Abstract
Purpose
Conventional chandelier-endoilluminators used for pars-plana vitrectomy consist of a light-emitting tip attached to an optical fibre. The tip requires introduction into the ocular space through an incision. To achieve complete illumination of the intraocular space, the introduction of more than just one tip is sometimes necessary. An extraocular vitreoretinal LED-endoilluminator discussed in this paper represents a new approach to illuminate the intraocular space. The light source is integrated into a speculum and firmly apposed to the sclera. This approach offers the advantage of effectively illuminating the interior of the eye even though the procedure is non-invasive. Furthermore, this approach significantly reduces the risk of damage to the retina by phototoxic effects.
Methods
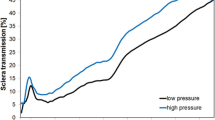
A round white LED was used as a light source. By integrating the light source into a speculum, the LED was firmly held against the sclera. Thus, the ocular space was illuminated transsclerally. As a result, indirect uniform illumination of the complete intraocular space was achieved. The prototype was developed considering the relevant international standards. Porcine eyes were used because their properties are similar to those of human eyes.
Results
Porcine eyes could be acceptably illuminated with the selected LED. The LED-endoilluminator conforms with international standards for endoillumination. Thus, possible photochemical and thermal risks are considered and reduced to a minimum.
Conclusions
A novel LED-endoilluminator which can be attached to a speculum was developed. The system does not need any connection to an external light source and, consequently, also avoids usage of an optical fibre. Regular and uniform illumination of the intraocular space was achieved by transmitted and scattered visible irradiation, avoiding an incision. The duration of potential light exposure, compared to existing illumination systems, can be significantly increased. This is also true when the illuminator is not directly placed over the pars-plana and the distance to the retina is reduced. Only a part of the light reaches the retina and the fraction of short wavelength becomes very small. Increased safety of the system results from now being able to increase the exposure time and reduce phototoxic stress to the retina.





Similar content being viewed by others
References
Ach T, Höh AE, Amberger R, Dithmar S (2008) Lichtexposition bei vitreoretinaler Chirurgie. Ophthalmologe 105:905–910. doi:10.1007/s00347-008-1795-y
Peyman GA (1976) Improved vitrectomy illumination system. Am J Ophthalmol 81:99–100
Peyman GA, Canakis C, Livir-Rallatos C, Easley J (2002) A new wide angle endoillumination probe for use during vitrectomy. Retina 22:242
Ryan EH (1997) Two shield bullet probes for panoramic endoillumination. Arch Ophthalmol 115:125–126
Sakaguchi H, Oshima Y (2012) Considering the Illumination Choices in Vitreoretinal Surgery. Continual improvements allow for better, safer outcomes. Retin Physican 9:26–31
DIN Deutsches Institut für Normung e. V (2014) Ophthalmische Instrumente – Grundlegende Anforderungen und Prüfverfahren – Teil 2: Schutz gegen Gefährdung durch Licht (ISO/DIS 15004–2:2014). Beuth Verlag, Berlin
DIN Deutsches Institut für Normung e. V (2013) Strahlungsphysik im optischen Bereich und Lichttechnik – Teil 10: Photobiologisch wirksame Strahlung, Größen, Kurzzeichen und Wirkungsspektren (DIN 5031–10). Beuth Verlag, Berlin
Ham WT, Mueller HA, Sliney DH (1976) Retinal sensitivity to damage from short wavelength light. Nature 260:153–155
Hünig S (2008) Optimierter Lichtschutz der Augen: eine dringende Aufgabe und ihre Lösung. Z prakt Augenheilkd 29:111–116
Mellerio J (1994) Light effects on the retina. In: Albert DM, Jakobiec FA (eds) Principles and practice of ophthalmology. WB Saunders, Philadelphia, pp 1–23
Udovičić L, Mainusch F, Janßen M, Nowack D, Ott G (2013) Photobiologische Sicherheit von Licht emittierenden Dioden (LED). Bundesanstalt für Arbeitsschutz und Arbeitssicherheit, Dortmund. http://www.baua.de/de/Publikationen/Fachbeitraege/F2115.pdf?__blob=publicationFile&v=6. Accessed 28 Dec 2014
Koch FHJ, Schmidt HP, Mönks T, Blumenröder S, Haller A, Steinmetz RL (1993) The retinal irradiance and spectral properties of the multiport illumination system for vitreous surgery. Am J Ophthalmol 116:489–496
Pepe IM (1999) Rhodopsin and phototransduction. J Photochem Photobiol B Biol 48:1–10
Remé CE (2005) The dark side of light: rhodopsin and the silent death of vision the proctor lecture. Invest Ophthalmol Vis Sci 46:2671–2682. doi:10.1167/iovs.04-1095
Różanowska M, Sarna T (2005) Light‐induced damage to the retina: role of rhodopsin chromophore revisited. Photochem Photobiol 81:1305–1330
Wu J, Seregard S, Algvere PV (2006) Photochemical damage of the retina. Surv Ophthalmol 51:461–481
