Abstract
Objective:
The aim of this study was to review the effectiveness of procalcitonin (PCT)-guided therapy in comparison to standard therapy in patients with suspected or confirmed bacterial infections in terms of antibiotic prescription at inclusion, duration of antibiotic therapy, total antibiotic exposure days/1,000 days, length of stay in the intensive care unit (ICU), length of stay in the hospital, and mortality.
Methods:
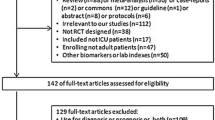
MEDLINE, EMBASE, Web of Science, and the Cochrane central register of controlled trials were searched up to November 2008. Studies considered to be eligible were randomized controlled trials comparing PCT-guided therapy with standard therapy in adult patients with bacterial infections. No language restriction was applied. Data were combined in a meta-analysis using random-effect models.
Results:
Seven studies with 1,458 patients were included. PCT-guided therapy was associated with a significant reduction in antibiotic prescription at inclusion (four studies; pooled odds ratio [OR] 0.506, 95% confidence interval [CI] 0.290–0.882, p = 0.016), duration of antibiotic therapy (six studies; weighted mean difference [WMD] 2.785, 95% CI 1.225–4.345, p = 0.000), total antibiotic exposure days/1,000 days (four studies; pooled relative risk [RR] 1.664, 95% CI 1.155–2.172, p = 0.000), and length of stay in the ICU (three studies; 292 patients; pooled WMD 3.49 days, 95% CI 1.28–5.70, p = 0.002). There were no significant differences in length of stay in the hospital (three studies; pooled WMD 1.003, 95% CI –0.430 to 2.437, p = 0.17) and mortality (seven studies; pooled OR 0.838, 95% CI 0.571–1.229, p = 0.365).
Conclusions:
Based on the results of this meta-analysis, it would appear that an algorithm based on serial PCT measurements would allow a more judicious use of antibiotics than currently occurs during the traditional treatment of patients with infections. PCT-guided antibiotic treatment appears to be safe and may also improve clinical outcome.
Similar content being viewed by others
References
Evans HL, Lefrak SN, Lyman J, Smith RL, Chong TW, McElearney ST, Schulman AR, Hughes MG, Raymond DP, Pruett TL, Sawyer RG: Cost of gram-negative resistance. Crit Care Med 2007; 35: 89–95.
Gonzales R, Steiner JF, Lum A, Barrett PH Jr: Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA 1999; 281: 1512–1519.
Guillemot D, Courvalin P: Better control of antibiotic resistance. Clin Infect Dis 2001; 33: 542–547.
Harbarth S, Nobre V, Pittet D: Does antibiotic selection impact patient outcome? Clin Infect Dis 2007; 44: 87–93.
El Moussaoui R, Roede BM, Speelman P, Bresser P, Prins JM, Bossuyt PM: Short-course antibiotic treatment in acute exacerbations of chronic bronchitis and COPD: a meta-analysis of double-blind studies. Thorax 2008; 63: 415–422.
File TM Jr, Mandell LA: What is optimal antimicrobial therapy for bacteremic pneumococcal pneumonia? Clin Infect Dis 2003; 36: 396–398.
Tillotson GS, Doern GV, Blondeau JM: Optimal antimicrobial therapy: the balance of potency and exposure. Expert Opin Investig Drugs 2006; 15: 335–337.
Fish DN: Optimal antimicrobial therapy for sepsis. Am J Health Syst Pharm 2002; 59(Suppl 1): S13–S19.
Christ-Crain M, Muller B: Biomarkers in respiratory tract infections: diagnostic guides to antibiotic prescription, prognostic markers and mediators. Eur Respir J 2007; 30: 556–573.
Oczenski W, Fitzgerald RD, Schwarz S: Procalcitonin: a new parameter for the diagnosis of bacterial infection in the perioperative period. Eur J Anaesthesiol 1998; 15: 202–209.
Muller B, Becker KL: Procalcitonin: how a hormone became a marker and mediator of sepsis. Swiss Med Wkly 2001; 131: 595–602.
Muller B, Becker KL, Kranzlin M, Schachinger H, Huber PR, Nylen ES, Snider RH, White JC, Schmidt-Gayk H, Zimmerli W, Ritz R: Disordered calcium homeostasis of sepsis: association with calcitonin precursors. Eur J Clin Invest 2000; 30: 823–831.
Yang CH, Lu DCT: Clinical applications of procalcitonin (ProCT). J Intern Med Taiwan 2006; 17: 1–10.
Chirouze C, Schuhmacher H, Rabaud C, Gil H, Khayat N, Estavoyer JM, May T, Hoen B: Low serum procalcitonin level accurately predicts the absence of bacteremia in adult patients with acute fever. Clin Infect Dis 2002; 35: 156–161.
