Abstract
Newborn screening for 5qSMA offers the potential for early, ideally pre-symptomatic, therapeutic intervention. However, limited data exist on the outcomes of individuals with 4 copies of SMN2, and there is no consensus within the SMA treatment community regarding early treatment initiation in this subgroup. To provide evidence-based insights into disease progression, we performed a retrospective analysis of 268 patients with 4 copies of SMN2 from the SMArtCARE registry in Germany, Austria and Switzerland. Inclusion criteria required comprehensive baseline data and diagnosis outside of newborn screening. Only data prior to initiation of disease-modifying treatment were included. The median age at disease onset was 3.0 years, with a mean of 6.4 years. Significantly, 55% of patients experienced symptoms before the age of 36 months. 3% never learned to sit unaided, a further 13% never gained the ability to walk independently and 33% of ambulatory patients lost this ability during the course of the disease. 43% developed scoliosis, 6.3% required non-invasive ventilation and 1.1% required tube feeding. In conclusion, our study, in line with previous observations, highlights the substantial phenotypic heterogeneity in SMA. Importantly, this study provides novel insights: the median age of disease onset in patients with 4 SMN2 copies typically occurs before school age, and in half of the patients even before the age of three years. These findings support a proactive approach, particularly early treatment initiation, in this subset of SMA patients diagnosed pre-symptomatically. However, it is important to recognize that the register will not include asymptomatic individuals.
Similar content being viewed by others
Introduction
Spinal muscular atrophy (SMA) is a genetic disorder characterized by the degeneration of motor neurons in the spinal cord and brain stem, leading to muscle weakness and wasting. The disease is caused by a deficiency of the survival motor neuron (SMN) protein, which is crucial for the normal development and function of motor neurons [1, 2]. SMA is the most common neurodegenerative disease in childhood and the second most common recessive disease after cystic fibrosis, with an incidence ranging from 1:6000 to 1:11,000 [3].
A bi-allelic loss of the SMN1 gene, often due to a homozygous deletion, is responsible for the autosomal recessive disease in over 95% of cases, resulting in SMN protein deficiency [4]. Approximately 5% of cases are attributed to point mutations in one or both alleles [5]. The SMN1 gene is responsible for producing most of the functional SMN protein. Humans also possess a gene called SMN2, which is paralogous to SMN1 but differs by only a few nucleotides. As a result, SMN2 primarily produces non-functional protein due to aberrant splicing during transcription. The severity of SMA, except in cases involving rarer, less understood genetic modifiers [6] is largely determined by the quantity of functional SMN protein generated by the SMN2 gene. This compensatory mechanism partially mitigates the loss of SMN1 and modulates the SMA phenotype because a small proportion of SMN2 transcripts undergo alternative splicing. This results in the production of approximately 5–10% of full-length functional SMN protein, with the severity of SMA strongly influenced by individual variations in SMN2 copy number.
Three SMN-targeted medications have been approved in Europe and the US between 2016 and 2021: Nusinersen (Spinraza®), onasemnogene abeparvovec xioi (Zolgensma®), and risdiplam (Evrysdi®). These medications either replace the deleted SMN1 gene using a viral vector or improve aberrant splicing of the SMN2 gene. All three of these active agents can provide the missing SMN protein [7,8,9,10,11]. However, the timing of treatment is crucial for its effectiveness, as damaged motor neurons poorly regenerate even when SMN protein is restored. Therefore, a substantial number of additional countries worldwide now have SMA included in newborn screening programs in pilot projects or for regular clinical use. It is currently being tested in other countries.
According to the literature, individuals with four copies of SMN2 typically exhibit a milder form of SMA compared to those with fewer copies [12, 13], and there are cases of individuals who remain mildly symptomatic or asymptomatic into advanced age [14, 15]. However, in the literature, it has been more common to classify SMA by type rather than by copy number, and there is limited available data on populations exclusively composed of individuals with 4 copies of SMN2. Existing studies have reported significant variability in the clinical presentation and disease progression of SMA in individuals with 4 SMN2 copies (16, 17). A recent study published in 2022, which originally focused on gender differences, reported a median age of onset for their 4-copy SMA cohort of 4.75 years (13), and another very recent study from Italy, which focused on disease progression and subgroup classification, revealed that 22% of their patients developed the disease before the age of 3 years [16]. In a recent study from the German SMA Newborn Screening Model Projects, we were able to demonstrate that a notable proportion of SMA patients with 4 SMN2 copies (5 of 7 patients, all subjects investigated under the age of 5) developed the disease between 1.5 and 4 years, with the majority experiencing very subtle symptoms [17], but some individuals suffering from significant and irreversible motor regression.
Overall, there is no description of the natural history and no consensus on treatment indications for this subset of SMA. This lack of agreement is also evident in the management following newborn screening, which has been introduced in several countries in recent years [18,19,20,21]. Following a positive newborn screening for SMA, a decision must be made concerning therapy. There is a clear consensus that individuals with 2 and 3 copies of SMN2 should receive immediate treatment, while there is uncertainty regarding treatment indications for those with 4 copies of SMN2 [22]. This disparity is reflected in the 2018 recommendations from the US expert group [23], which recommended a watchful waiting approach for individuals with 4 SMN2 copies after NBS, and their 2020 guideline revision [24], which suggested early initiation of therapy.
