Abstract
Purpose
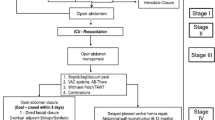
Therapeutic approaches for septic open abdomen treatment remain a major challenge with many uncertainties. The most convincing method is vacuum-assisted wound closure with mesh-mediated fascia traction with a protective plastic sheet placed on the viscera. As this plastic sheet and the mesh must be removed before final fascial closure, such a technique only allows temporary abdominal closure. This retrospective study analyzes the results of a modification of this technique allowing final abdominal closure using an anti-adhesive permeable polyvinylidene fluoride (PVDF) mesh.
Methods
The outcome of all consecutive patients with septic open abdomen treatment at one academic surgical department from January 2013 to June 2015 was retrospectively analyzed.
Results
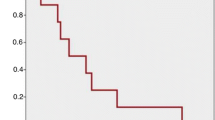
Retrospectively, 57 severely ill consecutive patients with septic open abdomen treatment with a 30-day mortality of 26% and a 2-year mortality of 51% were included in the study. In 26 patients, no mesh was implanted; in 31 patients, mesh implantation was done at median third-look laparotomy, median 5 days postoperative. Re-laparotomies after mesh implantation (median n = 2) revealed anastomotic leakage in 16% but no new bowel fistula. In 40% of those patients who had mesh implantation, fascia closure was not achieved and the mesh was left in place in a bridging position avoiding planned ventral hernia.
Conclusion
The application of an anti-adhesive PVDF mesh for fascia traction in vacuum-assisted wound closure of septic open abdomen is novel, versatile, and seems to be safe. It offers the highly relevant possibility for provisional and final abdominal closure.


Similar content being viewed by others
References
Roberts DJ, Ball CG, Kirkpatrick AW (2016) Increased pressure within the abdominal compartment: intra-abdominal hypertension and the abdominal compartment syndrome. Curr Opin Crit Care 22(2):174–185. https://doi.org/10.1097/MCC.0000000000000289
van Ruler O, Mahler CW, Boer KR, Reuland EA, Gooszen HG, Opmeer BC, de Graaf PW, Lamme B, Gerhards MF, Steller EP, van Till JW, de Borgie CJ, Gouma DJ, Reitsma JB, Boermeester MA, Dutch Peritonitis Study G (2007) Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: a randomized trial. JAMA: the Journal of the American Medical Association 298(8):865–872. https://doi.org/10.1001/jama.298.8.865
Strobel O, Werner J, Buchler MW (2011) Surgical therapy of peritonitis. Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizin 82(3):242–248. https://doi.org/10.1007/s00104-010-2015-2
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM (2014) Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 42(8):1749–1755. https://doi.org/10.1097/CCM.0000000000000330
Sartelli M, Abu-Zidan FM, Ansaloni L, Bala M, Beltran MA, Biffl WL, Catena F, Chiara O, Coccolini F, Coimbra R, Demetrashvili Z, Demetriades D, Diaz JJ, Di Saverio S, Fraga GP, Ghnnam W, Griffiths EA, Gupta S, Hecker A, Karamarkovic A, Kong VY, Kafka-Ritsch R, Kluger Y, Latifi R, Leppaniemi A, Lee JG, McFarlane M, Marwah S, Moore FA, Ordonez CA, Pereira GA, Plaudis H, Shelat VG, Ulrych J, Zachariah SK, Zielinski MD, Garcia MP, Moore EE (2015) The role of the open abdomen procedure in managing severe abdominal sepsis: WSES position paper. World Journal of Emergency Surgery: WJES 10:35. https://doi.org/10.1186/s13017-015-0032-7
Sartelli M, Abu-Zidan FM, Catena F, Griffiths EA, Di Saverio S, Coimbra R, Ordonez CA, Leppaniemi A, Fraga GP, Coccolini F, Agresta F, Abbas A, Abdel Kader S, Agboola J, Amhed A, Ajibade A, Akkucuk S, Alharthi B, Anyfantakis D, Augustin G, Baiocchi G, Bala M, Baraket O, Bayrak S, Bellanova G, Beltran MA, Bini R, Boal M, Borodach AV, Bouliaris K, Branger F, Brunelli D, Catani M, Che Jusoh A, Chichom-Mefire A, Cocorullo G, Colak E, Costa D, Costa S, Cui Y, Curca GL, Curry T, Das K, Delibegovic S, Demetrashvili Z, Di Carlo I, Drozdova N, El Zalabany T, Enani MA, Faro M, Gachabayov M, Gimenez Maurel T, Gkiokas G, Gomes CA, Gonsaga