Abstract
Background
Gastric cancer is a major public health problem around the globe. With the standardization of tumor treatment, surgery continues to be the most important treatment method for gastric cancer. However, changes in body composition and nutrition index parameters in patients with Billroth II and Roux-en-Y anastomosis following totally laparoscopic distal gastrectomy (TLDG) remain unclear.
Methods
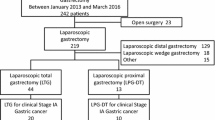
This was a single-center retrospective study. A total of 369 patients who underwent TLDG at the First Affiliated Hospital of Soochow University (Suzhou, China) between January 2016 and February 2019 were included and assigned to the Billroth II group or Roux-en-Y group according to the anastomosis method. After propensity score matching, body composition and relevant clinical data were compared between the two groups.
Results
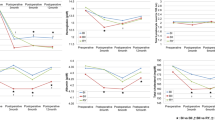
The operation time for the Billroth II group was significantly shorter than for the Roux-en-Y group (174.12 ± 39.33 min vs. 229.19 ± 28.12 min, P < 0.001). In addition, the Billroth II group showed lower skeletal muscle loss. Specifically, the Billroth II group showed a − 4.77 ± 4.88% change in the skeletal muscle index (SMI), whereas the Roux-en-Y group showed a − 11.89 ± 8.68% change (P = 0.001). The Billroth II group also showed a smaller decrease in BMI than the Roux-en-Y group (− 6.67 ± 7.76% vs. − 13.12 ± 10.79%, P = 0.018).
Conclusions
These results suggest that Billroth II anastomosis after TLDG has advantages over Roux-en-Y for maintaining patient body composition, especially in terms of SMI, and may serve as a useful reference when choosing an anastomosis method.


Similar content being viewed by others
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T, Baba H (2009) Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc 23(10):2374–2379
Lee MS, Ahn SH, Lee JH, Park DJ, Lee HJ, Kim HH, Yang HK, Kim N, Lee WW (2012) What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc 26(6):1539–1547
Tran TB, Worhunsky DJ, Squires MH, Jin LX, Spolverato G, Votanopoulos KI, Cho CS, Weber SM, Schmidt C, Levine EA, Bloomston M, Fields RC, Pawlik TM, Maithel SK, Norton JA, Poultsides GA (2016) To Roux or not to Roux: a comparison between Roux-en-Y and Billroth II reconstruction following partial gastrectomy for gastric cancer. Gastric Cancer 19(3):994–1001
Lee K, Kim KW, Lee JB, Shin Y, Jang JK, Yook JH, Kim BS, Lee IS (2019) Impact of remnant stomach volume and anastomosis on nutrition and body composition in gastric cancer patients. Surg Oncol 31:75–82
Kamarajah SK, Bundred J, Tan BHL (2019) Body composition assessment and sarcopenia in patients with gastric cancer: a systematic review and meta-analysis. Gastric Cancer 22(1):10–22
Zelnick R, Auguste LJ, Wise L (1989) Nutritional effects of postgastrectomy reconstruction: a clinical evaluation. J Surg Oncol 40(4):219–221
Kiyama T, Mizutani T, Okuda T, Fujita I, Tokunaga A, Tajiri T, Barbul A (2005) Postoperative changes in body composition after gastrectomy. J Gastrointest Surg 9(3):313–319
Park HS, Kim HS, Beom SH, Rha SY, Chung HC, Kim JH, Chun YJ, Lee SW, Choe EA, Heo SJ, Noh SH, Hyung WJ, Cheong JH, Kim HI, Son T, Lim JS, Baek SE, Jung M (2018) Marked loss of muscle, visceral fat, or subcutaneous fat after gastrectomy predicts poor survival in advanced gastric cancer: single-center study from the CLASSIC Trial. Ann Surg Oncol 25(11):3222–3230
Distrutti E, Monaldi L, Ricci P, Fiorucci S (2016) Gut microbiota role in irritable bowel syndrome: new therapeutic strategies. World J Gastroenterol 22(7):2219–2241
Shizgal HM (1985) Body composition of patients with malnutrition and cancer Summary of methods of assessment. Cancer 55(1 Suppl):250–253
Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, Baracos VE (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635
Yip C, Dinkel C, Mahajan A, Siddique M, Cook GJ, Goh V (2015) Imaging body composition in cancer patients: visceral obesity, sarcopenia and sarcopenic obesity may impact on clinical outcome. Insights Imaging 6(4):489–497