Further research is required to enhance our comprehension of the natural history and clinical progression of SMA with 4 SMN2 copies, along with identifying factors that could potentially impact disease severity and progression in this patient group. In this manuscript, we present a standardized retrospective evaluation of natural history data drawn from the SMA registry “SMArtCARE” involving 268 patients with 4 SMN2 copies.
Materials and methods
SMArtCARE, a disease-specific registry, currently encompasses 58 participating centres in Germany, Austria, and Switzerland. Its primary objective is to collect prospective, longitudinal data on SMA patients. Additionally, it retains retrospective data (medical history) acquired prior to inclusion in the registry and before therapy initiation. As of July 2023, the registry contains information on 1,648 patients of varying ages, SMA types, and treatment modalities. To be eligible for inclusion in SMArtCARE, patients must meet two criteria: they must possess genetically confirmed 5q SMA and provide written informed consent, obtained either from the patient or their caregiver.
Since the implementation of SMArtCARE in 2018, data collection occurs prospectively during routine patient visits to capture real-world outcomes. To maintain consistency, standardized case report forms are utilized to document data rather than extracting information from medical records. These forms adhere to international consensus guidelines for SMA registries and encompass various aspects such as motor function, motor milestones, respiratory and orthopaedic symptoms, adverse events, and genetic test results. Treating physicians record genetic test results, including SMN2 copy numbers, based on the patients' original genetic test results. Currently, 90.4% of all patients in the registry have undergone SMN2 copy number determination, with 23.2% possessing 4 SMN2 copies. It is important to note that SMN2 copy numbers are not centrally assessed within the SMArtCARE registry, but are entered by the treating clinicians based on the results from the genetic laboratories.
For the analysis of the patient cohort, we exclusively considered patients registered with 4 SMN2 copies. Inclusion criteria comprised a minimum age of 18 months and either complete attainment of motor milestones (independent walking) before initiating drug therapy or, if independent walking had not been achieved, a minimum age of 5 years at the onset of drug therapy. Patients identified as presymptomatic through newborn screening were excluded from the analysis.
The following parameters were extracted from the registry for statistical analysis: "year of birth," "age at milestones" (sitting unsupported, walking unsupported), "age at symptom onset," "first symptoms or signs leading to suspicion of SMA (free text field)," "wheelchair use," "nutrition (use of feeding tube)," "presence and/or surgery of scoliosis," "need for mechanical ventilation," and the results of the motor tests "6MWT," "RULM," and "HFSME." These baseline characteristics were obtained from the treatment centres through a patient/family medical history survey.
Statistical analyses were conducted using the "R" programming language (Open-Source-Software) and Microsoft Excel 2016 (Microsoft Corporation, Redmond, Washington, USA). The results underwent manual verification for plausibility, and individual patient entries were reconciled. Implausible entries were either corrected if unequivocal or changed to 'unknown'. In the case of 20 patients, the entry "sitting independently was not achieved" was modified to "sitting independently achieved at an unknown age," as this was evidently an incorrect entry, given that all these patients were ambulatory at baseline, corroborated by the "walk test" results. The same correction applies to 18 entries regarding the acquisition of the milestone "walking unaided."
Results
A total of 303 patients met the criteria of being at least 18 months of age and having 4 copies of SMN2. Thirty-two patients, born between 2018 and 2021, were detected by newborn screening and were, therefore, excluded. Three patients, born between 2015 and 2018, initiated drug therapy before achieving independent sitting/walking, leading to their exclusion. Consequently, 268 patients were included. The years of birth ranged from 1948 to 2016, and the patients’ ages at baseline ranged from 3 to 75 years (median 29.6, mean 27 years).
Age of symptom onset
Disease onset ranged from 1 month to 47 years of age (median 3.0 years, mean 6.4 years; information was available in all patients). 147 patients (55%) experienced disease onset within the first 36 months of age. The age at symptom onset is presented as a Kaplan–Meier curve in Fig. 1.
Type of first symptoms
The most common initial symptoms included gait instability, muscle weakness, delayed motor development, frequent falls, decreased performance in sports compared to peers, muscle hypotonia in infancy, tremor, fatigue, and difficulty running and/or climbing stairs. Table 1 provides an overview.
Motor milestones
The cohort learned to sit unaided at ages ranging from 5 to 30 months (median 9.2 months; data were available in 120 patients). Seventeen patients (6.3%) lost the ability to sit unaided at an age of 9 months to 67 years of age (mean 15 years; data were available in 11 patients). Nine patients (3.3%) did not achieve independent sitting.
Independent walking was achieved at ages ranging from 8 months 10.5 years (median 14 months; data were available in 125 patients). Forty-two patients (15.7%) did not attain the ability to walk without support.
