Abstract
Purpose
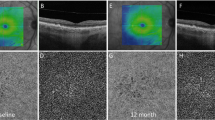
To evaluate the relationship between choriocapillaris (CC), flow deficits (FD), and structural optical coherence tomography (OCT) biomarkers, and the progression of intermediate age-related macular degeneration (iAMD) to complete retinal pigment epithelial and outer retinal atrophy (cRORA) or macular neovascularization (MNV).
Methods
Consecutive patients with iAMD were sequentially reviewed to define three equal sized groups: progressed to MNV, progressed to cRORA, or remained stable over 12 months of follow-up. Odds ratios for progression to cRORA and MNV were estimated by logistic regression for intraretinal hyperreflective foci (IHRF), hyporeflective drusen cores (hDC), subretinal drusenoid deposits (SDDs), high central drusen volume, fellow eye with late AMD, and peripheral and central CC FD.
Results
Thirty iAMD eyes from 30 patients were enrolled into each group. The CC FD was greater in the peripheral sectors of the macula of eyes which progressed to cRORA compared to the other two groups (P < 0.0001). The central CC FD was also significantly impaired in eyes that progressed to cRORA or MNV compared to eyes that did not progress (P = 0.001 and P = 0.02, respectively). CC FD in the peripheral macula was significantly and independently associated with the development of cRORA, while CC FD in the center was significantly and independently associated with the development of MNV.
Conclusions
While the CC is diffusely impaired throughout the macula in iAMD eyes that progress to cRORA, it is relatively spared in the more peripheral macula among eyes which progress to MNV. These differential findings may have implications for the pathophysiology of the different late-stage manifestations of AMD.



Similar content being viewed by others
Data availability
All data relevant to the study are included in the article or uploaded as supplementary information.
References
Schmitz-Valckenberg S, Steinberg JS, Fleckenstein M, Visvalingam S, Brinkmann CK, Holz FG (2010) Combined confocal scanning laser ophthalmoscopy and spectral-domain optical coherence tomography imaging of reticular drusen associated with age-related macular degeneration. Ophthalmology 117:1169–1176
Bressler SB, Maguire MG, Bressler NM, Fine SL (1990) Relationship of drusen and abnormalities of the retinal pigment epithelium to the prognosis of neovascular macular degeneration. The Macular Photocoagulation Study Group. Arch Ophthalmol 108:1442–1447
Ferris FL, Davis MD, Clemons TE et al (2005) A simplified severity scale for age-related macular degeneration: AREDS Report No.18. Arch Ophthalmol 123:1570–1574
Klein R, Klein BEK, Knudtson MD, Meuer SM, Swift M, Gangnon RE (2007) Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology 114:253–262
Abdelfattah NS, Zhang H, Boyer DS et al (2016) Drusen volume as a predictor of disease progression in patients with late age-related macular degeneration in the fellow eye. Invest Ophthalmol Vis Sci 57:1839–1846
Finger RP, Chong E, McGuinness MB et al (2016) Reticular pseudodrusen and their association with age-related macular degeneration: the Melbourne Collaborative Cohort Study. Ophthalmology 123:599–608
Spaide RF, Ooto S (2018) Curcio CA (2018) Subretinal drusenoid deposits AKA pseudodrusen. Surv Ophthalmol 63:782–815
Lei J, Balasubramanian S, Abdelfattah NS, Nittala MG, Sadda SR (2017) Proposal of a simple optical coherence tomography-based scoring system for progression of age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 255:1551–1558
Nassisi M, Lei J, Abdelfattah NS et al (2019) OCT risk factors for development of late age-related macular degeneration in the fellow eyes of patients enrolled in the HARBOR Study. Ophthalmology 126:1667–1674
Chirco KR, Sohn EH, Stone EM, Tucker BA, Mullins RF (2017) Structural and molecular changes in the aging choroid: implications for age-related macular degeneration. Eye (Lond) 31:10–25