RA, Guercioni G, Guner A, Gupta S, Gutierrez S, Hutan M, Ioannidis O, Isik A, Izawa Y, Jain SA, Jokubauskas M, Karamarkovic A, Kauhanen S, Kaushik R, Kenig J, Khokha V, Kim JI, Kong V, Koshy R, Krasniqi A, Kshirsagar A, Kuliesius Z, Lasithiotakis K, Leao P, Lee JG, Leon M, Lizarazu Perez A, Lohsiriwat V, Lopez-Tomassetti Fernandez E, Lostoridis E, Mn R, Major P, Marinis A, Marrelli D, Martinez-Perez A, Marwah S, McFarlane M, Melo RB, Mesina C, Michalopoulos N, Moldovanu R, Mouaqit O, Munyika A, Negoi I, Nikolopoulos I, Nita GE, Olaoye I, Omari A, Ossa PR, Ozkan Z, Padmakumar R, Pata F, Pereira Junior GA, Pereira J, Pintar T, Pouggouras K, Prabhu V, Rausei S, Rems M, Rios-Cruz D, Sakakushev B, Sanchez de Molina ML, Seretis C, Shelat V, Simoes RL, Sinibaldi G, Skrovina M, Smirnov D, Spyropoulos C, Tepp J, Tezcaner T, Tolonen M, Torba M, Ulrych J, Uzunoglu MY, van Dellen D, van Ramshorst GH, Vasquez G, Venara A, Vereczkei A, Vettoretto N, Vlad N, Yadav SK, Yilmaz TU, Yuan KC, Zachariah SK, Zida M, Zilinskas J, Ansaloni L (2015) Global validation of the WSES sepsis severity score for patients with complicated intra-abdominal infections: a prospective multicentre study (WISS Study). World Journal of Emergency Surgery: WJES 10:61. https://doi.org/10.1186/s13017-015-0055-0
Champault G, Magnier M, Psalmon F, Patel JC (1979) Controlled evisceration in the treatment of severe peritonitis. Chirurgie; memoires de l’Academie de chirurgie 105(9):866–869
Steinberg D (1979) On leaving the peritoneal cavity open in acute generalized suppurative peritonitis. Am J Surg 137(2):216–220
Quyn AJ, Johnston C, Hall D, Chambers A, Arapova N, Ogston S, Amin AI (2012) The open abdomen and temporary abdominal closure systems–historical evolution and systematic review. Color Dis 14(8):e429–e438. https://doi.org/10.1111/j.1463-1318.2012.03045.x
Koniaris LG, Hendrickson RJ, Drugas G, Abt P, Schoeniger LO (2001) Dynamic retention: a technique for closure of the complex abdomen in critically ill patients. Arch Surg 136(12):1359–1362 discussion 1363
Wittmann DH, Aprahamian C, Bergstein JM (1990) Etappenlavage: advanced diffuse peritonitis managed by planned multiple laparotomies utilizing zippers, slide fastener, and Velcro analogue for temporary abdominal closure. World J Surg 14(2):218–226
Brock WB, Barker DE, Burns RP (1995) Temporary closure of open abdominal wounds: the vacuum pack. Am Surg 61(1):30–35
Miller PR, Thompson JT, Faler BJ, Meredith JW, Chang MC (2002) Late fascial closure in lieu of ventral hernia: the next step in open abdomen management. J Trauma 53(5):843–849. https://doi.org/10.1097/01.TA.0000027879.14969.C9
Miller PR, Meredith JW, Johnson JC, Chang MC (2004) Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg 239(5):608–614 discussion 614-606
Perez D, Wildi S, Demartines N, Bramkamp M, Koehler C, Clavien PA (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205(4):586–592. https://doi.org/10.1016/j.jamcollsurg.2007.05.015
Herrle F, Hasenberg T, Fini B, Jonescheit J, Shang E, Kienle P, Post S, Niedergethmann M (2011) Open abdomen 2009. A national survey of open abdomen treatment in Germany. Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizin 82(8):684–690. https://doi.org/10.1007/s00104-010-2042-z
Petersson U, Acosta S, Bjorck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction–a novel technique for late closure of the open abdomen. World J Surg 31(11):2133–2137. https://doi.org/10.1007/s00268-007-9222-0
Salman AE, Yetisir F, Aksoy M, Tokac M, Yildirim MB, Kilic M (2014) Use of dynamic wound closure system in conjunction with vacuum-assisted closure therapy in delayed closure of open abdomen. Hernia: the Journal of Hernias and Abdominal Wall Surgery 18(1):99–104. https://doi.org/10.1007/s10029-012-1008-0
Verdam FJ, Dolmans DE, Loos MJ, Raber MH, de Wit RJ, Charbon JA, Vroemen JP (2011) Delayed primary closure of the septic open abdomen with a dynamic closure system. World J Surg 35(10):2348–2355. https://doi.org/10.1007/s00268-011-1210-8
