Abstract
Purpose
In critically ill patients, length of antibiotic treatment can be effectively guided by procalcitonin (PCT) protocols. International sepsis guidelines and guidelines on antibiotic stewardship strategies recommend PCT as helpful laboratory marker for a rational use of antibiotics. A number of studies and meta-analyses have confirmed the effectiveness of PCT-protocols for shortening antibiotic treatment without compromising clinical outcome in critically ill patients. But in clinical practice, there is still uncertainty how to interpret PCT levels and how to adjust antibiotic treatment in various infectious situations, especially in the perioperative period.
Methods
This narrative review gives an overview on the application of PCT-protocols in critically ill patients with severe bacterial infections on the basis of 5 case reports and the available literature. Beside strengths and limitations of this biomarker, also varying kinetics and different maximum values with regard to the infectious focus and pathogens are discussed.
Results
PCT-guided antibiotic treatment appears to be safe and effective. Most of the studies revealed a shorter antibiotic treatment without negative clinical outcomes. Cost effectiveness is still a matter of debate and effects on bacterial resistance due to shorter treatments, possible lower rates of drug-related adverse events, or decreased rates of Clostridium difficile infections are not yet evaluated.
Conclusion
Guidance of antibiotic treatment can effectively be supported by PCT-protocols. However, it is important to consider the limitations of this biomarker and to use PCT protocols along with antibiotic stewardship programmes and regular clinical rounds together with infectious diseases specialists.
Similar content being viewed by others
Introduction
Initiation of antibiotic treatment in critically ill patients should be based on clinical signs and symptoms, because currently no biochemical test allows a reliable diagnosis of infections or indicates the development of severe sepsis or septic shock early enough for timely therapeutic intervention. Once antibiotic treatment has been started, there is often uncertainty about the length of antibiotic therapy and, therefore, treatment is frequently extended beyond the international guideline recommendations of 7–10 days in patients with severe sepsis [1]. However, studies in patients with ventilator-associated pneumonia have clearly shown that a restricted antibiotic regimen of 7–8 days is safe and effective as long as infections caused by specific bacteria such as Pseudomonas spp. or Acinetobacter spp. are absent [2]. A recent study in septic patients with complicated intraabdominal infections who had undergone an adequate source-control procedure, the outcomes after fixed-duration antibiotic therapy (approximately 4 days) were similar to those after a longer course of antibiotics of aproximately 8 days that extended until after the resolution of physiological abnormalities [3].
Prolonged antibiotic therapy is associated with drug-related side effects, increased bacterial resistances, and escalating costs [4]. In this context, highly sensitive PCT tests have proven as a helpful marker for decision-making on when to stop antibiotic treatment in critically ill patients with bacterial sepsis leading to shorter antibiotic exposure without negative impact on further clinical course and outcome [5, 6], and a very recent large multicenter study has shown a decreased mortality in a mixed ICU population in the PCT-guided group [7]. However, it is important to adhere to established protocols with daily PCT monitoring to assess the dynamics of this biomarker [8]. Clinical studies in various diseases have shown that PCT-guided algorithms result in positive long-term effects with respect to frequency and length of antibiotic treatment in intensive care patients [9, 10]. Clinicians have to keep in mind that trauma, surgical interventions, or multi-organ failure may lead to increased PCT levels in the absence of underlying infections [11, 12]. In addition, the degree of systemic PCT release may vary depending on the site of the infectious focus and the type of bacteria [13, 14].
As shown in a recent multi-center study, PCT-guided escalation of antibiotic treatment along with extended diagnostic measures leads to higher complication rates, increased use of broad-spectrum antibiotics, and prolonged ICU stay [15]. Surgical patients enrolled in this study might have shown unspeficic high PCT levels not necessarily pointing to postoperative infections. For the daily clinical use, it is therefore essential to be aware of the kinetics and limitations of this biomarker. Any PCT measurement needs close correlation with the patients’ clinical presentation. The aim of this article is to give the reader a practical overview on the use of PCT-guided antibiotic treatment in critically ill patients based on five characteristic clinical examples together with a critical review of the available literature on PCT-guided antibiotic decision-making in the ICU.
Methods
In this study, we report on the effectiveness of PCT-guided antibiotic treatment in intensive care medicine based on five cases. Ethics approval was waived by the local ethics committee of the Landesärztekammer Nordrhein (LÄK Nordrhein 240–2015) due to retrospective and anonymous nature of the analysis. Based on five case reports and the available literature, PCT-guided antibiotic treatment in critically ill patients is discussed in this narrative review.
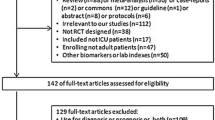
The PCT-protocol used in our ICU is shown in Fig. 1. Key elements of this algorithm are the following:
-
Start of antibiotic treatment in critically ill patients is based on a clinical decision, e. g., clinical signs of sepsis.
-
The protocol should be used to support the clinician’s decision to continue or stop antibiotic treatment in septic patients in which appropriate source control had been achieved.
-
Antibiotic treatment should be discontinued when PCT levels decrease to at least 20 % of peak level or below 0.5 ng/ml together with a clinical improvement.
-
If PCT levels do not decrease adequately in a recovering patient, look for conditions which may rise PCT unrelated to bacterial infections (e.g. surgical procedures or renal replacement therapy).
