Abstract
Objectives
To investigate whether a history of traumatic brain injury (TBI) is associated with greater long-term grey-matter loss in patients with mild cognitive impairment (MCI).
Methods
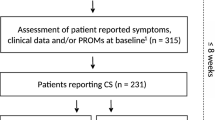
85 patients with MCI were identified, including 26 with a previous history of traumatic brain injury (MCI[TBI-]) and 59 without (MCI[TBI+]). Cortical thickness was evaluated by segmenting T1-weighted MRI scans acquired longitudinally over a 2-year period. Bayesian multilevel modelling was used to evaluate group differences in baseline cortical thickness and longitudinal change, as well as group differences in neuropsychological measures of executive function.
Results
At baseline, the MCI[TBI+] group had less grey matter within right entorhinal, left medial orbitofrontal and inferior temporal cortex areas bilaterally. Longitudinally, the MCI[TBI+] group also exhibited greater longitudinal declines in left rostral middle frontal, the left caudal middle frontal and left lateral orbitofrontal areas sover the span of 2 years (median = 1–2%, 90%HDI [−0.01%: −0.001%], probability of direction (PD) = 90–99%). The MCI[TBI+] group also displayed greater longitudinal declines in Trail-Making-Test (TMT)-derived ratio (median: 0.737%, 90%HDI: [0.229%: 1.31%], PD = 98.8%) and differences scores (median: 20.6%, 90%HDI: [−5.17%: 43.2%], PD = 91.7%).
Conclusions
Our findings support the notion that patients with MCI and a history of TBI are at risk of accelerated neurodegeneration, displaying greatest evidence for cortical atrophy within the left middle frontal and lateral orbitofrontal frontal cortex. Importantly, these results suggest that long-term TBI-mediated atrophy is more pronounced in areas vulnerable to TBI-related mechanical injury, highlighting their potential relevance for diagnostic forms of intervention in TBI.




Similar content being viewed by others
References
Nordström A, Nordström P (2018) Traumatic brain injury and the risk of dementia diagnosis: a nationwide cohort study. PLoS Med 15(1):e1002496. https://doi.org/10.1371/journal.pmed.1002496
Graham NS, Sharp DJ (2019) Understanding neurodegeneration after traumatic brain injury: from mechanisms to clinical trials in dementia. J Neurol Neurosurg Psychiatry 90:1221–1233
Guo Z, Cupples LA, Kurz A, Auerbach SH, Volicer L, Chui H et al (2000) Head injury and the risk of AD in the MIRAGE study. Neurology 54:1316–1323. https://doi.org/10.1212/WNL.54.6.1316
Schofield PW, Tang M, Marder K, Bell K, Dooneief G, Chun M et al (1997) Alzheimer’s disease after remote head injury: an incidence study. J Neurol Neurosurg Psychiatry 62:119–124. https://doi.org/10.1136/jnnp.62.2.119
Plassman BL, Havlik RJ, Steffens DC, Helms MJ, Newman TN, Drosdick D et al (2000) Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology 55:1158–1166. https://doi.org/10.1212/WNL.55.8.1158
LoBue C, Wadsworth H, Wilmoth K, Clem M, Hart J, Womack KB et al (2017) Traumatic brain injury history is associated with earlier age of onset of Alzheimer disease. Clin Neuropsychol 31:85–98. https://doi.org/10.1080/13854046.2016.1257069
Gedye A, Beattie BL, Tuokko H, Horton A, Korsarek E (1989) Severe head injury hastens age of onset of Alzheimer’s disease. J Am Geriatr Soc 37(10):970–973. https://doi.org/10.1111/j.1532-5415.1989.tb07283.x
Mortimer JA, van Duijn CM, Chandra V, Fratiglioni L, Graves AB, Heyman A, Jorm AF, Kokmen E, Kondo K, Rocca WA et al (1991) Head trauma as a risk factor for Alzheimer’s disease: a collaborative re-analysis of case-control studies. EURODEM Risk Factors Research Group. Int J Epidemiol 20(Suppl 2):S28–S35. https://doi.org/10.1093/ije/20.supplement_2.s28