Ambulation
Out of 226 patients who achieved independent walking, 75 (33.1%) eventually lost this function at ages ranging from 13 months to 57 years (median 21.2 years; information on age at walking loss was available in 62 patients). The age at which the ability to walk was lost is illustrated as a Kaplan–Meier curve in Fig. 2A. Thirty-nine patients (14.5%) used a wheelchair part-time, and full-time wheelchair use was reported by 106 patients (39.5%). Figure 2B displays ambulation as a function of age for the entire cohort, considering those who did not achieve independent walking (upper, pale blue shading). The time between "age at symptom onset" and "loss of ambulation" ranged from 24 months to 51 years, with a median of 17 years.
A Kaplan–Meier curve for loss of walking ability. By the age of 54, 32.5% of our cohort had lost their ability to walk without assistance. Note: For 20% of patients in this study cohort who lost independent ambulation, the exact age is unknown. Accordingly, 20% of the patients who were still able to walk were subtracted to create this curve. B Ambulation as a function of age for the entire cohort. Missing values were estimated from all known values
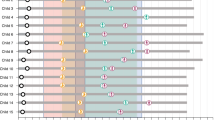
Motor scores
Baseline values for the motor scales "HFSME" (Hammersmith Functional Motor Scale Extended), "RULM" (Revised Upper Limb Assessment), and "6MWT" (6-Minute Walk Test) were available for 230 patients (HFSME), 241 patients (RULM), and 122 patients (6MWT). The results are depicted as scatter plots and box plots (the latter grouped in decades) in Fig. 3. It can be assumed that for both HFSME and RULM, that full scores are expected from the age of six onwards. Reference values for advanced age, where a physiological decline in scores might be expected, do not exist. Reference values for the 6MWT, compiled from a study on healthy populations [25] are shaded in a grey area on the chart.
Results of the motor function tests in Baseline. The wide variability of the disease independent of age is evident, with patients ranging from severely to mildly affected in all age groups up to 69 years. It can be assumed for both HFSME and RULM, that full scores are expected from the age of six onwards. Reference values for the 6MWT are shaded in a grey area on the chart
Scoliosis/scoliosis surgery
114 patients (42.8%; information available in 266 patients) had scoliosis. Scoliosis surgery had been performed on 28 (10.4%; information available for all patients).
Correlation of scoliosis (surgery) and age of symptom onset
Patients who underwent scoliosis surgery experienced symptom onset between 1 month and 5.5 years (median 12.5 months). The age at symptom onset for all scoliosis patients had a median of 1.6 years and a mean of 3.6 years. Among the 147 patients with symptom onset within the first 36 months of age, 83 (57%) had scoliosis.
Tube feeding
Three of the patients (1.1%) utilized a gastric or nasal feeding tube. The age at the initiation of tube feeding was 6.8, 7.3, and 28.9 years, respectively.
Ventilation
Seventeen patients (6.3%) received non-invasive ventilation. The onset of ventilation ranged from 8 months to 49.8 years (median 19.8 years, mean 23.0 years).
Correlation between motor function and ventilator use
Among the 17 ventilated patients, five learned to walk independently, but four of them subsequently lost this ability. Additionally, one of them also lost the ability to sit unaided. In contrast, among the 12 ventilated patients who never acquired the ability to walk independently, one also lost the ability to sit unaided. Conversely, among the 42 patients who never achieved independent walking, 30 did not require ventilation.
Discussion
The natural history of SMA in individuals with four copies of SMN2 remains less well understood than in other types of SMA. However, there is a widely accepted consensus that emphasizes the paramount importance of early detection and treatment of SMA, regardless of SMN2 copy number, to improve overall outcomes. In Europe, treatment options for SMA patients with four SMN2 copies include SMN-targeted therapies such as nusinersen and risdiplam, both of which have been shown in clinical trials to increase SMN protein levels and improve motor function. However, there is a lack of consensus regarding the optimal timing for initiating drug therapy in pre-symptomatic patients with four copies of SMN2. In addition, there is an ongoing debate about the potential scenario in which SMA does not manifest until adulthood, potentially avoiding years of unnecessary treatment [22].
The study aims to address the existing ambiguities in determining treatment indications for individuals with higher SMN2 copy numbers, primarily due to the paucity of long-term data in this context. To address this knowledge gap, we present a robust dataset derived from an extensive cohort of patients with SMA, specifically characterised by the possession of four copies of the SMN2 gene. We performed a standardised query of the SMA Registry of the D-A-CH Region, which now includes more than 1600 patients. 268 patients with 4 copies of SMN2 met the inclusion criteria and could be analysed.
Our findings not only support but also refine the prevailing assumption that the phenotypic diversity among individuals with four copies of SMN2 is remarkably large. In particular, our assessment of motor function at different ages highlights the substantial individual heterogeneity observed in the motor abilities of these patients.