Querques G, Querques L, Forte R, Massamba N, Coscas F, Souied EH (2012) Choroidal changes associated with reticular pseudodrusen. Invest Ophthalmol Vis Sci 53:1258–1263
Corvi F, Souied EH, Capuano V et al (2017) Choroidal structure in eyes with drusen and reticular pseudodrusen determined by binarisation of optical coherence tomographic images. Br J Ophthalmol 101:348–352
Corvi F, Su L, Sadda SR (2021) Evaluation of the inner choroid using OCT angiography. Eye (Lond) 35:110–120
Nasir MA, Sugino I, Zarbin MA (1997) Decreased choriocapillaris perfusion following surgical excision of choroidal neovascular membranes in age-related macular degeneration. Br J Ophthalmol 81:481–489
Thulliez M, Zhang Q, Shi Y et al (2019) Correlations between choriocapillaris flow deficits around geographic atrophy and enlargement rates based on swept-source OCT imaging. Ophthalmol Retina 3:478–488
Alagorie AR, Verma A, Nassisi M, Sadda SR (2019) Quantitative assessment of choriocapillaris flow deficits in eyes with advanced age-related macular degeneration versus healthy eyes. Am J Ophthalmol 205:132–139
Corradetti G, Tiosano L, Nassisi M et al (2020) Scotopic microperimetric sensitivity and inner choroid flow deficits as predictors of progression to nascent geographic atrophy. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-316893
Corvi F, Tiosano L, Corradetti G et al (2020) Choriocapillaris flow deficit as a risk factor for progression of age-related macular degeneration. Retina. https://doi.org/10.1097/IAE.0000000000002990
Moult EM, Alibhai AY, Rebhun C et al (2020) Spatial distribution of choriocapillaris impairment in eyes with choroidal neovascularization secondary to age-related macular degeneration: a Quantitative OCT Angiography Study. Retina 40:428–445
Alagorie AR, Verma A, Nassisi M et al (2020) Quantitative assessment of choriocapillaris flow deficits surrounding choroidal neovascular membranes. Retina. https://doi.org/10.1097/IAE.0000000000002878
Alagorie AR, Nassisi M, Verma A et al (2020) Relationship between proximity of choriocapillaris flow deficits and enlargement rate of geographic atrophy. Graefes Arch Clin Exp Ophthalmol 258:995–1003
Moult EM, Alibhai AY, Lee B et al (2020) A framework for multiscale quantitation of relationships between choriocapillaris flow impairment and geographic atrophy growth. Am J Ophthalmol 214:172–187
Ferris FL, Wilkinson CP, Bird A et al (2013) Clinical classification of age-related macular degeneration. Ophthalmology 120:844–851
Sadda SR, Guymer R, Holz FG et al (2018) Consensus definition for atrophy associated with age-related macular degeneration on OCT: classification of atrophy report 3. Ophthalmology 125:537–548
Spaide RF, Jaffe GJ, Sarraf D et al (2020) Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology 127:616–636
Ho J, Witkin AJ, Liu J et al (2011) Documentation of intraretinal retinal pigment epithelium migration via high-speed ultrahigh-resolution optical coherence tomography. Ophthalmology 118:687–693
Lee SY, Stetson PF, Ruiz-Garcia H, Heussen FM, Sadda SR (2012) Automated characterization of pigment epithelial detachment by optical coherence tomography. Invest Ophthalmol Vis Sci 53:164–170
Gregori G, Wang F, Rosenfeld PJ et al (2011) Spectral domain optical coherence tomography imaging of drusen in nonexudative age-related macular degeneration. Ophthalmology 118:1373–1379
Byon I, Alagorie AR, Ji Y, Su L, Sadda SR (2020) Optimizing the repeatability of choriocapillaris flow deficit measurement from optical coherence tomography angiography. Am J Ophthalmol 219:21–32
Lane M, Moult EM, Novais EA et al (2016) Visualizing the choriocapillaris under drusen: comparing 1050-nm swept-source versus 840-nm spectral-domain optical coherence tomography angiography. Invest Ophthalmol Vis Sci 57:OCT585–OCT590