Sullivan P, Petitti D, Barbaccia J (1987) Head trauma and age of onset of dementia of the Alzheimer type. JAMA 257(17):2289–2290. https://doi.org/10.1001/jama.1987.03390170045014
Barnes DE, Kaup A, Kirby KA, Byers AL, Diaz-Arrastia R, Yaffe K (2014) Traumatic brain injury and risk of dementia in older veterans. Neurology 83(4):312–319. https://doi.org/10.1212/WNL.0000000000000616
Gardner RC, Burke JF, Nettiksimmons J, Kaup A, Barnes DE, Yaffe K (2014) Dementia risk after traumatic brain injury vs. nonbrain trauma: the role of age and severity. JAMA Neurol 71(12):1490–1497. https://doi.org/10.1001/jamaneurol.2014.2668
DeKosky ST, Asken BM (2017) Injury cascades in TBI-related neurodegeneration. Brain Inj 31(9):1177–1182. https://doi.org/10.1080/02699052.2017.1312528
Hosomi S, Ohnishi M, Ogura H, Shimazu T (2020) Traumatic brain injury-related inflammatory projection: beyond local inflammatory responses. Acute Med Surg 7(1):e520. https://doi.org/10.1002/ams2.520
Xiong Y, Mahmood A, Chopp M (2018) Current understanding of neuroinflammation after traumatic brain injury and cell-based therapeutic opportunities. Chin J Traumatol 21(3):137–151. https://doi.org/10.1016/j.cjtee.2018.02.003
Simon D, McGeachy M, Bayır H et al (2017) The far-reaching scope of neuroinflammation after traumatic brain injury. Nat Rev Neurol 13:171–191. https://doi.org/10.1038/nrneurol.2017.13
Mills BD, Goubran M, Parivash SN, Dennis EL, Rezaii P, Akers C, Bian W, Mitchell LA, Boldt B, Douglas D, Sami S, Mouchawar N, Wilson EW, DiGiacomo P, Parekh M, Do H, Lopez J, Rosenberg J, Camarillo D, Grant G, Wintermark M, Zeineh M (2020) Longitudinal alteration of cortical thickness and volume in high-impact sports. Neuroimage 217:116864. https://doi.org/10.1016/j.neuroimage.2020.116864
Cole JH, Jolly A, de Simoni S, Bourke N, Patel MC, Scott G, Sharp DJ (2018) Spatial patterns of progressive brain volume loss after moderate-severe traumatic brain injury. Brain 141(3):822–836. https://doi.org/10.1093/brain/awx354
Scheid R, Walther K, Guthke T et al (2006) Cognitive sequelae of diffuse axonal injury. Arch Neurol 63:418–424
Wilde EA et al (2021) Developmental alterations in cortical organization and socialization in adolescents who sustained a traumatic brain injury in early childhood. J Neurotrauma 38(1):133–143. https://doi.org/10.1089/neu.2019.6698
Govindarajan KA, Narayana PA, Hasan KM et al (2016) Cortical thickness in mild traumatic brain injury. J Neurotrauma 33(20):1809–1817. https://doi.org/10.1089/neu.2015.4253
Santhanam P, Wilson SH, Oakes TR, Weaver LK (2019) Accelerated age-related cortical thinning in mild traumatic brain injury. Brain Behav 9(1):e01161. https://doi.org/10.1002/brb3.1161
Mazaharally M, Stojanovski S, Trossman R, Szulc-Lerch K, Chakravarty MM, Colella B, Glazer J, Green RE, Wheeler AL (2022) Patterns of change in cortical morphometry following traumatic brain injury in adults. Hum Brain Mapp 43(6):1882–1894. https://doi.org/10.1002/hbm.25761
Gardener SL et al (2021) Longitudinal trajectories in cortical thickness and volume atrophy: superior cognitive performance does not protect against brain atrophy in older adults. J Alzheimers Dis 81(3):1039–1052
Armstrong RC, Mierzwa AJ, Marion CM, Sullivan GM (2016) White matter involvement after TBI: clues to axon and myelin repair capacity. Exp Neurol 275(Pt 3):328–333. https://doi.org/10.1016/j.expneurol.2015.02.011
Strain JF, Womack KB, Didehbani N et al (2015) Imaging correlates of memory and concussion history in retired national football league athletes. JAMA Neurol 72(7):773–780. https://doi.org/10.1001/jamaneurol.2015.0206
Edmonds EC, Weigand AJ, Hatton SN, Marshall AJ, Thomas KR, Ayala DA, Bondi MW, McDonald CR, Alzheimer’s Disease Neuroimaging Initiative (2020) Patterns of longitudinal cortical atrophy over 3 years in empirically derived MCI subtypes. Neurology 94(24):e2532–e2544. https://doi.org/10.1212/WNL.0000000000009462