PCT protocol used in our ICU. Start of antibiotic treatment is based on a clinical decision. According to this algorithm, antibiotics should be discontinued when clinical improvement goes along with decreasing PCT levels. The protocol can be overruled by the means of the attending physician due to clinical reasons or when conditions are present which require a prolonged antibiotic treatment (e.g. endocarditis, osteomyelitis, S. aureus sepsis etc)
Clinical cases
Case 1
A 75-year-old multimorbid female patient (arterial hypertension, coronary artery disease (CAD), congestive heart failure NYHA II, atrial fibrillation, chronic renal failure stage II KDIGO) presented with clinical signs of severe urosepsis due to right-sided hydronephrosis. Following insertion of a ureter stent, she remained intubated, ventilated, and analgosedated, and was transferred to the intensive care unit. Septic shock treatment was initiated with fluid replacement and vasopressors, mechanical ventilation had to be continued due to pulmonary failure. Empiric i.v. antibiotics were started preoperatively with piperacillin/tazobactam (3 × 4/0.5 g/day). Urinary cultures revealed Escherichia coli, blood cultures were sterile. According to the bacterial resistogram, antibiotic treatment with piperacillin/tazobactam was continued. Initial PCT concentration was 48.9 ng/ml and decreased to 6.2 ng/ml within 5 days which is 80 % less compared to the initial peak value. Along with a substantial clinical improvement and complete resolution of organ dysfunction, antibiotic therapy was discontinued after 5 days. The patient was discharged from the intensive care unit on day 6 (Fig. 2).
Course of biomarkers, antibiotic treatment, and microbiological findings in a 75-year-old multimorbid female patient with septic shock due to urosepsis. The initial SOFA-Score was 13 and the SAPS II was 45. pip/tazo, piperacillin/tazobactam. SOFA Sequential Organ Failure Assessment Score. SAPS II Simplified Acute Physiology Score II. PCT procalcitonin (0–0.5 ng/ml). CRP C-reactive protein (< 0.5 mg/dl). WBC white blood cell count (3.5–9.8/nl).
Case 2
A 63-year-old male patient was admitted to hospital by his house practitioner with persisting urinary tract infection despite treatment with levofloxacin (500 mg/day) per os. On emergency room admission, the patient presented with signs of circulatory failure due to severe sepsis and had to be transferred to the intensive care unit. Due to pretreatment with fluorochinolones, the risk of infection with extended-spectrum beta-lactamases (ESBLs)-producing bacteria was high. PCT concentration was 196.0 ng/ml, and antibiotic treatment was empirically escalated to intravenous meropenen (1000 mg t. i. d.). While ureter stenting was performed under general anaesthesia, the patient’s vasopressors were required due to marked hypotension. Cardiocirculatory failure was responsive to continued fluid replacement and vasopressors, so that extubation was possible soon after re-transfer to the intensive care unit. Blood cultures revealed a cefuroxime-sensitive E. coli, and antibiotic treatment was de-escalated to intravenous cefuroxime (1500 mg t. i. d.). Repeated blood cultures on day 4 and 8, respectively, were negative, and antibiotic therapy was discontinued on day 10 after the patient was transferred to the regular ward on day 5 (Fig. 3).
Course of biomarkers, antibiotic treatment, and microbiological findings in a 63-year-old male patient with severe sepsis caused by ascending urinary tract infection and E. coli-bacteraemia. Initial SOFA-Score was 10 and SAPS II was 53. SOFA Sequential Organ Failure Assessment Score. SAPS II Simplified Acute Physiology Score II. PCT procalcitonin (0–0.5 ng/ml). CRP C-reactive protein (< 0.5 mg/dl). WBC white blood cell count (3.5–9.8/nl)
Case 3
A 43-year-old male patient was admitted to the intensive care unit with a clinical presentation of severe sepsis on the third postoperative day after laparoscopic adhaesiolysis due to adhaesions after open appendectomy 25 years ago. Hemodynamic stabilization was initiated, blood cultures were drawn, and empiric intravenous antibiosis with piperacillin/tazobactam (4000 mg/ 500 mg q. i. d.) was started. Emergency surgery with laparotomy revealed a small bowel lesion, intraoperative smears were taken, and a small bowel resection with anastomosis and intraoperative lavage was performed. Postoperatively, the patient returned intubated, ventilated, and analgosedated to the intensive care unit. Persistent cardocirculatory failure was treated with fluid replacement and vasopressors, mechanical ventilation had to be continued for respiratory failure. Intraabdominal smears grew Enterobacter cloacae, resistograms confirmed aedequate antibiotic treatment with piperacillin/tazobactam. Blood cultures remained sterile throughout the clinical course. Antibiotic treatment was discontinued on day 6 after clinical improvement and resolution of organ failure. Simultaneously, PCT concentrations decreased from 29.2 to 2.6 ng/ml. The patient was discharged from the intensive care unit on day 8 (Fig. 4).