Augustin AJ, Dick HB, Offermann I, Schmidt-Erfurth U (2002) Bedeutung oxidativer Mechanismen bei Erkrankungen der Netzhaut. Klin Monatsbl Augenheilkd 219:631–643
Augustin AJ, Dick HB, Winkgen A, Schmidt-Erfurth U (2001) Ursache und Prävention oxidativer Schäden des Auges. Ophthalmologe 98:776–797
Beatty S, Koh HH, Phil M, Henson D, Boulton M (2000) The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol 45:115–134
Bernstein PS, Nelson JL, Burrows JL, Askew EW (2003) Oxidative stress and age-related macular degeneration. In: Packer L, Podda M, Fuchs J (eds) Redox-Genome Interactions in Health and Disease CRC-press pp 367–391. doi: 10.1201/9780203912874.ch16
Evereklioglu C, Er H, Doganay S, Cekmen M, Turkoz Y, Otlu B, Ozerol E (2003) Nitric oxide and lipid peroxidation are increased and associated with decreased antioxidant enzyme activities in patients with age-related macular degeneration. Doc Ophthalmol 106:129–136
Halliwell B, Gutteridge JMC (1989) Free radicals in biology and medicine. Oxford University Press, Oxford
Jones DP (2006) Extracellular redox state: refining the definition of oxidative stress in aging. Rejuvenation Res 9:169–181
Ohia SE, Opere CA, LeDay AM (2005) Pharmacological consequences of oxidative stress in ocular tissues. Mutat Res/Fundam Mol Mech Mutagen 579:22–36. doi:10.1016/j.mrfmmm.2005.03.025
Eckardt C, Eckert T, Eckardt U (2008) 27-gauge twinlight chandelier illumination system for bimanual transconjunctival vitrectomy. Retina 28:518–519
Vogel A, Dlugos C, Nuffer R, Birngruber R (1991) Optical properties of human sclera, and their consequences for transscleral laser applications. Lasers Surg Med 11:331–340
Empfehlung der Strahlenschutzkommission (2006) Blendung durch natürliche und neue künstliche Lichtquellen und ihre Gefahren. http://www.ssk.de/SharedDocs/Beratungsergebnisse_PDF/2006/Blendung_Lichtquellen.html?nn=2041716. Accessed 20 Dec 2014
Jr H, William T, Mueller HA (1989) The photopathology and nature of the blue light and near-UV retinal lesions produced by lasers and other optical sources. In: Wolbarsht ML (ed) Laser applications in medicine and biology. Plenum Press, New York, pp 191–246
International Commission on Non-Ionizing Radiation Protection (1997) Guidelines on limits of exposure to broad-band incoherent optical radiation (0.38 to 3 mm). Health Phys 73:539–554
WHO/IRPA Task Group on Environmental Health Criteria for Lasers (1982) Lasers and optical radiation. WHO, Geneva. http://www.inchem.org/documents/ehc/ehc/ehc23.htm Accessed 28 Dec 2014
Sakaguchi H, Oshima Y, Nishida K, Awh CC (2011) A 29/30-gauge dualchandelier illumination system for panoramic viewing during microincision vitrectomy surgery. Retina 31:1231–1233. doi:10.1097/IAE.0b013e31822091ca
Dithmar S, Hoeh AE, Amberger R, Ruppenstein M, Ach T (2011) Light-emitting diode technology in vitreoretinal surgery. Retina 31:924–927. doi:10.1097/IAE.0b013e3181f44269
Bashkatov AN, Genina EA, Kochubey VI, Tuchin VV (2010) Optical properties of human sclera in spectral range 370–2500 nm. Opt Spectrosc 109:197–204
Rol P, Niederer P, Dürr U, Henchoz PD, Fankhauser F (1990) Experimental investigations on the light scattering properties of the human sclera. Lasers Light Ophthalmol 3:201–212
Benedek GB (1971) Theory of transparency of the eye. Appl Opt 10:459–473
Köll R (1990) Experimentelle Untersuchungen zur Sklerotomie mittels Nd:YAG Laser. Dissertation, Ludwig-Maximilians-University of Munich
Torczynski E (1988) Choroid and suprachoroid. In: Duane TD, Jaeger EA (eds) Biomedical foundations of ophthalmology. J.B. Lippincott, Philadelphia, pp 1–33
Novack R L (2009) The CONSTELLATION Vision System: Assessing the Improvements in Illumination for Vitreoretinal Surgery. Retinal Physician, http://www.retinalphysician.com/articleviewer.aspx?articleID=102828. Accessed 28 Feb 2015
Nuffer R (1988) Transsklerale Streuungs- und Absorptionsmessung. Diploma thesis, Polytechnical University of Munich
Eckardt C (2003) Twin lights: a new chandelier illumination for bimanual surgery. Retina 23:893–894
Oshima Y, Awh CC, Tano Y (2007) Self-retaining 27-gauge transconjunctival chandelier endoillumination for panoramic viewing during vitreous surgery. Am J Ophthalmol 143:166–167
Oshima Y, Chow DR, Awh CC, Sakaguchi H, Tano Y (2008) Novel mercury vapor illuminator combined with a 27/29-gauge chandelier light fiber for vitreous surgery. Retina 28:171–173
Conflict of Interest
Svenja Deuchler, Pankaj Singh and Frank Koch have no conflicts of interests. Philipp Simon Kölbl, Christoph Lindner, Christian Lingenfelder and Martin Hessling filed a German patent application in November 2014.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kölbl, P.S., Lindner, C., Lingenfelder, C. et al. An extraocular non-invasive transscleral LED-endoilluminator for eye speculum integration. Graefes Arch Clin Exp Ophthalmol 253, 1529–1535 (2015). https://doi.org/10.1007/s00417-015-3036-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3036-9