However, perhaps the most important finding of this study is the age of symptom onset (Fig. 1). In our large cohort of symptomatic patients, the median age of onset was only 3 years. In more than half of the cohort, the first symptoms occurred before the age of 3 years. By the age of 18, about 95% of patients with four copies of SMN2 were affected by the disease. Of course, this number must be treated with caution, as people with very little or no symptoms would not be included in the registry. Nevertheless, these data support the proposal of the Independent Expert Commission 2020 [24] to discuss the timing of drug treatment after pre-symptomatic diagnosis. Our data suggest that in the majority of patients with 4 copies of SMN2, the amount of SMN protein is insufficient to prevent motor neuron damage in the long term. As SMN production is highest in early life [26], early initiation of therapy in infancy may be appropriate to prevent motor neuron death if the diagnosis is made at a pre-symptomatic stage [24].
This is supported by the fact that in terms of loss of ambulation, as shown in Fig. 2, almost a third of the cohort lost their previously achieved ability to walk independently. Looking at the age at which this loss of ambulation occurred, there was, as expected, a wide age range with a distribution that is relatively uniform. This observation largely confirms the findings documented in the comprehensive review by Wirth et al. in 2021 [27] and the recent study by Ricci et al., who found an overall risk of walking loss of 35% in their cohort of SMA types 3 and 4 [16]. The time between "age at symptom onset" and "loss of ambulation" also showed a large variation.
In terms of ventilatory support, the prevalence of patients requiring non-invasive ventilation among those with four SMN2 copies was relatively small. Of course, the absence of ventilation does not exclude respiratory muscle involvement (data on vital capacity were not available at baseline), but this suggests that the disease course associated with four copies of SMN2 may have a comparatively milder effect on the respiratory musculature compared to patients with a lower copy number. However, an additional explanation for this "lower respiratory prevalence" could be due to the gradual progression of symptoms, with patients adapting their daily activities and not actively reporting respiratory problems. It may also be due to increased "medical awareness" within the healthcare community, which is now more vigilant than in previous years in monitoring and treating any co-morbidities associated with SMA [28].
Scoliosis was present in 42% of our patients, whereas the prevalence of scoliosis in the otherwise healthy population is only about 2–4%. However, only one quarter of scoliosis patients required spinal surgery. As almost all patients with SMA type 2 develop scoliosis in early childhood [29], we correlated the age of symptom onset in our patient cohort with the presence of scoliosis. Indeed, in patients who underwent scoliosis surgery, symptoms appeared between the ages of 1 month and 5.5 years. Looking at the age at symptom onset for all patients with scoliosis, the median/mean is 1.6/3.6 years, which is significantly lower than in the overall cohort. It is therefore plausible that early onset SMA with 4 SMN2 copies is associated with an increased risk of severe scoliosis. To investigate this further, we looked at the subgroup with disease onset up to 36 months of age. Among them, 56% had scoliosis, which was higher than the overall rate of 43%, but not as high as in the type 2 population. In addition, the proportion of patients in our cohort who did not achieve independent walking exceeded the known range for SMA type 2 patients with 4 SMN2 copies [30]. It can therefore be concluded that the "old classification", which has gradually been abandoned and is now more often referred to as "sitter" or "walker", does not accurately represent the types of SMA and that there is a certain continuum between type 2 and type 3, even among 4 SMN2 copies.
Our clinical data reflect the severe consequences of SMN deficiency in SMA even with 4 SMN2 copies. The overall picture is one of an aggressive disease with an early onset and a high number of wheelchair-bound patients, with a very broad phenotypic spectrum. This broad spectrum, which is also known in SMA with 3 SMN2 copies, is still poorly understood. One reason may be that there is no guarantee that all the SMN2 copies found are able to produce SMN protein. Certainly, siblings with different SMA phenotypes and identical SMN2 copy number and markers have been described, suggesting that the genetic background around the SMA locus alone is not sufficient to explain the phenotypic variability [31, 32]. However, it is possible that one or more copies are defective [33]. Several SMN2 variants have been identified that are associated with milder phenotypes [34,35,36,37], but less is known about SMN2 variants that lead to more severe SMA phenotypes or whether certain SMN2 variants are associated with a weaker response to mRNA treatment. Sequential analysis of individual SMN2 copies is not yet established in routine diagnostics and, unlike other potential genetic modifiers, has not been sufficiently studied to determine its validity.
However, individual patients with 4 copies of SMN2 who remained asymptomatic over a long period of life have been published. There has been no significant increase in similar reports over the years, suggesting that this phenomenon may be rare. Unfortunately, there are no known modifiers that can be routinely tested to predict progression, which makes counselling families with SMA and 4 SMN2 copies diagnosed through a newborn screening program very difficult. In general, the value of electrophysiology, such as EMG to detect denervation/re-innervation, or the Motor Unit Number Index MUNIX, which has been shown to be feasible in children after the age of 5 in proximal muscles in older children [38, 39], can be helpful in making treatment decisions. However, these are invasive procedures that are increasingly unavailable in paediatric treatment centres and are, therefore, more theoretical (also reflected in the fact that almost no electrophysiological data from our patient cohort are recorded in the registry). Of course, therapy indication must be weighed against the potential risks (e.g. long-term intrathecal therapy or the short observation period of oral small-molecule therapy). But given that once damaged, motor neurons do not regenerate and therefore any form of SMA should be treated strictly pre-symptomatically, the data from this study support a proactive approach, despite uncertainty about the expected course of the disease.
