metastasis: To help the “villain” to do evil. Int J Cancer 138(9):2078–2087
Buergy D, Wenz F, Groden C, Brockmann MA (2012) Tumor-platelet interaction in solid tumors. Int J Cancer 130(12):2747–2760
Wang RT, Zhang LQ, Mu YP, Li JB, Xu XS, Pang Q, Sun LK, Zhang X, Dong SB, Wang L, Liu C (2015) Prognostic significance of preoperative platelet count in patients with gallbladder cancer. World J Gastroenterol 21(17):5303–5310
Seretis C, Youssef H, Chapman M (2015) Hypercoagulation in colorectal cancer: what can platelet indices tell us? Platelets 26(2):114–118
Mahdavi-Zafarghandi R, Shakiba B, Keramati MR, Tavakkoli M (2014) Platelet volume indices in patients with varicocele. Clin Exp Reprod Med 41(2):92–95
Zuo X, Kong W, Feng L, Zhang H, Meng X, Chen W (2019) Elevated platelet distribution width predicts poor prognosis in hepatocellular carcinoma. Cancer Biomark : section A of Disease markers 24(3):307–313
Liu F, Hu HJ, Regmi P, Jin YW, Ma WJ, Wang JK, Zou RQ, Li FY (2021) Elevated platelet distribution width predicts poor prognosis in gallbladder carcinoma. Cancer Manag Res 13:4647–4655
Sakin A, Sahin S, Sakin A, Karatas F, SengulSamanci N, Yasar N, Arici S, Demir C, Geredeli C, Dikker O, Cihan S (2020) Mean platelet volume and platelet distribution width correlates with prognosis of early colon cancer. J of B.U.ON: official journal of the Balkan Union of Oncology 25(1):227–239
Regimbeau JM, Fuks D, Bachellier P, Le Treut YP, Pruvot FR, Navarro F, Chiche L, Farges O (2011) Prognostic value of jaundice in patients with gallbladder cancer by the AFC-GBC-2009 study group, European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of. Surg Oncol 37(6):505–512
Wang JW, Peng SY, Li JT, Wang Y, Zhang ZP, Cheng Y, Cheng DQ, Weng WH, Wu XS, Fei XZ, Quan ZW, Li JY, Li SG, Liu YB (2009) Identification of metastasis-associated proteins involved in gallbladder carcinoma metastasis by proteomic analysis and functional exploration of chloride intracellular channel 1. Cancer Lett 281(1):71–81
Li D, Yang Z, Liu Z, Zou Q, Yuan Y (2020) Clinical Significance of CBS and CCL21 in Gallbladder Adenocarcinomas and Squamous Cell/Adenosquamous Carcinomas. Appl Immunohistochem Mol Morphol : AIMM 28(2):103–110
Gregory AD, Houghton AM (2011) Tumor-associated neutrophils: new targets for cancer therapy. Can Res 71(7):2411–2416
Dunn GP, Old LJ, Schreiber RD (2004) The immunobiology of cancer immunosurveillance and immunoediting. Immunity 21(2):137–148
Halazun KJ, Hardy MA, Rana AA, Woodland DCT, Luyten EJ, Mahadev S, Witkowski P, Siegel AB, Brown RS Jr, Emond JC (2009) Negative impact of neutrophil-lymphocyte ratio on outcome after liver transplantation for hepatocellular carcinoma. Annal Surg 250(1):141–51
Zhang Y, Jiang C, Li J, Sun J, Qu X (2015) Prognostic significance of preoperative neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in patients with gallbladder carcinoma. Clin Transl Oncol : official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico 17(10):810–818
Liu F, Hu HJ, Ma WJ, Yang Q, Wang JK, Li FY (2019) Prognostic significance of neutrophil-lymphocyte ratio and carbohydrate antigen 19–9 in patients with gallbladder carcinoma. Medicine 98(8):e14550
Beal EW, Wei L, Ethun CG, Black SM, Dillhoff M, Salem A, Weber SM, Tran T, Poultsides G, Son AY, Hatzaras I, Jin L, Fields RC, Buettner S, Pawlik TM, Scoggins C, Martin RC, Isom CA, Idrees K, Mogal HD, Shen P, Maithel SK, Schmidt CR (2016) Elevated NLR in gallbladder cancer and cholangiocarcinoma - making bad cancers even worse: results from the US Extrahepatic Biliary Malignancy Consortium. HPB (Oxford) 18(11):950–957
Bartlett DL, Fong Y, Fortner JG, Brennan MF, Blumgart LH (1996) Long-term results after resection for gallbladder cancer Implications for staging and management. Annal Surg 224(5):639–646
Funding
This work was supported by1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC21046); 1.3.5 project for disciplines of excellence-Clinical Research Incubation Project, West China Hospital, Sichuan University (2021HXFH001);Sichuan University-Zigong School-local Cooperation project (2021CDZG-23); Sichuan University-Sui Lin School-local Cooperation project (2022CDSN-18); Science and Technology project of the Health planning committee of Sichuan (21PJ046);National Natural Science Foundation of China for Young Scientists Fund (82303669);China Telecom Sichuan Company Biliary tract Tumor Big Data Platform and Application Phase I R&D Project(312230752).
Author information
Authors and Affiliations
Contributions
Fei Liu and Jun-Ke Wang contributed to the data acquisition and drafted the manuscript. Wen-Jie Ma and Hai-Jie Hu contributed to data acquisition. Fu-Yu Li and Yan-Wen Jin contributed to the study design and revised the manuscript. Manuscript is approved by all authors for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study conforms to the criteria of the Helsinki Declaration and current ethical guideline, and was approved by the Institutional Ethical Board of West China Hospital of Sichuan University (20231394).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, F., Wang, JK., Ma, WJ. et al. Prognostic value of combined preoperative inflammatory marker neutrophil–lymphocyte ratio and platelet distribution width in patients with gallbladder carcinoma. Langenbecks Arch Surg 409, 51 (2024). https://doi.org/10.1007/s00423-024-03247-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03247-6