Course of biomarkers, antibiotic treatment, and microbiological findings in a 43-year-old male patient with severe sepsis caused by peritonitis due to small bowel perforation. Initial SOFA-Score was 11 and SAPS II was 54. pip/tazo, piperacillin/tazobactam. SOFA Sequential Organ Failure Assessment Score. SAPS II Simplified Acute Physiology Score II. PCT procalcitonin (0–0.5 ng/ml). CRP C-reactive protein (< 0.5 mg/dl). WBC white blood cell count (3.5–9.8/nl)
Case 4
A 59-year-old male patient was readmitted to the surgical intensive care unit with signs of sepsis on postoperative day 6 after a pylorus-preserving duodenopancreatectomy due to a neuroendocrine tumour. So far, the patient had taken an uneventful course, he had been monitored at the intensive care unit for the first two postoperative days. An empiric antibiotic therapy with intravenous piperacillin/tazobactam (4000 mg/500 mg q. i. d.) was started. Prior to this, blood cultures were taken peripherally and from a central-venous line which revealed local signs of infection. In the absence of other possible infectious sources, a catheter-related sepsis was diagnosed. After blood cultures grew, Staphylococci species i. v. vancomycin (1000 mg b. i. d.) was added on day 3. After antibiograms and resistograms were available Staphylococcus aureus was identified and the antibiotic regimen was de-escalated to i.v. Flucloxacillin (6 × 2 g /day) on day 4. In the presence of a proven S. aureus sepsis, flucloxacillin treatment was intended for 14 days after a negative control blood culture. Aedequate clinical improvement and a PCT-decrease from 1.8 ng/ml on day 2 to 0.2 ng/ml on day 6 allowed a discharge from the intensive care unit to the regular ward on day 7 (Fig. 5).
Course of biomarkers, antibiotic treatment, and microbiological findings in a 59-year-old male patient with central venous catheter related sepsis. Initial SOFA-Score was 7 and SAPS II 25. pip/tazo, piperacillin/tazobactam. Vanco vancomycin. Fluc flucloxacillin. SOFA Sequential Organ Failure Assessment Score. SAPS II Simplified Acute Physiology Score II. PCT procalcitonin (0–0.5 ng/ml). CRP, C-reactive protein (< 0.5 mg/dl). WBC white blood cell count (3.5–9.8 /nl)
Case 5
A 76-year-old male was admitted to the emergency room with acute respiratory failure due to infectious chronic obstructive pulmonary disease (COPD) exacerbation and immediately transferred to the intensive care unit. After intubation, a bronchoscopy was performed, bronchoalveolar fluid samples were collected, and blood cultures were drawn. According to guideline recommendations, an intravenous antibiotic therapy with piperacillin/tazobactam (4000 mg/500 mg q. i. d.) and clarithromycin (500 mg b. i. d.) was immediately initiated. Concomitant septic shock required fluid replacement and vasopressors. Bronchoalveolar fluid samples grew Klebsiella pneumoniae, and antibiotic treatment was de-escalated to intravenous ampicillin/sulbactam (2000/1000 mg t. i. d.) on day 4 after clinical improvement. PCT concentrations decreased from 0.8 ng/ml on day 1 to 0.2 ng/ml on day 4. Along with complete resolution of organ failure and extubation, antibiotic treatment was discontinued on day 5. The patient was discharged from the intensive care unit on day 7 (Fig. 6).
Course of PCT, antibiotic treatment, and microbiological findings in a 76 year old patient with severe sepsis caused by infectious exacerbation of COPD. Initial SOFA-Score was 9 and SAPS II was 47 (not shown). pip/tazo, piperacillin/tazobactam. Amp/sulbact, ampicillin/sulbactam. Clari clarithromycin. SOFA Sequential Organ Failure Assessment Score. SAPS II Simplified Acute Physiology Score II. COPD chronic obstructive pulmonary disease. PCT procalcitonin (0–0.5 ng/ml). CRP C-reactive protein (< 0.5 mg/dl). WBC white blood cell count (3.5–9.8/nl)
Discussion
Severe systemic inflammatory response as well as severe non-septic diseases may lead to high PCT levels. Despite well-defined PCT cut-off levels, therapeutic decision-making requires assessment of clinical signs and symptoms. For clinically stable patients presenting to the emergency room with respiratory infections, PCT values <0.25 ng/ml could be shown to exclude severe bacterial infections. In these patients, decision making for or against antibiotic treatment can be safely made on the basis of a single PCT measurement [16]. In the intensive care setting, the situation is more complex. Antibiotic treatment is generally recommended at PCT cut-off levels >0.5 ng/ml; however, it has to be emphasised that infection must be suspected on the basis of both clinical signs and a potential septic focus. This is frequently a problem in the early postoperative period when PCT levels may be elevated in the absence of an infectious focus. The degree of PCT release usually correlates with the extent of the surgical procedure [17].
Kinetics of procalcitonin and limitations of clinical use
PCT can be detected in circulation within 2 to 6 h after an adequate infectious or inflammatory stimulus, and significant plasma concentrations are reached after about 6 h with peak levels after 12 to 48 h. Half-life of PCT is about 24 to 35 h, and daily measurements are sufficient to reflect the changes of plasma levels. Usually, a daily decrease of more than 30 % from the previous day’s value indicates a successful treatment in the ICU [18].
Not only infections but also other inflammatory conditions may trigger PCT, and several situations have been described where PCT can be elevated by non-bacterial causes. These include, but are not limited to the following:
-
the early period after a major trauma, major surgical intervention, severe burns, treatment with OKT3 antibodies, and other drugs stimulating the release of pro-inflammatory cytokines
-
patients with invasive fungal infections, acute attacks of plasmodium falciparum malaria
-
patients with prolonged or severe cardiogenic shock, prolonged severe organ perfusion anomalies, small-cell lung cancer, and medullary C-cell carcinoma of the thyroid [18].
Persistently, high or even increasing PCT levels indicate an ongoing inflammatory reaction and are often associated with an unfavourable clinical outcome [18].