Ebell M: Procalcitonin-guided treatment of respiratory tract infections. Am Fam Physician 2008; 78: 756–757.
Martinez FJ, Curtis JL: Procalcitonin-guided antibiotic therapy in COPD exacerbations: closer but not quite there. Chest 2007; 131: 1–2.
Shehabi Y, Seppelt I: Pro/Con debate: is procalcitonin useful for guiding antibiotic decision making in critically ill patients? Crit Care 2008; 12: 211.
Higgins JPT, Altman DG: Assessing risk of bias in included studies. In: Higgins JPT, Green S (eds): Ochrane handbook for systematic reviews of interventions 5.0.0. Wiley: London 2008.
Wen J, Ren Y, Wang L, Li Y, Liu Y, Zhou M, Liu P, Ye L, Tian W: The reporting quality of meta-analyses improves: a random sampling study. J Clin Epidemiol 2008; 61: 770–775.
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF: Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999; 354: 1896–1900.
DerSimonian R: Combining evidence from clinical trials. Anesth Analg 1990; 70: 475–476.
Higgins JP, Thompson SG: Quantifying heterogeneity in a metaanalysis. Stat Med 2002; 21: 1539–1558.
Egger M, Davey Smith G, Schneider M, Minder C: Bias in metaanalysis detected by a simple, graphical test. Br Med J 1997; 315: 629–634.
Soeken KL, Sripusanapan A: Assessing publication bias in metaanalysis. Nurs Res 2003; 52: 57–60.
Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, Muller B: Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet 2004; 363: 600–607.
Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR, Zimmerli W, Harbarth S, Tamm M, Muller B: Procalcitonin guidance of antibiotic therapy in communityacquired pneumonia: a randomized trial. Am J Respir Crit Care Med 2006; 174: 84–93.
Stolz D, Christ-Grain M, Bingisser R, Leuppi J, Miedinger D, Muller C, Huber P, Muller B, Tamm M: Antibiotic treatment of exacerbations of COPD: a randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007; 131: 9–19.
Svoboda P, Kantorova I, Scheer P, Radvanova J, Radvan M: Can procalcitonin help us in timing of re-intervention in septic patients after multiple trauma or major surgery? Hepato-gastroenterology 2007; 54: 359–363.
Briel M, Schuetz P, Mueller B, Young J, Schild U, Nusbaumer C, Periat P, Bucher HC, Christ-Crain M: Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med 2008; 168: 2000–2007, discussion 2007–2008.
Hochreiter M, Kohler T, Schweiger A-M, Keck FS, Bein B, Von Spiegel T, Schroder S: Antibiotic treatment of surgical intensive care patients. Procalcitonin to guide duration of therapy. Anaesthesist 2008; 57: 571–577.
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J: Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 2008; 177: 498–505.
Reinhart K, Meisner M, Brunkhorst FM: Markers for sepsis diagnosis: what is useful? Crit Care Clin 2006; 22: 503–519, ix–x.
Harbarth S: The effect of antimicrobial use on emergence and selection of resistance. Anasthesiol Intensivmed Notfallmed Schmerzther 2007; 42: 130–135.
Carbon C, Bax RP: Regulating the use of antibiotics in the community. Br Med J 1998; 317: 663–665.
Guillemot D, Maison P, Carbon C, Balkau B, Vauzelle-Kervroedan F, Sermet C, Bouvenot G, Eschwege E: Trends in antimicrobial drug use in the community-France, 1981–1992. J Infect Dis 1998; 177: 492–497.
Tang BM, Eslick GD, Craig JC, McLean AS: Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis 2007; 7: 210–217.
Jones AE, Fiechtl JF, Brown MD, Ballew JJ, Kline JA: Procalcitonin test in the diagnosis of bacteremia: a meta-analysis. Ann Emerg Med 2007; 50: 34–41.
Nylen E, Muller B, Becker KL, Snider R: The future diagnostic role of procalcitonin levels: the need for improved sensitivity. Clin Infect Dis 2003; 36: 823–824, author reply 826–827.
Becker KL, Snider R, Nylen ES: Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med 2008; 36: 941–952.
Schneider HG, Lam QT: Procalcitonin for the clinical laboratory: a review. Pathology 2007; 39: 383–390.
Christ-Crain M, Schuetz P, Huber AR, Muller B: Procalcitonin — importance for the diagnosis of bacterial infections. Ther Umsch 2008; 65: 559–568.
Meisner M: Pathobiochemistry and clinical use of procalcitonin. Clin Chim Acta 2002; 323: 17–29.
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Tang and T. Huang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tang, H., Huang, T., Jing, J. et al. Effect of Procalcitonin-Guided Treatment in Patients with Infections: a Systematic Review and Meta-Analysis. Infection 37, 497–507 (2009). https://doi.org/10.1007/s15010-009-9034-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-009-9034-2