Farhan SM, Bartha R, Black SE, Corbett D, Finger E, Freedman M, Greenberg B, Grimes DA, Hegele RA, Hudson C, Kleinstiver PW, Lang AE, Masellis M, McIlroy WE, McLaughlin PM, Montero-Odasso M, Munoz DG, Munoz DP, Strother S, Swartz RH, Symons S, Tartaglia MC, Zinman L, ONDRI Investigators, Strong MJ (2017) The Ontario neurodegenerative disease research initiative (ONDRI). Can J Neurol Sci 44(2):196–202
McLaughlin PM, Sunderland KM, Beaton D, Binns MA, Kwan D, Levine B, Orange JB, Peltsch AJ, Roberts AC, Strother SC, Troyer AK (2021) The quality assurance and quality control protocol for neuropsychological data collection and curation in the Ontario neurodegenerative disease research initiative (ONDRI) Study. Assessment 28(5):1267–1286. https://doi.org/10.1177/1073191120913933
Vaccarino AL, Dharsee M, Strother S, Aldridge D, Arnott SR, Behan B, Dafnas C, Dong F, Edgecombe K, El-Badrawi R, El-Emam K, Gee T, Evans SG, Javadi M, Jeanson F, Lefaivre S, Lutz K, MacPhee FC, Mikkelsen J, Mikkelsen T et al (2018) Brain-CODE: a secure neuroinformatics platform for management, federation, sharing and analysis of multi-dimensional neuroscience data. Front Neuroinform 12:28. https://doi.org/10.3389/fninf.2018.00028
Ramirez J, Holmes MF, Scott CJM, Ozzoude M, Adamo S, Szilagyi GM, Goubran M, Gao F, Arnott SR, Lawrence-Dewar JM, Beaton D, Strother SC, Munoz DP, Masellis M, Swartz RH, Bartha R, Symons S, Black SE, ONDRI Investigators (2020) Ontario neurodegenerative disease research initiative (ONDRI): structural MRI methods and outcome measures. Front Neurol 11:847. https://doi.org/10.3389/fneur.2020.00847
Reuter M, Rosas HD, Fischl B (2010) Highly accurate inverse consistent registration: a robust approach. Neuroimage 53(4):1181–1196
Ozzoude, M., Ramirez, J., Raamana, P.R., Holmes, F.M., Walker, K., Scott, J.M.C., Gao, F., Goubran, M., Kwan, D., Tartaglia, C.M., Beaton, D., Saposnik, G., Hassan, A., Lawrence-Dewar, J., Dowlatshahi, D., Strother, C.S., Symons, S., Bartha, R., Swartz, H.R., Black, E.S.; on behalf of the ONDRI Investigators (2020) Cortical thickness estimation in individuals with cerebral small vessel disease, focal atrophy, and chronic stroke lesions. Front Neurosci. https://doi.org/10.3389/fnins.2020.598868
Drane DL, Yuspeh RL, Huthwaite JS, Klingler LK (2002) Demographic characteristics and normative observations for derived-trail making test indices. Neuropsychiatry Neuropsychol Behav Neurol 15(1):39–43
Corrigan JD, Hinkeldey NS (1987) Relationships between parts A and B of the Trail Making Test. J Clin Psychol 43(4):402–409. https://doi.org/10.1002/1097-4679(198707)43:4%3c402::aid-jclp2270430411%3e3.0.co;2-e
Lange RT, Iverson GL, Zakrzewski MJ, Ethel-King PE, Franzen MD (2005) Interpreting the trail making test following traumatic brain injury: comparison of traditional time scores and derived indices. J Clin Exp Neuropsychol 27(7):897–906. https://doi.org/10.1080/1380339049091290
Lamberty GJ, Putnam SH, Chatel DM, Bieliauskas LA et al (1994) Derived trail making test indices: a preliminary report. Neuropsychiatry Neuropsychol Behav Neurol 7(3):230–234
Arbuthnott K, Frank J (2000) Trail making test, part B as a measure of executive control: validation using a set-switching paradigm. J Clin Exp Neuropsychol 22(4):518–528. https://doi.org/10.1076/1380-3395(200008)22:4;1-0;FT518
Lezak MD, Howieson DB, Bigler ED, Tranel D (2012) Neuropsychological assessment, 5th edn. Oxford University Press, Oxford
Periáñez JA, Ríos-Lago M, Rodríguez-Sánchez JM, Adrover-Roig D, Sánchez-Cubillo I, Crespo-Facorro B, Quemada JI, Barceló F (2007) Trail making test in traumatic brain injury, schizophrenia, and normal ageing: sample comparisons and normative data. Arch Clin Neuropsychol 22(4):433–447. https://doi.org/10.1016/j.acn.2007.01.022