Patients with renal insufficiency can have slightly elevated baseline PCT levels, and some authors suggest the use of an adjusted reference range from 0.5 to 1.5 ng/ml in patients with severe renal insufficiency [19, 20]. Furthermore, renal replacement therapy (RRT) can alter PCT concentrations by elimination from the plasma but on the contrary haemodialysis per se can lead to elevated PCT levels even in the outpatient setting [21]. In critically ill patients, PCT is removed from the plasma during continuous veno-venous haemofiltration (CVVH), but plasma PCT levels remain unchanged [22]. In summary, the situation in patients with renal failure with or without RRT appears to be complex, but the clinical relevance remains questionable [23]. Randomised controlled PCT trials included patients with acute or chronic renal failure and patients requiring RRT without adaption of cut-off levels [24].
PCT is not a specific marker for fungal diseases but elevated PCT levels can be found in severe fungal infections. Fungal infections should be considered in critically ill patients with persistently elevated or even increasing PCT levels despite of approriate source control and antibiotic treatment [18].
Equally, PCT is not a specific marker for viral infections. The strength of PCT in this context is to rule out bacterial causes in patients presenting with clinically mild to moderate acute respiratory infections in the emergency room or in the outpatient setting [25].
Severe infections may be associated with falsely low PCT concentrations, especially during the very early stages. Furthermore, in a critically ill patient with blood stream infections, PCT elevation and diagnosis accuracy could be lower if sepsis is secondary than in those with a first episode of infection [26].
As a consequence, necessary antibiotic treatment could be withheld if therapeutic decision-making is based on PCT values alone. It is therefore essential that decision-making for initiating antibiotic treatment in critically ill patients is always based on clinical criteria. If repeated PCT assessment reveals concentrations <0.5 ng/ml, severe bacterial infection can be excluded with high likelihood.
Clinical studies on PCT-guided treatment in the ICU
The length of antibiotic therapy in critically ill patients can be safely guided by PCT-guided protocols. Several reviews and meta-analyses demonstrated that implementation of PCT-guided algorithms led to a significant reduction of antibiotic exposure of 2 to 3.5 days [5–7, 25, 27, 28]. Shorter antibiotic treatment was safe and not associated with adverse effects on overall clinical outcome. Moreover, in some studies, even a reduced length of intensive care unit stay was reported [29, 30]. In a very recent large multi-center study in 1575 critically ill patients, median duration of antibiotic treatment was 5 days in the PCT group versus 7 days in the standard-of-care group. One-year mortality was significantly lower in the PCT group (36 %) than in the control group (43 %). The authors hypothesised that the adequacy of the antibiotics, a more timely recognition of alternative diagnoses and a lower toxicity of antibiotics might have contributed to a lower mortality in the PCT group [7].
Most of the high-quality studies in ICU patients which analysed the impact of PCT-guided therapy enrolled a large number (59–97 %) of medical patients [15, 31, 32], whereas only three studies included exclusively patients with a surgical diagnosis [30, 33, 34]. Two of these surgical studies reported on a shorter antibiotic treatment [30, 33], and one study even revealed a shorter ICU stay in the PCT group [30]. The study by Svoboda and colleagues focused more on PCT-triggered diagnostic procedures (computertomography, sonography) and surgical interventions [34].
In the intensive care setting, the strength of PCT is clearly to support decision-making for discontinuing antibiotic treatment. In the individual patient, the course of PCT concentrations over time is definitely more important than absolute values (especially in the postoperative period) as reliable indicator of successful treatment. It is therefore not surprising that studies using PCT cut-off values pro or contra escalating antibiotic regimen did not observe favourable effects on the use of antibiotics, but even reported increasing treatment rates and prolonged mechanical ventilation [15].
In septic patients, source control within the first 12 h should be achieved [1]. Inappropriate source control for example is an independent determinant of mortality in septic patients with intra-abominal infections [35]. However, both of the PCT studies in surgical ICU patients [30, 33] and two of the RCTs in a mixed ICU population [15, 31] did not exclusively exclude patients with inappropriate source control or the need for a long-term anti-infective treatment. The studies by Bouadma and Nobre in contrast excluded patients with a strong need for long-term antibiotics (i.e., infective endocarditis, osteoarticular infections, mediastinitis, hepatic or cerebral abscesses) and severely immunocompromised patients or patients on immunosuppressive therapy. Thus, for patients in which appropriate source control cannot be achieved, decisions on antibiotic treatment should rather be based on an individual approach. Biomarkers such as PCT can probably support deccision making even in these situations but further data are warranted to evaluate the role of PCT in septic patients with inappropriate source control.
Altough meta-analyses outline the potential of PCT in reducing the length of antibiotic treatment, there are several limitations in the prospective studies such as prolonged antibiotic treatment in the control groups as well as high drop-out rates due to non adherence to the PCT-algorithm in up to 50 % of patients which question the benefits of PCT-guided protocols for directing antibiotic treatment in the daily routine intensive care setting [29, 32, 36]. Unfortunately, robust clinical data on this topic are still scarce. Two publications in respiratory tract infections in the outpatient setting could show a sigificant reduction of antibiotic use if a PCT-guided algorithm was employed [37, 38]. In septic intensive care patients, a retrospective study demonstrated that implementation of a PCT-based algorithm was associated with a significantly shortened length of antibiotic treatment over a 5-year observation period [10]. As already well documented by prospective randomised studies, no negative effects on overall clinical outcome were observed despite the reduced antibiotic exposure.
