Abstract
Purpose
Conventional imaging techniques are not sensitive enough to reveal detailed structures of lacrimal drainage system (LDS) and its surrounding tissue (ST). Our study aimed to explore utility of ultrasound biomicroscopy (UBM) in assessment of small masses at the medial canthal region and compare performance of UBM with conventional imaging techniques.
Methods
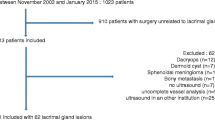
We prospectively recruited cases with small mass (long axis < 1 cm) at the medial canthal region (upper LDS-located area) from June 2017 to October 2018. UBM ± color Doppler flow imaging (CDFI) and conventional imaging techniques (computed tomography, magnetic resonance imaging, and dacryocystography) were conducted by four independent practitioners. Results were analyzed against gold standards with Cohen’s kappa test in three aspects including LDS patency, mass location, and presumptive diagnosis. Corresponding gold standards were syringe and dacryocystography, intraoperative findings, and pathological/empirical diagnosis.
Results
Seventy-two cases were recruited, including 20 cases of LDS lesions and 52 cases of ST lesions. Female (odds ratio 7.14) and age ≥ 37 (odds ratio 9.80) were risk factors for LDS lesion, and age range of 15–25 (odds ratio 9.17) was a risk factor for inflammatory ST lesion. In terms of LDS patency, UBM results were reliable for the detection of pre-saccal obstruction (kappa = 0.920), but were not reliable for intra-saccal and post-saccal obstruction (kappa = 0.106). In terms of mass location, the UBM (kappa = 0.766) performed better than conventional techniques (except for dacryocystography) to sort out ST lesions, with sensitivity of 93.8% and specificity of 83.3%. In terms of diagnosis, the UBM (kappa = 0.882) outweighed conventional techniques (except for magnetic resonance imaging) to distinguish cysts from nodules, with sensitivity of 93.8% and specificity of 94.4%. Notably, the UBM + CDFI achieved better performance than the UBM when screen out inflammatory lesions (kappa = 0.926 vs kappa = 0.689) and LDS-adjacent lesions (kappa = 0.815 vs kappa = 0.673), resulting in sensitivity of 91.7% and specificity of 100% for both testing items. If deep lesions (at the lacrimal sac–harbored area) were excluded, UBM reliability to detect inflammatory lesions (kappa = 0.915) and LDS-adjacent lesions (kappa = 0.770) improved, achieving sensitivity of 90.0% and 88.9%, and specificity of 100.0% and 92.7%, respectively.
Conclusions
The UBM is a valuable tool to assess superficial masses at the medial canthal region regarding pre-saccal obstruction, mass location, and presumptive diagnosis.
Trial registration
This work was registered on Chinese Clinical Trial Registry website with registration number ChiCTR1800018956.





Similar content being viewed by others
References
Santamaria JA, Gallagher CF, Mehta A, Davies BW (2018) Fibrous histiocytoma of the lacrimal sac in an 11-year-old male. Ophthalmic Plast Reconstr Surg 34:e90–e91
Sabundayo MS, Takahashi Y, Kakizaki H (2018) Lacrimal sac lymphoma: a series of Japanese patients. Eur J Ophthalmol. https://doi.org/10.1177/1120672118803510
Kim NJ, Choung HK, Khwarg SI (2009) Management of dermoid tumor in the medial canthal area. Korean J Ophthalmol 23:204–206
Obi EE, Olurin O, Mota PM, Sipkova Z, Vonica O, Pearson AR (2018) Assessment of lacrimal resistance using a manometric tear duct irrigation system. Orbit 37:273–279
Enright NJ, Brown SJ, Rouse HC, McNab AA, Hardy TG (2018) Nasolacrimal sac diverticulum: a case series and literature review. Ophthalmic Plast Reconstr Surg. https://doi.org/10.1097/IOP.0000000000001156
Kumar VA, Esmaeli B, Ahmed S, Gogia B, Debnam JM, Ginsberg LE (2016) Imaging features of malignant lacrimal sac and nasolacrimal duct tumors. AJNR Am J Neuroradiol 37:2134–2137
Nagi KS, Meyer DR (2010) Utilization patterns for diagnostic imaging in the evaluation of epiphora due to lacrimal obstruction: a National Survey. Ophthalmic Plast Reconstr Surg 26:168–171
Yuan MK, Tsai DC, Chang SC, Yuan MC, Chang SJ, Chen HW, Leu HB (2013) The risk of cataract associated with repeated head and neck CT studies: a nationwide population-based study. AJR Am J Roentgenol 201:626–630
Chen JX, Kachniarz B, Gilani S, Shin JJ (2014) Risk of malignancy associated with head and neck CT in children: a systematic review. Otolaryngol Head Neck Surg 151:554–566
Stupp T, Pavlidis M, Busse H, Thanos S (2004) Presurgical and postsurgical ultrasound assessment of lacrimal drainage dysfunction. Am J Ophthalmol 138:764–771
Zaidman CM, Seelig MJ, Baker JC, Mackinnon SE, Pestronk A (2013) Detection of peripheral nerve pathology: comparison of ultrasound and MRI. Neurology 80:1634–1640
Al-Faky YH (2011) Anatomical utility of ultrasound biomicroscopy in the lacrimal drainage system. Br J Ophthalmol 95:1446–1450