Our data also support the value of detecting SMA with 4 SMN2 copies in newborn screening. The goal of newborn screening is to diagnose patients at a pre-symptomatic stage, before the onset of motor neuron disease. Failure to report pathological findings in children with 4 copies puts patients at risk of developing severe forms of SMA. Therefore, the results of our studies call for surveillance programmes of asymptomatic gene carriers aimed at detecting early signs of disease, which may include neurochemical markers.
Limitations
There is a potential bias in the determination of the SMN2 copy number, as we know that especially the older determinations of the SMN2 copy number can be very inaccurate. It is therefore possible that not all patients have the correct copy number and that some patients with three copies may have been included, which was shown in the recent work by Ricci et al. to be 10% in their 4 SMN2 copy cohort [16]. However, the observation that only 6.3% are ventilator dependent suggests that the substantial subset of patients with early motor symptoms from infancy have not been inadvertently included due to an incorrect copy number.
Another limitation is to consider is that individuals with minimal or no symptoms may not have received a diagnosis, potentially resulting in their under-representation in the registry. However, this limitation is mitigated by the fact that the overall prevalence of 4 SMN2 copies in the registry is currently 23%, which is consistent with recent incidences reported in new-born screening projects that do not miss cases of homozygous SMN1 deletion [40].
In Fig. 2B, it has not been taken into account that the observation period varies from patient to patient. The youngest patients are only seven years old, so some will lose their ability to walk in the future—this is not reflected in the graph.
Conclusion
The early onset of symptoms in our cohort, coupled with the expected wide clinical variability, strongly supports the characterization of SMA in individuals with four SMN2 copies as primarily a childhood disease. In particular, more than half of our cohort had their first symptoms before the age of 36 months and almost 95% of patients were affected by the disease by the age of 18 years. These findings must be taken into account when considering the feasibility of a watchful waiting approach to SMA therapy. Our data strongly support a proactive stance involving early initiation of treatment in this subset of SMA patients, particularly if a pre-symptomatic diagnosis is made.
Data availability
Detailed data are available from the SMArtCARE registry or from the corresponding author’s institutions, upon reasonable request.
Abbreviations
- SMA:
-
Spinal muscular atrophy
- SMN:
-
Survival motor neuron
- 6MWT:
-
Six-minute walk test
- RULM:
-
Revised upper limb module
- HFSME:
-
Hammersmith functional motor scale expanded
References
Burghes AH, Beattie CE (2009) Spinal muscular atrophy: why do low levels of survival motor neuron protein make motor neurons sick? Nat Rev Neurosci 10(8):597–609
Pellizzoni L, Yong J, Dreyfuss G (2002) Essential role for the SMN complex in the specificity of snRNP assembly. Science 298(5599):1775–1779
Verhaart IEC et al (2017) Prevalence, incidence and carrier frequency of 5q-linked spinal muscular atrophy - a literature review. Orphanet J Rare Dis 12(1):124
Lefebvre S et al (1995) Identification and characterization of a spinal muscular atrophy-determining gene. Cell 80(1):155–165
Lorson CL et al (1999) A single nucleotide in the SMN gene regulates splicing and is responsible for spinal muscular atrophy. Proc Natl Acad Sci U S A 96(11):6307–6311
Wirth B, Garbes L, Riessland M (2013) How genetic modifiers influence the phenotype of spinal muscular atrophy and suggest future therapeutic approaches. Curr Opin Genet Dev 23(3):330–338
Finkel RS et al (2017) Treatment of infantile-onset spinal muscular atrophy with nusinersen: a phase 2, open-label, dose-escalation study. Lancet 388(10063):3017–3026
Mercuri E et al (2018) Nusinersen versus sham control in later-onset spinal muscular atrophy. N Engl J Med 378(7):625–635
Mendell JR et al (2017) Single-Dose gene-replacement therapy for spinal muscular atrophy. N Engl J Med 377(18):1713–1722
Strauss KA et al (2022) Onasemnogene abeparvovec for presymptomatic infants with three copies of SMN2 at risk for spinal muscular atrophy: the Phase III SPR1NT trial. Nat Med 28(7):1390–1397
Darras BT et al (2021) Risdiplam-treated infants with type 1 spinal muscular atrophy versus historical controls. N Engl J Med 385(5):427–435
Pechmann A, Kirschner J (2017) Diagnosis and new treatment avenues in spinal muscular atrophy. Neuropediatrics 48(4):273–281
Maggi L et al (2022) Adults with spinal muscular atrophy: a large-scale natural history study shows gender effect on disease. J Neurol Neurosurg Psychiatry 93(12):1253–1261
Jedrzejowska M et al (2008) Unaffected patients with a homozygous absence of the SMN1 gene. Eur J Hum Genet 16(8):930–934
Wirth B et al (2006) Mildly affected patients with spinal muscular atrophy are partially protected by an increased SMN2 copy number. Hum Genet 119(4):422–428
Ricci M et al (2023) Clinical phenotype of pediatric and adult patients with spinal muscular atrophy with four smn2 copies: are they really all stable? Ann Neurol 94:1126
Blaschek A et al (2022) Newborn screening for SMA - can a wait-and-see strategy be responsibly justified in patients with four SMN2 copies? J Neuromuscul Dis 9(5):597–605
Kariyawasam DST et al (2020) The implementation of newborn screening for spinal muscular atrophy: the Australian experience. Genet Med 22(3):557–565
Kraszewski JN et al (2018) Pilot study of population-based newborn screening for spinal muscular atrophy in New York state. Genet Med 20(6):608–613
Gailite L et al (2022) New-born screening for spinal muscular atrophy: results of a latvian pilot study. Int J Neonatal Screen 8(1):15
Muller-Felber, W., et al., Newbornscreening SMA - From Pilot Project to Nationwide Screening in Germany. J Neuromuscul Dis, 2022.