Alternative biomarkers for guiding antibiotic treatment in the ICU
Despite of the widespread use of C-reactive protein (CRP), until recently, there were no prospectively tested cut-off values for guiding antibiotic treatment in the ICU. A recent Brazilian two-center RCT showed that a CRP-guided protocol was as effective as PCT-guided antibiotic treatment in 94 critically ill patients [39]. In this study, antibiotic treatment was discontinued in both groups by day 7 at the latest when infection had resolved regardless of biomarker levels. Median duration of antibiotic treatment was 7 (PCT), respectively, 6 days (CRP) and did not differ siginificantly in this study. By the restriction of antibiotic treatment to 7 days, the study impressively supports recommendations from guidelines that in a clinically recovering septic patient, 7 days of antibiotic treatment appears to be safe [1] rather than providing evidence that CRP-guided treament is as effective as PCT. Furthermore, the patient population in this study was not representative for a surgical ICU, as patients who suffered multiple trauma, burns, or major surgery in the previous 5 days were excluded.
In our clinical examples, the varying kinetics of CRP and white cell blood count (WBC), particularly in case 1,3, and 4, impressively show that decisions on discontinuation or de-escalation cannot be made based on these biomarkers (Figs. 2, 4, and 5). To our knowledge, no other biomarkers for guiding antibiotic treatment in critically ill septic patients have been evaluated in RCTs so far.
PCT in current guidelines
The favourable results of various prospective randomised studies have made PCT-guided protocols for antibiotic therapy integral part of different guideline recommendations such as the current international guideline for the treatment of sepsis [1]. Accordingly, the German 2013S3-guideline emphasises the role of PCT in hospitalised patients as a valid strategy to assure a rational use of antibiotics [40]. However, both the grade of recommendation and the evidence for the use of PCT in the current guidelines is still low; however, this is also true for several measures recommended in international sepsis guidelines.
Cut-off levels
It has, however, to be mentioned that in some of these studies, strikingly different PCT cut-off values ranging from <1.0 ng/ml over <0.5 ng/ml to even <0.25 ng/ml were used at which discontinuation of antibiotic treatment was recommended. In a French multicenter study, the cut-off level for discontinuing antibiotic treatment was different for surgical and medical patients. In surgical patients, the cut-off level was <4 ng/ml, whereas in medical patients considerably lower concentrations were suggested [31]. Antibiotic treatment should also be stopped, if PCT levels decline to a specific percentage of the peak value, even if the abovementioned absolute concentrations are not yet reached. These percentages were ranging from 70 to 90 % in most of the studies. The algorithm for PCT-guided antibiotic treatment used in our ICU is shown in Fig. 1.
The variable cut-off levels clearly demonstrate that no general guideline can ever meet the disease complexity of critically ill patients in intensive care units. Any biomarker needs to be interpreted in the clinical course and context. For example, if organ dysfunction such as neurologic disturbance or vasopressor support resolves and, thus, indicates clinical stabilisation along with a decrease of PCT concentrations below the abovementioned cut-off levels or PCT levels decrease to 10–20 % of the peak value, antibiotic treatment can be safely discontinued.
PCT in different septic conditions
Case 1 is a very good example for the application of a PCT-guided antibiotic treatment: in the multimorbid female patient with clinical signs of a severe urosepsis due to hydronephrosis focus control by ureter stenting, empiric antibiosis, and intensive care support of organ failure was performed. After 5 days of treatment and marked clinical improvement, antibiosis was discontinued at a PCT level of 6.2 ng/ml equaling a decrease of 80 % compared to the initial peak concentration. Case 2 suffered from urosepsis as well. In this patient, an E. coli sepsis was diagnosed and antibiotic treatment was continued for until day 10 despite clinical improvement and an aedequate PCT decrease. The two respective cases also demonstrate that patients with urosepsis caused by E. coli present with overall higher PCT concentrations than patient 3 with peritonitis and proven Enterobacter cloacae intraabdominally, patient 5 with pneumonia and proven Klebsiella pneumoniae in bronchoalveolar fluid or patient 4 with catheter related sepsis by S. aureus. Our clinical cases impressively show that the degree of systemic PCT release is highly dependent on the site of infection and the type of bacteria. In a critically ill patient with clinical sepsis, Gram-negative bacteraemia seems to be associated with higher PCT levels than Gram-positive bacteraemia [14]. Although the mechanism underlying different PCT production in response to different bacterial pathogens is not completely clear, it could possibly be explained by the different interactions of Gram-positive or Gram-negative bacteria with host’s cells and different pathogen-associated molecular patterns [41]. E. coli bacteraemia/sepsis usually triggers an extremely high, S. aureus bacteraemia/sepsis only a moderate rise of PCT levels.
PCT and antimicrobial stewardship
In patients with infections such as bacterial endocarditis, mediastinitis, cerebral abscess or osteomyelitis, S. aureus or E. coli bacteraemia/sepsis generally requires a prolonged antibiotic regimen and, thus, we disregarded our PCT-protocol in patient 5 with S. aureus-sepsis. In these patients, specific guideline recommendations for antibiotic therapy rather than PCT-guided algorithms should be considered. Thus, it is important to use PCT-protocols in conjunction with local antibiotic stewardship measures, such as regular clinical rounds together with infectious diseases specialists. Antimicrobial stewardship includes not only limiting inappropriate use but also optimising antimicrobial selection, dosing, route, and duration of therapy to maximise clinical cure or prevention of infection while limiting the unintended consequences, such as the emergence of resistance, adverse drug events, and cost [42].