Martin TA, Hoffman NM, Donders J (2003) Clinical utility of the trail making test ratio score. Appl Neuropsychol 10(3):163–169. https://doi.org/10.1207/S15324826AN1003_05
Sánchez-Cubillo I, Periáñez JA, Adrover-Roig D, Rodríguez-Sánchez JM, Ríos-Lago M, Tirapu J, Barceló F (2009) Construct validity of the trail making test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc 15(3):438–450. https://doi.org/10.1017/S1355617709090626
Gavett BE, Stern RA, Cantu RC et al (2010) Mild traumatic brain injury: a risk factor for neurodegeneration. Alzheimers Res Ther 2:18. https://doi.org/10.1186/alzrt42
Gu D, Ou S, Liu G (2022) Traumatic brain injury and risk of dementia and Alzheimer’s disease: a systematic review and meta-analysis. Neuroepidemiology 56(1):4–16. https://doi.org/10.1159/000520966
Julien J, Joubert S, Ferland MC, Frenette LC, Boudreau-Duhaime MM, Malo-Véronneau L, de Guise E (2017) Association of traumatic brain injury and Alzheimer disease onset: a systematic review. Ann Phys Rehabil Med 60(5):347–356. https://doi.org/10.1016/j.rehab.2017.03.009
Gilbert M, Snyder C, Corcoran C, Norton MC, Lyketsos CG, Tschanz JT (2014) The association of traumatic brain injury with rate of progression of cognitive and functional impairment in a population-based cohort of Alzheimer’s disease: the cache county dementia progression study. Int Psychogeriatr 26:1593–1601. https://doi.org/10.1017/S1041610214000842
Yao Z, Hu B, Liang C, Zhao L, Jackson M, Alzheimer’s Disease Neuroimaging Initiative (2012) A longitudinal study of atrophy in amnestic mild cognitive impairment and normal aging revealed by cortical thickness. PLoS ONE 7(11):e48973. https://doi.org/10.1371/journal.pone.0048973
Machulda MM, Lundt ES, Albertson SM, Spychalla AJ, Schwarz CG, Mielke MM, Jack CR Jr, Kremers WK, Vemuri P, Knopman DS, Jones DT, Bondi MW, Petersen RC (2020) Cortical atrophy patterns of incident MCI subtypes in the Mayo clinic study of aging. Alzheimers Dement 16(7):1013–1022. https://doi.org/10.1002/alz.12108
Whitwell JL, Petersen RC, Negash S, Weigand SD, Kantarci K, Ivnik RJ, Knopman DS, Boeve BF, Smith GE, Jack CR Jr (2007) Patterns of atrophy differ among specific subtypes of mild cognitive impairment. Arch Neurol 64(8):1130–1138. https://doi.org/10.1001/archneur.64.8.1130
Bigler ED (2007) Anterior and middle cranial fossa in traumatic brain injury: relevant neuroanatomy and neuropathology in the study of neuropsychological outcome. Neuropsychology 21(5):515–531. https://doi.org/10.1037/0894-4105.21.5.515
Pang D (1989) Physics and pathology of closed head injury. In: Lezak M, Liss AR (eds) Assessment of the behavioral consequences of head trauma. Liss, New York, pp 1–17
Schimmel SJ, Acosta S, Lozano D (2017) Neuroinflammation in traumatic brain injury: a chronic response to an acute injury. Brain Circ 3(3):135–142. https://doi.org/10.4103/bc.bc_18_17
Yang S-T, Hsiao I-T, Hsieh C-J, Chiang Y-H, Yen T-C, Chiu W-T et al (2015) Accumulation of amyloid in cognitive impairment after mild traumatic brain injury. J Neurol Sci 349:99–104. https://doi.org/10.1016/j.jns.2014.12.032
LoBue C, Munro C, Schaffert J, Didehbani N, Hart J, Batjer H, Cullum CM (2019) Traumatic brain injury and risk of long-term brain changes, accumulation of pathological markers, and developing dementia: a review. J Alzheimers Dis 70(3):629–654. https://doi.org/10.3233/JAD-190028
Witcher KG, Bray CE, Chunchai T, Zhao F, O’Neil SM, Gordillo AJ, Campbell WA, McKim DB, Liu X, Dziabis JE, Quan N, Eiferman DS, Fischer AJ, Kokiko-Cochran ON, Askwith C, Godbout JP (2021) Traumatic brain injury causes chronic cortical inflammation and neuronal dysfunction mediated by microglia. J Neurosci 41(7):1597–1616. https://doi.org/10.1523/JNEUROSCI.2469-20.2020