Muller-Felber W et al (2020) Infants diagnosed with spinal muscular atrophy and 4 SMN2 copies through newborn screening - opportunity or burden? J Neuromuscul Dis 7(2):109–117
Glascock J et al (2018) Treatment algorithm for infants diagnosed with spinal muscular atrophy through newborn screening. J Neuromuscul Dis 5(2):145–158
Glascock J et al (2020) Revised recommendations for the treatment of infants diagnosed with spinal muscular atrophy via newborn screening who have 4 copies of SMN2. J Neuromuscul Dis 7(2):97–100
Casanova C et al (2011) The 6-min walk distance in healthy subjects: reference standards from seven countries. Eur Respir J 37(1):150–156
Ramos DM et al (2019) Age-dependent SMN expression in disease-relevant tissue and implications for SMA treatment. J Clin Invest 129(11):4817–4831
Wirth B (2021) Spinal muscular atrophy: in the challenge lies a solution. Trends Neurosci 44(4):306–322
Leibrock B et al (2023) Areas of improvement in the medical care of SMA: evidence from a nationwide patient registry in Germany. Orphanet J Rare Dis 18(1):32
Mullender M et al (2008) A Dutch guideline for the treatment of scoliosis in neuromuscular disorders. Scoliosis 3:14
Calucho M et al (2018) Correlation between SMA type and SMN2 copy number revisited: an analysis of 625 unrelated Spanish patients and a compilation of 2834 reported cases. Neuromuscul Disord 28(3):208–215
Cusco I et al (2006) SMN2 copy number predicts acute or chronic spinal muscular atrophy but does not account for intrafamilial variability in siblings. J Neurol 253(1):21–25
Jones CC et al (2020) Spinal muscular atrophy (SMA) subtype concordance in siblings: findings from the cure SMA cohort. J Neuromuscul Dis 7(1):33–40
Chen X et al (2023) Comprehensive SMN1 and SMN2 profiling for spinal muscular atrophy analysis using long-read PacBio HiFi sequencing. Am J Hum Genet 110(2):240–250
Prior TW et al (2009) A positive modifier of spinal muscular atrophy in the SMN2 gene. Am J Hum Genet 85(3):408–413
Vezain M et al (2010) A rare SMN2 variant in a previously unrecognized composite splicing regulatory element induces exon 7 inclusion and reduces the clinical severity of spinal muscular atrophy. Hum Mutat 31(1):E1110–E1125
Wu X et al (2017) A-44G transition in SMN2 intron 6 protects patients with spinal muscular atrophy. Hum Mol Genet 26(14):2768–2780
Ruhno C et al (2019) Complete sequencing of the SMN2 gene in SMA patients detects SMN gene deletion junctions and variants in SMN2 that modify the SMA phenotype. Hum Genet 138(3):241–256
Neuwirth C, Weber M (2020) MUNIX in children with spinal muscular atrophy: an unexpected journey. Muscle Nerve 62(5):565–566
Mendonca RH et al (2021) Motor unit number index (MUNIX) in children and adults with 5q-spinal muscular atrophy: variability and clinical correlations. Neuromuscul Disord 31(6):498–504
Vill K et al (2021) Newborn screening for spinal muscular atrophy in Germany: clinical results after 2 years. Orphanet J Rare Dis 16(1):153
Acknowledgements
We would like to express our gratitude to all the patients and their families who generously shared their data through the SMArtCARE registry. Additionally, we extend our sincere appreciation to all the participating centers in Germany, Austria, and Switzerland for their valuable contributions. AP received support from the Berta-Ottenstein Clinician Scientist Program at the University of Freiburg. HL acknowledges funding from the Canadian Institutes of Health Research (Foundation Grant FDN-167281), the Canadian Institutes of Health Research and Muscular Dystrophy Canada (Network Catalyst Grant for NMD4C), the Canada Foundation for Innovation (CFI-JELF 38412), and the Canada Research Chairs program (Canada Research Chair in Neuromuscular Genomics and Health, 950-232279).