Core strategies of hospital antimicrobial stewardship programmes (ASP) are [40] the following:
-
Application of local treatment guidelines/pathways, hospital antiinfective formulary, formulary restrictions and approval requirements
-
Design and implementation of education, training and information
-
Conducting proactive audits of antiinfective use
-
Quality indicators.
Retrospective data from a surgical ICU showed a marked reduction (−21.2 %) of antibiotic use density after implementation of a local antibiotic stewardship programm in conjunction with a PCT protocol [9].
Further effects of PCT-guided antibiotic treatment
Shortening antibiotic exposure may have additional positive effects such as a reduction of drug-related side effects, the development of fewer bacterial resistances or a lower incidence of Clostridium difficile infections. So far, the question as to what extent PCT-guided antibiotic protocols may contribute to these issues remains unanswered. In addition, cost effectiveness of PCT-driven antibiotic regimen is still a matter of debate. While some calculations have shown that the use of PCT is cost effective under specific circumstances [43, 44], most prospective randomised studies did not address this issue. For any valid cost-effectiveness calculation, it is not sufficient to compare cost savings due to shortened antibiotic treatment with increased expenses caused by PCT measurements alone. This would furthermore require to include possible savings in terms of treatment expenses for drug-related side effets or Clostridium difficile infections. In addition, a potential reduction of mutli-resistant bacteria could save both staff and logistic requirements and, thus, may further enhance the economic benefit. Calculation of cost-effectiveness is furthermore hampered by the fact that no uniform PCT algorithm exists for the use in the intensive care setting. As already mentioned, the available studies report extremely variable PCT cut-off values. On the other hand, the exact number of PCT measurements and the time intervals between has not been clarified yet. While some studies performed PCT measuremets daily, intervals of 2 to 3 days are usually the rule in routine clinical care which further adds to cost savings. Finally, it should be mentioned that different assays are available for PCT measurements: a regular immunoassay, a highly sensitive immunoassay and a semiquantitative bedside-test. For guided treatment protocols, it is important to use highly sensitive assays which have a functional assay sensitivity of <0.1 ng/ml, especially with regard to indications like respiratory tract infections. Semiquantitative tests or tests with a low sensitivity are not suitable for PCT-guided antibiotic treatment and have not been evaluated in high-quality clinical studies.
Conclusions
In summary, the indication for antibiotic treatment in intensive care medicine is a clinical decicion. PCT protocols are a helpful and safe guide without negative effects on overall clinical outcome to discontinue antibiotic therapy in the ICU. Herein, a decrease of PCT along with clinical improvement is more important than the absolute concentration or any defined cut-off value. According to the current literature, antibiotic treatment can be discontinued, if PCT drops below a range of <0.25 or <0.5 ng/ml or decreases to at least 20 % of its peak level in the course of the disease along with clinical improvement of the patient. Regarding the limitations of PCT and due to the complexity of infections in critically ill patients, such protocols should be implemented in antibiotic stewardship programmes.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39(2):165–228. doi:10.1007/s00134-012-2769-8
Pugh R, Grant C, Cooke RP, Dempsey G (2015) Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev 8:Cd007577. doi:10.1002/14651858.CD007577.pub3
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, Cook CH, O’Neill PJ, Mazuski JE, Askari R, Wilson MA, Napolitano LM, Namias N, Miller PR, Dellinger EP, Watson CM, Coimbra R, Dent DL, Lowry SF, Cocanour CS, West MA, Banton KL, Cheadle WG, Lipsett PA, Guidry CA, Popovsky K (2015) Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med 372(21):1996–2005. doi:10.1056/NEJMoa1411162
Rubinstein E (2007) Short antibiotic treatment courses or how short is short? Int J Antimicrob Agents 30(Suppl 1):S76–S79. doi:10.1016/j.ijantimicag.2007.06.017
Matthaiou DK, Ntani G, Kontogiorgi M, Poulakou G, Armaganidis A, Dimopoulos G (2012) An ESICM systematic review and meta-analysis of procalcitonin-guided antibiotic therapy algorithms in adult critically ill patients. Intensive Care Med 38(6):940–949. doi:10.1007/s00134-012-2563-7
Prkno A, Wacker C, Brunkhorst FM, Schlattmann P (2013) Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock—a systematic review and meta-analysis. Crit Care 17(6):R291. doi:10.1186/cc13157
de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, Loef BG, Dormans T, van Melsen GC, Kluiters YC, Kemperman H, van den Elsen MJ, Schouten JA, Streefkerk JO, Krabbe HG, Kieft H, Kluge GH, van Dam VC, van Pelt J, Bormans L, Otten MB, Reidinga AC, Endeman H, Twisk JW, van de Garde EM, de Smet AM, Kesecioglu J, Girbes AR, Nijsten MW, de Lange DW (2016) Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. doi:10.1016/s1473-3099(16)00053-0