Jellinger KA, Attems J (2013) Neuropathological approaches to cerebral aging and neuroplasticity. Dialogues Clin Neurosci 15(1):29–43. https://doi.org/10.31887/DCNS.2013.15.1/kjellinger
Troyer AK, Moscovitch M, Winocur G, Alexander MP, Stuss D (1998) Clustering and switching on verbal fluency: the effects of focal frontal- and temporal-lobe lesions. Neuropsychologia 36(6):499–504. https://doi.org/10.1016/s0028-3932(97)00152-8
Henry JD, Crawford JR (2004) A meta-analytic review of verbal fluency performance following focal cortical lesions. Neuropsychology 18(2):284–295. https://doi.org/10.1037/0894-4105.18.2.284
Passingham R (1975) Delayed matching after selective prefrontal lesions in monkeys (Macaca mulatta). Brain Res 92:89–102
Naqvi N, Tranel D, Bechara A (2006) Visceral and decision-making functions of the ventromedial prefrontal cortex. In: Zald DH, Rauch SL (eds) Orbitofrontal cortex. Oxford University Press, Oxford
Meunier M, Bachevalier J, Mishkin M (1997) Effects of orbital frontal and anterior cingulate lesions on object and spatial memory in rhesus monkeys. Neuropsychologia 35:999–1015
Zald DH, Andreotti C (2010) Neuropsychological assessment of the orbital and ventromedial prefrontal cortex. Neuropsychologia 48(12):3377–3391. https://doi.org/10.1016/j.neuropsychologia.2010.08.012
Barbey AK, Koenigs M, Grafman J (2011) Orbitofrontal contributions to human working memory. Cereb Cortex 21(4):789–795. https://doi.org/10.1093/cercor/bhq153
Chan E, MacPherson SE, Robinson G, Turner M, Lecce F, Shallice T, Cipolotti L (2015) Limitations of the trail making test part-B in assessing frontal executive dysfunction. J Int Neuropsychol Soc 21(2):169–174. https://doi.org/10.1017/S135561771500003X
Schwarz CG, Gunter JL, Wiste HJ, Przybelski SA, Weigand SD, Ward CP, Senjem ML, Vemuri P, Murray ME, Dickson DW, Parisi JE, Kantarci K, Weiner MW, Petersen RC, Jack CR Jr, Alzheimer’s Disease Neuroimaging Initiative (2016) A large-scale comparison of cortical thickness and volume methods for measuring Alzheimer’s disease severity. Neuroimage Clin 11:802–812. https://doi.org/10.1016/j.nicl.2016.05.017
Knussmann GN, Anderson JS, Prigge MBD, Dean DC III, Lange N, Bigler ED, Alexander AL, Lainhart JE, Zielinski BA, King JB (2022) Test-retest reliability of FreeSurfer-derived volume, area and cortical thickness from MPRAGE and MP2RAGE brain MRI images. Neuroimage Rep 2(2):100086. https://doi.org/10.1016/j.ynirp.2022.100086
Acknowledgements
The authors acknowledge ONDRI’s participants, clinical coordinators, and other research team members including Catarina Downey, Heather Hink, Donna McBain, Lindsey McLeish, and Alicia J. Peltsch. This research was conducted with the support of the Ontario Brain Institute, an independent non-profit corporation, funded partially by the Ontario government. The opinions, results, and conclusions are those of the authors and no endorsement by the Ontario Brain Institute is intended or should be inferred. Matching funds were provided by participant hospital (recruitment sites) and research institute foundations, including the Baycrest Foundation, Bruyère Research Institute, Centre for Addiction and Mental Health Foundation, London Health Sciences Foundation, McMaster University Faculty of Health Sciences, Ottawa Brain and Mind Research Institute, Queen’s University Faculty of Health Sciences, the Sunnybrook Foundation, the Thunder Bay Regional Health Sciences Centre, the University of Ottawa Faculty of Medicine, and the Windsor/Essex County ALS Association. The Temerty Family Foundation provided the major infrastructure matching funds.