SMArtCARE study group: Wolfgang Löscher, Pascal Martin, Gerd Meyer zu Hörste, Imke Rathmann, Dorothee Schäfer, Elisabeth Steiner, Johannes Stoffels, Julia Bellut, Benedikt Becker, Isabell Cordts, Iris Hannibal, Maren Nitzsche, Therese Well, Birgit Warken, Elisabeth Rothenfusser, Veronika Pilshofer, Kathrin Mörtlbauer, Elke Pernegger, Ana Elmecker, Tanja Neimair, Verena Angermair, Daniela Berg, Maike Tomforde, Fiona Zeiner, Mika Rappold, Alexandra Ille, Magdalena Gosk-Tomek, Anna Wiesenhofer, Katia Vettori, Anna Hüpper, Theresa Stadler, Tabea Reinhardt, Michael Zemlin, Sabine Hettrich, Paul Lingor, Luisa Semmler, Gerrit Machetanz, Dorothea Holzwarth, Stephanie Geitmann, Gabriel Dworschak, Franziska Busch, Ute Baur, Marion Richmann, Barbara Fiedler, Timo Deba, Eva Johann to Settel, Katja Köbbing, Heymut Omran, Hélène Guillemot, Stefan Kappel, Kyriakos Martakis, Tascha Gehrke, Lisa Quinten, Andrea Hackemer, Lena Ruß, Omar Atta, Annina Lang, Benjamin Stolte, Svenja Brakemeier, Andreas Thimm, Jaqueline Lipka, Melina Schlag, Doris Roland-Schäfer, Nadja Kaiser, Andrea Bevot, Eva Jansen, Hanna Küpper, Birgit Meßmer, Hans Hartmann, Barbara Ramadan, Sophie Fischer, Mohamad Tareq Muhandes, Tobias Baum, Adela Della-Marina, Andrea Gangfuß, Britta Holtkamp, Barbara Andres, Isabelle Renger, Steffen Naegel, Ilka Schneider, Thomas Kendzierski, Anna Koelsch, Brigitte Brauner, Christine Leypold, Nathalie Braun, Zylfie Dibrani, Jasmin Bischofberger, Bogdan Bjelica, Camilla Wohnrade, Tilman Riesmeier, Michaela Schwippert, Antonia Leinert, Alma Oscmanovic, Olivia Schreiber-Katz, Daniela Angelova-Toshkina, Lisa Jung, Maja von der Hagen, Jens Schallner, Susan Fiebig, Sandy Foerster, Nicole Claus, Ilka Lehnert, Julie Hammer, Bettina Behring, Stephanie Schüssler, Arpad von Moers, Klaus Goldhahn, Lea Seeber, Daniela Zeisler, Kathrin Bühner, Mike Grünwedel, Katharina Müller-Kaempfer, Anne Güttsches, Melanie Roeder, Irene Lange, Corinna Stoltenburg, Joanna Schneider, Alexandra Wagner, Annette George, Vladimir Dukic, Angela M. Kaindl, Lieske van der Stam, Peter Reilich, Miriam Hiebeler, Federica Montagnese, Simone Thiele, Anna Hagenmeyer, Laura Grimm, Corinna Wirner-Piotrowski, Georg Friedrich Hoffmann, Stefan Kölker, Afshin Saffari, Moritz Niesert, Sabine Specht, Annegret Hoevel, Anke Bon, Petra Müller, Peter Vollmann, Ina Krahwinklergartz, Maren Freigang, Hanna Sophie Lapp, Isabelle Dittes, Maria Wessel, Zeljko Uzelac, Simon Witzel, Johannes Dorst, Joachim Schuster, Kurt Wollinsky, Annekathrin Roediger, Uta Smesny, Almut Fritsch, Nadin Fedtke, Nicole Berberich, Marcel Mann-Richter, Heidi Rochau-Trumpp, Marion Schnurr, Guido Stocker, Wolfgang Wick.
Funding
Open Access funding enabled and organized by Projekt DEAL. Biogen, Roche and Novartis provided financial support for the registry. Data collection and analysis was carried out by the academic SMArtCARE network independent of the commercial partner.
Author information
Authors and Affiliations
Author notes
First and last authors, as well as several of the co-authors are members of the European Reference Network for Neuromuscular Diseases (ERN EURO-NMD).