Schuetz P, Raad I, Amin DN (2013) Using procalcitonin-guided algorithms to improve antimicrobial therapy in ICU patients with respiratory infections and sepsis. Curr Opin Crit Care 19(5):453–460. doi:10.1097/MCC.0b013e328363bd38
Hohn A, Heising B, Hertel S, Baumgarten G, Hochreiter M, Schroeder S (2015) Antibiotic consumption after implementation of a procalcitonin-guided antimicrobial stewardship programme in surgical patients admitted to an intensive care unit: a retrospective before-and-after analysis. Infection 43(4):405–412. doi:10.1007/s15010-014-0718-x
Hohn A, Schroeder S, Gehrt A, Bernhardt K, Bein B, Wegscheider K, Hochreiter M (2013) Procalcitonin-guided algorithm to reduce length of antibiotic therapy in patients with severe sepsis and septic shock. BMC Infect Dis 13:158. doi:10.1186/1471-2334-13-158
Meisner M, Adina H, Schmidt J (2006) Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the intensive care unit course of multiple-trauma patients. Crit Care 10(1):R1. doi:10.1186/cc3910
Meisner M, Rauschmayer C, Schmidt J, Feyrer R, Cesnjevar R, Bredle D, Tschaikowsky K (2002) Early increase of procalcitonin after cardiovascular surgery in patients with postoperative complications. Intensive Care Med 28(8):1094–1102. doi:10.1007/s00134-002-1392-5
Brodska H, Malickova K, Adamkova V, Benakova H, Stastna MM, Zima T (2013) Significantly higher procalcitonin levels could differentiate gram-negative sepsis from gram-positive and fungal sepsis. Clin Exp Med 13(3):165–170. doi:10.1007/s10238-012-0191-8
Charles PE, Ladoire S, Aho S, Quenot JP, Doise JM, Prin S, Olsson NO, Blettery B (2008) Serum procalcitonin elevation in critically ill patients at the onset of bacteremia caused by either gram negative or gram positive bacteria. BMC Infect Dis 8:38. doi:10.1186/1471-2334-8-38
Jensen JU, Hein L, Lundgren B, Bestle MH, Mohr TT, Andersen MH, Thornberg KJ, Loken J, Steensen M, Fox Z, Tousi H, Soe-Jensen P, Lauritsen AO, Strange D, Petersen PL, Reiter N, Hestad S, Thormar K, Fjeldborg P, Larsen KM, Drenck NE, Ostergaard C, Kjaer J, Grarup J, Lundgren JD (2011) Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomized trial. Crit Care Med 39(9):2048–2058. doi:10.1097/CCM.0b013e31821e8791
Schuetz P, Christ-Crain M, Thomann R, Falconnier C, Wolbers M, Widmer I, Neidert S, Fricker T, Blum C, Schild U, Regez K, Schoenenberger R, Henzen C, Bregenzer T, Hoess C, Krause M, Bucher HC, Zimmerli W, Mueller B (2009) Effect of procalcitonin-based guidelines vs standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. JAMA 302(10):1059–1066. doi:10.1001/jama.2009.1297
Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schuttler J (1998) Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med 24(7):680–684
Meisner M (2000) Procalcitonin (PCT)—a new, innovative infection parameter. Biochemical and clinical aspects. Thieme, Stuttgart
Amour J, Birenbaum A, Langeron O, Le Manach Y, Bertrand M, Coriat P, Riou B, Bernard M, Hausfater P (2008) Influence of renal dysfunction on the accuracy of procalcitonin for the diagnosis of postoperative infection after vascular surgery. Crit Care Med 36(4):1147–1154. doi:10.1097/CCM.0b013e3181692966
Sitter T, Schmidt M, Schneider S, Schiffl H (2002) Differential diagnosis of bacterial infection and inflammatory response in kidney diseases using procalcitonin. J Nephrol 15(3):297–301
Schmidt M, Burchardi C, Sitter T, Held E, Schiffl H (2000) Procalcitonin in patients undergoing chronic hemodialysis. Nephron 84(2):187–188
Meisner M, Huttemann E, Lohs T, Kasakov L, Reinhart K (2001) Plasma concentrations and clearance of procalcitonin during continuous veno-venous hemofiltration in septic patients. Shock 15(3):171–175
Kutz A, Grolimund E, Christ-Crain M, Thomann R, Falconnier C, Hoess C, Henzen C, Zimmerli W, Mueller B, Schuetz P (2014) Pre-analytic factors and initial biomarker levels in community-acquired pneumonia patients. BMC Anesthesiol 14:102. doi:10.1186/1471-2253-14-102
Albrich WC, Harbarth S (2015) Pros and cons of using biomarkers versus clinical decisions in start and stop decisions for antibiotics in the critical care setting. Intensive Care Med 41(10):1739–1751. doi:10.1007/s00134-015-3978-8
Schuetz P, Muller B, Christ-Crain M, Stolz D, Tamm M, Bouadma L, Luyt CE, Wolff M, Chastre J, Tubach F, Kristoffersen KB, Burkhardt O, Welte T, Schroeder S, Nobre V, Wei L, Bhatnagar N, Bucher HC, Briel M (2012) Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev 9:CD007498. doi:10.1002/14651858.CD007498.pub2
Charles PE, Ladoire S, Snauwaert A, Prin S, Aho S, Pechinot A, Olsson NO, Blettery B, Doise JM, Quenot JP (2008) Impact of previous sepsis on the accuracy of procalcitonin for the early diagnosis of blood stream infection in critically ill patients. BMC Infect Dis 8:163. doi:10.1186/1471-2334-8-163
Kopterides P, Siempos II, Tsangaris I, Tsantes A, Armaganidis A (2010) Procalcitonin-guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med 38(11):2229–2241. doi:10.1097/CCM.0b013e3181f17bf9
Tang H, Huang T, Jing J, Shen H, Cui W (2009) Effect of procalcitonin-guided treatment in patients with infections: a systematic review and meta-analysis. Infection 37(6):497–507. doi:10.1007/s15010-009-9034-2