Funding
Angela Christine Roberts: (1) Salary support from the Canada Research Chairs program. (2) Travel stipends from the Movement Disorders Society and World Parkinson Congress. Sanjeev Kumar: (1) Research support from Brain and Behavior Foundation, National institute on Ageing, BrightFocus Foundation, Brain Canada, Canadian Institute of Health Research, Canadian Consortium on Neurodegeneration in Aging, Centre for Ageing and Brain Health Innovation, Centre for Addiction and Mental Health, and an Academic Scholars Award from the Department of Psychiatry, University of Toronto. Equipment support from Soterix Medical. Stephen R. Arnott: (1) Consultation work for Indoc Research. Maria C. Tartaglia: (1) NIH, Weston Brain Foundation, Tanenbaum Institute for Science in Sport. (2) Consultant: Eli Lilly, EISAI. (3) Scientific advisor Women’s Brain Project, Brain Injury Canada, PSP Canada. (4) Clinical trials: Passage Bio, Janssen, Biogen, Avanex, Green Valley, Roche, GSK, BMS. Bruce Pollock: (1) Dr. Bruce G. Pollock receives research support from the Peter & Shelagh Godsoe Endowed Chair in Late-Life Mental Health, CAMH Foundation, and Discovery Fund, National Institute of Aging, Brain Canada, the Canadian Institutes of Health Research, the Alzheimer’s Drug Discovery Foundation, the Ontario Brain Institute, the Centre for Aging and Brain Health Innovation, the Bright Focus Foundation, the Alzheimer’s Society of Canada, the W. Garfield Weston Foundation, the Weston Brain Institute, the Canadian Consortium on Neurodegeneration in Aging and Genome Canada. Dr. Pollock receives honoraria from the American Geriatrics Society for book authorship and holds United States Provisional Patent Nos. 6/490,680, 17/396,030 and Canadian Provisional Patent No. 3,054,093 for a cell-based assay and kits for assessing serum anticholinergic activity. Tarek K. Rajji: (1) Dr. Rajji has received research support from Brain Canada, Brain and Behavior Research Foundation, BrightFocus Foundation, Canada Foundation for Innovation, Canada Research Chair, Canadian Institutes of Health Research, Centre for Aging and Brain Health Innovation, National Institutes of Health, Ontario Ministry of Health and Long-Term Care, Ontario Ministry of Research and Innovation, and the Weston Brain Institute. Dr. Rajji also received for an investigator-initiated study in-kind equipment support from Newronika, and in-kind research online accounts from Scientific Brain Training Pro, and participated in 2021 and 2022 in an advisory activity for Biogen Canada Inc. As of September 1, 2023, Dr. Rajji is an ex officio member of the Board of Trustees of the Centre for Addiction and Mental Health (CAMH) in his role as Chair of the Medical Advisory Committee at CAMH. Dr. Rajji is also an inventor on the United States Provisional Patent No. 17/396,030 that describes cell-based assays and kits for assessing serum cholinergic receptor activity. David F. Tang-Wai: (1) Hydrocephalus Canada medical advisory board. Corinne E. Fischer: (1) Grant Funding For: NIH, NIA, CCNA, CIHR, St. Michaels Hospital Foundation, Hilary and Galen Weston Foundation, ADDF and Novo Nordisk.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The following authors have no conflicts of interest/disclosures: Marc A. Khoury, Nathan W. Churchill, Alex Di Battista, Simon J. Graham, Sean Symons, Angela K. Troyer, Brian Tan, Joel Ramirez, Stephen H. Pasternak, Michael Borrie, Andrew Frank, Michaels Borrie, Christopher J. M. Scott, Seyyed Mohammad Hassan Haddad, Nuwan Nanayakkara, Joseph B. Orange, Alicia Peltsch, David G. Munoz, Tom A. Schweizer.
Ethical standards
All the procedures have been completed in compliance with the ethical standards of the Committee on Human Experimentation of the institution under the accord of the Helsinki Declaration of 1975. No animal experiments were undertaken for this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khoury, M.A., Churchill, N.W., Di Battista, A. et al. History of traumatic brain injury is associated with increased grey-matter loss in patients with mild cognitive impairment. J Neurol (2024). https://doi.org/10.1007/s00415-024-12369-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00415-024-12369-2