Chu Z, Cheng Y, Zhang Q et al (2020) Quantification of choriocapillaris with Phansalkar local thresholding: pitfalls to avoid. Am J Ophthalmol 213:161–176
Zhang Q, Shi Y, Zhou H et al (2018) Accurate estimation of choriocapillaris flow deficits beyond normal intercapillary spacing with swept source OCT angiography. Quant Imaging Med Surg 8:658–666
Choi W, Moult EM, Waheed NK et al (2015) Ultrahigh-speed, swept-source optical coherence tomography angiography in nonexudative age-related macular degeneration with geographic atrophy. Ophthalmology 122:2532–2544
Moult EM, Waheed NK, Novais EA et al (2016) Swept-source optical coherence tomography angiography reveals choriocapillaris alterations in eyes with nascent geographic atrophy and drusen-associated geographic atrophy. Retina Suppl 1:S2–S11
Nattagh K, Zhou H, Rinella N et al (2020) OCT angiography to predict geographic atrophy progression using choriocapillaris flow void as a biomarker. Transl Vis Sci Technol 9:6
Christenbury JG, Folgar FA, O’Connell RV, Chiu SJ, Farsiu S, Toth CA (2013) Progression of intermediate age-related macular degeneration with proliferation and inner retinal migration of hyperreflective foci. Ophthalmology 120:1038–1045
Schmidt-Erfurth U, Waldstein SM, Klimscha S et al (2018) Prediction of individual disease conversion in early AMD using artificial intelligence. Invest Ophthalmol Vis Sci 59:3199–3208
Veerappan M, El-Hage-Sleiman A-KM, Tai V et al (2016) Optical coherence tomography reflective drusen substructures predict progression to geographic atrophy in age-related macular degeneration. Ophthalmology 123:2554–2570
Ouyang Y, Heussen FM, Hariri A, Keane PA, Sadda SR (2013) Optical coherence tomography-based observation of the natural history of drusenoid lesion in eyes with dry age-related macular degeneration. Ophthalmology 120:2656–2665
Corvi F, Cozzi M, Invernizzi A, Pace L, Sadda SR, Staurenghi G (2020) Optical coherence tomography angiography for detection of macular neovascularization associated with atrophy in age-related macular degeneration. Graefe’s Arch Clin Exp. https://doi.org/10.1007/s00417-020-04821-6
Faridi A, Jia Y, Gao SS et al (2017) Sensitivity and specificity of OCT angiography to detect choroidal neovascularization. Ophthalmol Retina 1:294–303
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FC: study conception, design, analysis, data acquisition, interpretation of data, drafting and revising, final approval. GC, LT, JAM, and TKL: data acquisition and data analysis, revising, and final approval. SRS: study conception, design, interpretation of data, drafting and revising, final approval.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
F. Corvi, G. Corradetti, L. Tiosano, J.A. McLaughlin, T.K. Lee declare no conflict of interest. S.R. Sadda reports consulting fees from Amgen, Allergan, Regeneron, Roche/Genentech, Novartis, Merck, 4DMT, Optos, Heidelberg, and Centervue. He also receives research instruments from Topcon, Nidek, Heidelberg, Centervue, Optos, and Carl Zeiss Meditec, outside the submitted work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplemental Figure 1.
Scatter plot showing the duration of the follow-up visit (in months) on the y-axis and the individual subject on x-axis for each group: intermediate age-related macular degeneration (iAMD) patients who remained stable over follow-up (black dot), iAMD who progressed to MNV (white square), and iAMD who progressed to cRORA (white dot) (PNG 7661 kb)
Rights and permissions
About this article
Cite this article
Corvi, F., Corradetti, G., Tiosano, L. et al. Topography of choriocapillaris flow deficit predicts development of neovascularization or atrophy in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 259, 2887–2895 (2021). https://doi.org/10.1007/s00417-021-05167-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05167-3