Rasilainen SK, Mentula PJ, Leppaniemi AK (2012) Vacuum and mesh-mediated fascial traction for primary closure of the open abdomen in critically ill surgical patients. Br J Surg 99(12):1725–1732. https://doi.org/10.1002/bjs.8914
Atema JJ, Gans SL, Boermeester MA (2015) Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg 39(4):912–925. https://doi.org/10.1007/s00268-014-2883-6
Robledo FA, Luque-de-Leon E, Suarez R, Sanchez P, de-la-Fuente M, Vargas A, Mier J (2007) Open versus closed management of the abdomen in the surgical treatment of severe secondary peritonitis: a randomized clinical trial. Surg Infect 8(1):63–72. https://doi.org/10.1089/sur.2006.8.016
Salamone G, Licari L, Guercio G, Comelli A, Mangiapane M, Falco N, Tutino R, Bagarella N, Campanella S, Porrello C, Gullo R, Cocorullo G, Gulotta G (2018) Vacuum-assisted wound closure with mesh-mediated fascial traction achieves better outcomes than vacuum-assisted wound closure alone: a comparative study. World J Surg 42(6):1679–1686. https://doi.org/10.1007/s00268-017-4354-3
Rasilainen SK, Mentula PJ, Leppaniemi AK (2016) Components separation technique is feasible for assisting delayed primary fascial closure of open abdomen. Scandinavian Journal of Surgery: Official Organ for the Finnish Surgical Society and the Scandinavian Surgical Society 105(1):17–21. https://doi.org/10.1177/1457496915586651
Rausei S, Dionigi G, Boni L, Rovera F, Minoja G, Cuffari S, Dionigi R (2014) Open abdomen management of intra-abdominal infections: analysis of a twenty-year experience. Surg Infect 15(3):200–206. https://doi.org/10.1089/sur.2012.180
Kushimoto S, Yamamoto Y, Aiboshi J, Ogawa F, Koido Y, Yoshida R, Kawai M (2007) Usefulness of the bilateral anterior rectus abdominis sheath turnover flap method for early fascial closure in patients requiring open abdominal management. World J Surg 31(1):2–8; discussion 9-10. https://doi.org/10.1007/s00268-006-0282-3
Berrevoet F (2018) Prevention of incisional hernias after open abdomen treatment. Frontiers in surgery 5:11. https://doi.org/10.3389/fsurg.2018.00011
Lamme B, Boermeester MA, Belt EJ, van Till JW, Gouma DJ, Obertop H (2004) Mortality and morbidity of planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Br J Surg 91(8):1046–1054. https://doi.org/10.1002/bjs.4517
Tsuei BJ, Skinner JC, Bernard AC, Kearney PA, Boulanger BR (2004) The open peritoneal cavity: etiology correlates with the likelihood of fascial closure. Am Surg 70(7):652–656
Arai M, Kushimoto S, Kim S, Masuno T, Hagiwara J, Ishii H, Yokota H (2015) A novel technique for managing open abdomen with the combined use of mesh-mediated traction and the bilateral anterior rectus abdominis sheath turnover flap method: how to do it. Surg Today 45(10):1335–1339. https://doi.org/10.1007/s00595-015-1133-3
Willms A, Schaaf S, Schwab R, Richardsen I, Bieler D, Wagner B, Gusgen C (2016) Abdominal wall integrity after open abdomen: long-term results of vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM). Hernia: the Journal of Hernias and Abdominal Wall Surgery 20(6):849–858. https://doi.org/10.1007/s10029-016-1534-2
Rao M, Burke D, Finan PJ, Sagar PM (2007) The use of vacuum-assisted closure of abdominal wounds: a word of caution. Color Dis 9(3):266–268. https://doi.org/10.1111/j.1463-1318.2006.01154.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study has not been funded. All authors have declared that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
With permission of the University of Zurich Ethics Commission (BASEC No 2016-00164), this retrospective study on all consecutive patients with open abdomen treatment at one institution from January 2013 to June 2015 was performed. Mainly due to high mortality, informed consent could not be obtained from all individuals included in this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Käser, S.A., Brosi, P., Clavien, P.A. et al. Blurring the boundary between open abdomen treatment and ventral hernia repair. Langenbecks Arch Surg 404, 489–494 (2019). https://doi.org/10.1007/s00423-019-01757-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01757-2