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J (2008) Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 177(5):498–505. doi:10.1164/rccm.200708-1238OC
Hochreiter M, Kohler T, Schweiger AM, Keck FS, Bein B, von Spiegel T, Schroeder S (2009) Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Crit Care 13(3):R83. doi:10.1186/cc7903
Annane D, Maxime V, Faller JP, Mezher C, Clec’h C, Martel P, Gonzales H, Feissel M, Cohen Y, Capellier G, Gharbi M, Nardi O (2013) Procalcitonin levels to guide antibiotic therapy in adults with non-microbiologically proven apparent severe sepsis: a randomised controlled trial. BMJ Open 3(2). doi:10.1136/bmjopen-2012-002186
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M, Bernard M, Pasquet B, Regnier B, Brun-Buisson C, Chastre J, Wolff M (2010) Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 375(9713):463–474. doi:10.1016/S0140-6736(09)61879-1
Schroeder S, Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, von Spiegel T (2009) Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: results of a prospective randomized study. Langenbeck’s Arch Surg 394(2):221–226. doi:10.1007/s00423-008-0432-1
Svoboda P, Kantorova I, Scheer P, Radvanova J, Radvan M (2007) Can procalcitonin help us in timing of re-intervention in septic patients after multiple trauma or major surgery? Hepato-Gastroenterology 54(74):359–363
Tellor B, Skrupky LP, Symons W, High E, Micek ST, Mazuski JE (2015) Inadequate source control and inappropriate antibiotics are key determinants of mortality in patients with intra-abdominal sepsis and associated bacteremia. Surg Infect 16(6):785–793. doi:10.1089/sur.2014.166
Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, Marsch S, Azzola A, Rakic J, Mueller B, Tamm M (2009) Procalcitonin for reduced antibiotic exposure in ventilator-associated pneumonia: a randomised study. Eur Respir J 34(6):1364–1375. doi:10.1183/09031936.00053209
Albrich WC, Dusemund F, Bucher B, Meyer S, Thomann R, Kuhn F, Bassetti S, Sprenger M, Bachli E, Sigrist T, Schwietert M, Amin D, Hausfater P, Carre E, Gaillat J, Schuetz P, Regez K, Bossart R, Schild U, Mueller B, Proreal Study Team FT (2012) Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in “real life”: an international, multicenter poststudy survey (ProREAL). Arch Intern Med 172(9):715–722. doi:10.1001/archinternmed.2012.770
Schuetz P, Batschwaroff M, Dusemund F, Albrich W, Burgi U, Maurer M, Brutsche M, Huber AR, Muller B (2010) Effectiveness of a procalcitonin algorithm to guide antibiotic therapy in respiratory tract infections outside of study conditions: a post-study survey. Eur J Clin Microbiol Infect Dis 29(3):269–277. doi:10.1007/s10096-009-0851-0
Oliveira CF, Botoni FA, Oliveira CR, Silva CB, Pereira HA, Serufo JC, Nobre V (2013) Procalcitonin versus C-reactive protein for guiding antibiotic therapy in sepsis: a randomized trial. Crit Care Med 41(10):2336–2343. doi:10.1097/CCM.0b013e31828e969f
de With K, Allerberger F, Amann S, Apfalter P, Brodt HR, Eckmanns T, Fellhauer M, Geiss HK, Janata O, Krause R, Lemmen S, Meyer E, Mittermayer H, Porsche U, Presterl E, Reuter S, Sinha B, Strauss R, Wechsler-Fordos A, Wenisch C, Kern WV (2016) Strategies to enhance rational use of antibiotics in hospital: a guideline by the German Society for Infectious Diseases. Infection. doi:10.1007/s15010-016-0885-z
Leli C, Ferranti M, Moretti A, Al Dhahab ZS, Cenci E, Mencacci A (2015) Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections. Dis Markers 2015:701480. doi:10.1155/2015/701480
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44(2):159–177. doi:10.1086/510393
Heyland DK, Johnson AP, Reynolds SC, Muscedere J (2011) Procalcitonin for reduced antibiotic exposure in the critical care setting: a systematic review and an economic evaluation. Crit Care Med 39(7):1792–1799. doi:10.1097/CCM.0b013e31821201a5
Wilke MH, Grube RF, Bodmann KF (2011) The use of a standardized PCT-algorithm reduces costs in intensive care in septic patients - a DRG-based simulation model. Eur J Med Res 16(12):543–548
Authors’ contributions
AH, BH, and SS contributed to the study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript and the critical revision of manuscript.
JKS and OS contributed to the acquisition of data, analysis and interpretation of data, and the critical revision of manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study received no particular funding.
This retrospective study based on chart review was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Ethics approval was waived by the local ethics committee of the Landesärztekammer Nordrhein (LÄK Nordrhein 240–2015) due to retrospective and anonymous nature of the analysis and an informed consent was not required.
Sources of financial support
None.
Conflict of interest
SS served as consultant and has received payments from BRAHMS AG for speaking engagements. All other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hohn, A., Heising, B., Schütte, JK. et al. Procalcitonin-guided antibiotic treatment in critically ill patients. Langenbecks Arch Surg 402, 1–13 (2017). https://doi.org/10.1007/s00423-016-1458-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1458-4