Yip C, Dinkel C, Mahajan A, Siddique M, Cook GJR, Goh V (2015) Imaging body composition in cancer patients: visceral obesity, sarcopenia and sarcopenic obesity may impact on clinical outcome. Insights Imaging 6(4):489–497
Seeruttun SR, Yuan S, Qiu H, Huang Y, Li Y, Liang Y, Guan Y, Zhan Y, Li W, Chen Y, Sun X, Xu D, Zhou Z (2017) A comprehensive analysis comparing the eighth AJCC gastric cancer pathological classification to the seventh, sixth, and fifth editions. Cancer Med 6(12):2804–2813
Yang D, He L, Tong WH, Jia ZF, Su TR, Wang Q (2017) Randomized controlled trial of uncut Roux-en-Y vs Billroth II reconstruction after distal gastrectomy for gastric cancer: which technique is better for avoiding biliary reflux and gastritis? World J Gastroenterol 23(34):6350–6356
Ma Z, Wang Z, Zhang J (2001) Carcinogenicity of duodenogastric reflux juice in patients undergoing gastrectomy. Zhonghua Wai Ke Za Zhi 39(10):764–766
Shimoda M, Kubota K, Katoh M, Kita J (2013) Effect of billroth II or Roux-en-Y reconstruction for the gastrojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled study. Ann Surg 257(5):938–942
So JB, Rao J, Wong AS, Chan YH, Pang NQ, Tay AYL, Yung MY, Su Z, Phua JNS, Shabbir A, Ng EKW (2018) Roux-en-Y or Billroth II reconstruction after radical distal gastrectomy for gastric cancer: a multicenter randomized controlled trial. Ann Surg 267(2):236–242
Johnsson F, Joelsson B, Gudmundsson K, Greiff L (1987) Symptoms and endoscopic findings in the diagnosis of gastroesophageal reflux disease. Scand J Gastroenterol 22(6):714–718
Xiong JJ, Altaf K, Javed MA, Nunes QM, Huang W, Mai G, Tan CL, Mukherjee R, Sutton R, Hu WM, Liu XB (2013) Roux-en-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol 19(7):1124–1134
Taylor PR, Mason RC, Filipe MI, Vaja S, Hanley DC, Murphy GM, Dowling RH, Mccoll I (1991) Gastric carcinogenesis in the rat induced by duodenogastric reflux without carcinogens - morphology, mucin histochemistry, polyamine metabolism, and labeling index. Gut 32(12):1447–1454
Gustavsson S, Ilstrup DM, Morrison P, Kelly KA (1988) Roux-Y stasis syndrome after gastrectomy. Am J Surg 155(3):490–494
Mathias JR, Fernandez A, Sninsky CA, Clench MH, Davis RH (1985) Nausea, vomiting, and abdominal pain after Roux-en-Y anastomosis: motility of the jejunal limb. Gastroenterology 88(1 Pt 1):101–107
Ongaro E, Buoro V, Cinausero M, Caccialanza R, Turri A, Fanotto V, Basile D, Vitale MG, Ermacora P, Cardellino GG, Nicoletti L, Fornaro L, Casadei-Gardini A, Aprile G (2017) Sarcopenia in gastric cancer: when the loss costs too much. Gastric Cancer 20(4):563–572
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE (2012) Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer 107(6):931–936
Tegels JJ, van Vugt JL, Reisinger KW, Hulsewe KW, Hoofwijk AG, Derikx JP, Stoot JH (2015) Sarcopenia is highly prevalent in patients undergoing surgery for gastric cancer but not associated with worse outcomes. J Surg Oncol 112(4):403–407
Li XT, Tang L, Chen Y, Li YL, Zhang XP, Sun YS (2015) Visceral and subcutaneous fat as new independent predictive factors of survival in locally advanced gastric carcinoma patients treated with neo-adjuvant chemotherapy. J Cancer Res Clin Oncol 141(7):1237–1247
Antoun S, Bayar A, Ileana E, Laplanche A, Fizazi K, di Palma M, Escudier B, Albiges L, Massard C, Loriot Y (2015) High subcutaneous adipose tissue predicts the prognosis in metastatic castration-resistant prostate cancer patients in post chemotherapy setting. Eur J Cancer 51(17):2570–2577
Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R (2002) Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr 75(4):683–688
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa S, Maeda S, Uemura M, Miyake M, Hama N, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T (2016) Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer 19(3):986–993
Wang SL, Zhuang CL, Huang DD, Pang WY, Lou N, Chen FF, Zhou CJ, Shen X, Yu Z (2016) Sarcopenia adversely impacts postoperative clinical outcomes following gastrectomy in patients with gastric cancer: a prospective study. Ann Surg Oncol 23(2):556–564