Mishra K, Hu KY, Kamal S, Andron A, Della Rocca RC, Ali MJ, Nair AG (2017) Dacryolithiasis: a review. Ophthalmic Plast Reconstr Surg 33:83–89
Tao H, Xu LP, Han C, Wang P, Bai F (2014) Diagnosis of lacrimal canalicular diseases using ultrasound biomicroscopy: a preliminary study. Int J Ophthalmol 7:659–662
Pavlidis M, Stupp T, Grenzebach U, Busse H, Thanos S (2005) Ultrasonic visualization of the effect of blinking on the lacrimal pump mechanism. Graefes Arch Clin Exp Ophthalmol 243:228–234
Maliborski A, Różycki R (2014) Diagnostic imaging of the nasolacrimal drainage system. Part I. Radiological anatomy of lacrimal pathways. Physiology of tear secretion and tear outflow. Med Sci Monit 20:628–638
Lachmund U, Ammann-Rauch D, Forrer A, Petralli C, Remonda L, Roeren T, Vonmoos F, Wilhelm K (2005) Balloon catheter dilatation of common canaliculus stenoses. Orbit 24:177–183
Vonica OA, Obi E, Sipkova Z, Soare C, Pearson AR (2017) The value of lacrimal scintillography in the assessment of patients with epiphora. Eye 31:1020–1026
Coskun B, Ilgit E, Onal B, Konuk O, Erbas G (2012) MR dacryocystography in the evaluation of patients with obstructive epiphora treated by means of interventional radiologic procedures. AJNR Am J Neuroradiol 33:141–147
Freitag SK, Woog JJ, Kousoubris PD, Curtin HD (2002) Helical computed tomographic dacryocystography with three-dimensional reconstruction-a new view of the lacrimal drainage system. Ophthalmic Plast Reconstr Surg 18:121–132
Tschopp M, Bornstein MM, Sendi P, Jacobs R, Goldblum D (2014) Dacryocystography using cone beam CT in patients with lacrimal drainage system obstruction. Ophthalmic Plast Reconstr Surg 30:486–491
Patella F, Panella S, Zannoni S, Jannone ML, Pesapane F, Angileri SA, Sbaraini S, Ierardi AM, Soldi S, Franceschelli G, Carrafiello G (2018) The role of interventional radiology in the treatment of epiphora. Gland Surg 7:103–110
Lindsley K, Nichols JJ, Dickersin K (2017) Non-surgical interventions for acute internal hordeolum. Cochrane Database Syst Rev 1:CD007742
Fayet B, Racy E, Assouline M, Zerbib M (2005) Surgical anatomy of the lacrimal fossa a prospective computed tomodensitometry scan analysis. Ophthalmology 112:1119–1128
Watanabe M, Buch K, Fujita A, Jara H, Qureshi MM, Sakai O (2017) Quantitative MR imaging of intra-orbital structures: tissue-specific measurements and age dependency compared to extra-orbital structures using multispectral quantitative MR imaging. Orbit 36:189–196
Zhang J, Chen L, Wang QX, Liu R, Zhu WZ, Luo X, Peng L, Xiong W (2015) Isotropic three-dimensional fast spin-echo cube magnetic resonance dacryocystography: comparison with the three-dimensional fast-recovery fast spin-echo technique. Neuroradiology 57:357–365
Higashi H, Tamada T, Mizukawa K, Ito K (2016) MR dacryocystography: comparison with dacryoendoscopy in positional diagnosis of nasolacrimal duct obstruction. Radiol Med 121:580–587
Sagili S, Selva D, Malhotra R (2012) Lacrimal scintigraphy: “interpretation more art than science”. Orbit 31:77–85
Shams PN, Chen PG, Wormald PJ, Sloan B, Wilcsek G, McNab A, Selva D (2014) Management of functional epiphora in patients with an anatomically patent dacryocystorhinostomy. JAMA Ophthalmol 132:1127–1132
Al-Faky YH (2013) Physiological utility of ultrasound biomicroscopy in the lacrimal drainage system. Br J Ophthalmol 97:1325–1329
Acknowledgements
We gratefully acknowledge Dr. Yue Geng (Fudan Eye & ENT Hospital) for performing DCG imaging, Dr. Yichen Li (Fudan Eye & ENT Hospital) for performing CT scan, and Dr. Shenjiang Wang (Fudan Eye & ENT Hospital) for performing MRI scan.
Funding
This work was supported by National Natural Science Foundation of China (grant number 81800867).
Author information
Authors and Affiliations
Contributions
Q.C., R.M., and Y.Y. conceived and designed research; H.R. served as scientific advisor; Y.Y. critically reviewed the study proposal; Q.C. and R.M. collected and analyzed the data; L.G. provided and cared for study patients; R.M. drafted the manuscript; Q.C., L.G., H.R. and Y.Y. edited and revised the manuscript; Q.C., R.M., L.G., H.R., and Y.Y. approved final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration
Authors declare no financial relationship with the organization that sponsored the research. Authors have full control of all primary data and agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review the primary data upon request.
Disclaimer
The views expressed in the manuscript are authors’ own and not an official position of the institution or funder.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Q., Ma, R., Gan, L. et al. Value of ultrasound biomicroscopy in assessment of small masses at medial canthal region. Graefes Arch Clin Exp Ophthalmol 257, 827–834 (2019). https://doi.org/10.1007/s00417-019-04252-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04252-y