Consortia
Corresponding author
Ethics declarations
Conflict of interest
AB has received travel expenses and speaker fees from Roche, Novartis, Sanofi Genzyme, Biogen and Santhera. AH has received speaker fees and honoraria for advisor activities from Biogen, Roche, and Novartis Gene Therapies, and research grants from Novartis Gene Therapies. AL is a member of Advisory Boards of Roche Pharma AG, Biogen, Alector and Amylyx. He received compensation for talks from Biologix, the German Society of Neurology, Biogen, Springer Medicine, Amylyx and the company Streamed Up! GmbH. He is involved in trials which are sponsored by Amylyx, Ferrer International, Novartis Research and Development, Mitsubishi Tanabe, Apellis Pharmaceuticals, Alexion, Orion Pharma, the European Union, BMBF, Biogen and Orphazyme, Ionis Pharmaceuticals, QurAlis and Alector. AM has received advisory board honoraria from Hormosan and Sanofi, outside of the submitted work. AP received compensation for advisory boards, training activities and research grants from Novartis and Biogen. AR received honoraria as speaker from Amylyx Pharmaceuticals and as consultant in advisory boards from Biogen and Argenx. RS received honoraria as speaker from ITF Pharma. AZ received compensation for advisory boards and speaker fees from Biogen, Novartis and Roche. He received research compensation from Biogen. CDW has received honoraria from Biogen as an advisory board member and for lectures and as a consultant and advisory board member from Hoffmann‑La Roche. She also received travel expenses from Biogen. CK has received compensation for advisory boards and speaker honoraria from Biogen, Roche and Ipsen, and unrestricted travel grants from Merz and Ipsen, outside of the submitted work. CN has received personal fees from Biogen and Hoffmann–La Roche outside of the submitted work for advisory boards. CW has received honoraria for advisory boards and presentations and travel expenses from Biogen, Avexis/Novartis and Roche. DZ received compensation from Biogen for participation on advisory boards, from Novartis for consultancy work, and travel compensation from Angelini Pharma outside of the submitted work. GMzH received compensation for serving on scientific advisory boards (Alexion, Roche, LFB, Immunovant) and speaker honoraria (Alexion, LFB). He has received scientific project funding from Biogen and Merck. GW has received advisory board honoraria and speaker fees from Alnylam, Biogen, Hormosan, Pfizer and Sobi outside of the submitted work. HK is serving on a scientific advisory board for Avexis and received travel expenses and speaker honoraria from Biogen, Pfizer, Roche, and Sanofi-Aventis. JJ received compensation for advisory boards and funding for travel or speaker honoraria from Avexis/Novartis, Biogen, ITF, Roche, PTC, Pfizer and Sarepta Therapeutics. JK received compensation for research and/or educational and consultancy activities from Biogen, Avexis/Novartis, Roche and Scholar Rock. KV has received received honoraria as an advisory board member, travel expenses and speaker fees from Biogen, Santhera, Orchard, ITF and Novartis. MB received compensation for advisory boards and speakers honoraria from Novartis, Biogen and Roche. MCW received speaker fees and compensation for advisory boards and consultancy activities from Biogen, Avexis/Novartis, Roche. MD has received personal fees as speaker/consultant from Biogen and Roche. MFB has received consultant fees from Biogen, Novartis and Hoffmann-La Roche and Biogen. MG has received an advisory board honorarium from Hoffmann-La Roche and a speaker fee from Novartis outside of the submitted work. MS received compensation for advisory boards from Roche, Eisai and Takeda. MW received advisory board and consultant honoraria from Biogen and Hoffmann-La Roche, and speaker honoraria and travel support for conference attendance from Biogen, outside of the submitted work. OS has served as a member of a scientific advisory board for Avexis and received travel expenses and speaker fees from Biogen. RT received speaker fees and compensation for advisory boards from Biogen, Roche, and PTC. SI received compensation for advisory board and speakers honoraria from Novartis and Roche. SG received consulting fees and speaker fees from Novartis. SP has received speaker fees, non-financial support and research support from Biogen, Roche, AL-S Pharma, Amylyx, Cytokinetics, Ferrer, ITF-Pharma, Zambon, PTC and Sanofi and served on advisory boards of Amylyx, Biogen, Roche, Zambon and ITF Pharma and research grants from the German Neuromuscular Society (DGM) and Neurodegenerative Research outside of the submitted work. TH received compensation for advisory boards, speaker fees and research grants from Roche, Novartis and Biogen. US has served as a member of a scientific advisory board and data safety monitoring board for Biogen, Avexis and Novartis and received speaker fees from Biogen, Avexis, PTC and Sanofi-Aventis. VH received compensation for advisory boards from Avexis/Novartis and Biogen. WMF has served as a member of a scientific advisory board for Biogen, Avexis, PTC, Sarepta, Sanofi-Aventis, Roche and Cytokinetics and received travel expenses and speaker fees from Biogen, Avexis, Novartis, PTC, Roche, Sarepta and Sanofi-Aventis.
Ethical approval
For the SMArtCARE registry, central ethics approval was obtained by the Ethics committee of the University of Freiburg (EK-Freiburg 56/18), and local ethics approvals were obtained from all participating centers. SMArtCARE is registered in the German Clinical Trials Registry (DRKS00012699).
Consent for publication
Informed consent for prospective follow-up and publication was obtained from the participating families.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vill, K., Tacke, M., König, A. et al. 5qSMA: standardised retrospective natural history assessment in 268 patients with four copies of SMN2. J Neurol 271, 2787–2797 (2024). https://doi.org/10.1007/s00415-024-12188-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12188-5