Zhuang CL, Huang DD, Pang WY, Zhou CJ, Wang SL, Lou N, Ma LL, Yu Z, Shen X (2016) Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: analysis from a large-scale cohort. Medicine (Baltimore) 95(13):e3164
Thirlby RC, Bahiraei F, Randall J, Drewnoski A (2006) Effect of Roux-en-Y gastric bypass on satiety and food likes: the role of genetics. J Gastrointest Surg 10(2):270–277
Lin XH, Huang KH, Chuang WH, Luo JC, Lin CC, Ting PH, Young SH, Fang WL, Hou MC, Lee FY (2018) The long term effect of metabolic profile and microbiota status in early gastric cancer patients after subtotal gastrectomy. PLoS One 13(11):e0206930
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, Mariat D, Corthier G, Dore J, Henegar C, Rizkalla S, Clement K (2010) Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 59(12):3049–3057
Graessler J, Qin Y, Zhong H, Zhang J, Licinio J, Wong ML, Xu A, Chavakis T, Bornstein AB, Ehrhart-Bornstein M, Lamounier-Zepter V, Lohmann T, Wolf T, Bornstein SR (2013) Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J 13(6):514–522
Kong LC, Tap J, Aron-Wisnewsky J, Pelloux V, Basdevant A, Bouillot JL, Zucker JD, Dore J, Clement K (2013) Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am J Clin Nutr 98(1):16–24
Clemente-Postigo M, Roca-Rodriguez Mdel M, Camargo A, Ocana-Wilhelmi L, Cardona F, Tinahones FJ (2015) Lipopolysaccharide and lipopolysaccharide-binding protein levels and their relationship to early metabolic improvement after bariatric surgery. Surg Obes Relat Dis 11(4):933–939
Cani PD, Everard A, Duparc T (2013) Gut microbiota, enteroendocrine functions and metabolism. Curr Opin Pharmacol 13(6):935–940
Long SL, Gahan CGM, Joyce SA (2017) Interactions between gut bacteria and bile in health and disease. Mol Aspects Med 56:54–65
Lin JX, Lin JP, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M, Tu R, Zheng CH, Huang CM, Li P (2019) Prognostic value and association of sarcopenia and systemic inflammation for patients with gastric cancer following radical gastrectomy. Oncologist 24(11):e1091–e1101
Fukuda T, Seto Y, Yamada K, Hiki N, Fukunaga T, Oyama S, Yamaguchi T (2008) Can immune-enhancing nutrients reduce postoperative complications in patients undergoing esophageal surgery? Dis Esophagus 21(8):708–711
Harada K, Ida S, Baba Y, Ishimoto T, Kosumi K, Tokunaga R, Izumi D, Ohuchi M, Nakamura K, Kiyozumi Y, Imamura Y, Iwatsuki M, Iwagami S, Miyamoto Y, Sakamoto Y, Yoshida N, Watanabe M, Baba H (2016) Prognostic and clinical impact of sarcopenia in esophageal squamous cell carcinoma. Dis Esophagus 29(6):627–633
Wagner D, DeMarco MM, Amini N, Buttner S, Segev D, Gani F, Pawlik TM (2016) Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg 8(1):27–40
Heymsfield SB (2008) Development of imaging methods to assess adiposity and metabolism. Int J Obes (Lond) 32(Suppl 7):S76-82
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was not funded. Author Jiawen Zhang declares that he has no conflict of interest. Author Linhua Jiang declares that he has no conflict of interest. Author Xinguo Zhu declares that he has no conflict of interest. The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Soochow University. This project was conducted as a retrospective observational study; the study protocol involved minimal risk and did not threaten the health of the subjects. And, all participating patients signed informed consents. This project was conducted in compliance with the spirit of the “Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects” (as amended in Fortaleza, October 2013).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, L., Zhang, J. & Zhu, X. Billroth II anastomosis maintains SMI and BMI better than Roux-en-Y anastomosis following totally laparoscopic distal gastrectomy: a propensity score-matched study. Langenbecks Arch Surg 407, 1441–1450 (2022). https://doi.org/10.1007/s00423-022-02459-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02459-y