Abstract
The diagnostic criteria of menstrual migraine (MM), migraine related to menstruation and pure menstrual migraine, are placed in the appendix of the International Classification of Headache Disorders and are still primarily considered as research criteria that need validation. Although there is a great wealth of knowledge about the neurobiological processes underlying MM and its symptoms, the mechanisms by which an attack starts during the menstrual cycle remain baffling, and the disease is still undertreated. In this narrative review, we aim to summarize recent data on pathophysiology, epidemiology, burden of disease and treatment of MM. The vast majority of the literature focuses on the relationship between MM and hormonal factors. The role of falling in estrogen levels is believed to increase the susceptibility of blood vessels to prostaglandins, which have been implicated in neurogenic inflammation. Moreover, fluctuations of ovarian steroid hormone levels modulate calcitonin gene-related peptide in the trigeminovascular system. In addition, it has been observed that gonadal hormones modulate cortical spreading depression susceptibility in animal models. Sex hormone influences on MM affect not only the frequency and severity of headache attack but also its treatment. Understanding the mechanisms that contribute to neuroendocrine vulnerability in some women and some menstrual cycles may yield possible marker of the disease opening treatment options specifically targeting MM. An increased interest for future research on the subject will further elucidate how to manage this debilitating type of migraine.



Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38:1–211
Couturier EG, Bomhof MA, Neven AK, van Duijn NP (2003) Menstrual migraine in a representative Dutch population sample: prevalence, disability and treatment. Cephalalgia 23:302–308
Granella F, Sances G, Allais G, Nappi RE, Tirelli A, Benedetto C, Brundu B, Facchinetti F, Nappi G (2004) Characteristics of menstrual and nonmenstrual attacks in women with menstrually related migraine referred to headache centres. Cephalalgia 24:707–716
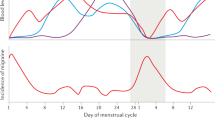
MacGregor EA, Frith A, Ellis J, Aspinall L, Hackshaw A (2006) Incidence of migraine relative to menstrual cycle phases of rising and falling estrogen. Neurology 67:2154–2158
MacGregor EA, Victor TW, Hu X, Xiang Q, Puenpatom RA, Chen W, Campbell JC (2010) Characteristics of menstrual vs nonmenstrual migraine: a post hoc, within-woman analysis of the usual-care phase of a nonrandomized menstrual migraine clinical trial. Headache 50:528–538
Pinkerman B, Holroyd K (2010) Menstrual and nonmenstrual migraines differ in women with menstrually-related migraine. Cephalalgia 30:1187–1194
Vetvik KG, Benth JŠ, MacGregor EA, Lundqvist C, Russell MB (2015) Menstrual versus non-menstrual attacks of migraine without aura in women with and without menstrual migraine. Cephalalgia 35:1261–1268
Classification and Diagnostic Criteria for Headache Disorders, Cranial Neuralgias and Facial Pain (1988) Headache classification committee of the International Headache Society. Cephalalgia 8(Suppl 7):1–96
Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders: 2nd edition. Cephalalgia 24(Suppl 1):9–160
Headache Classification Committee of the International Headache Society (IHS) (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33:629–808
Somerville BW (1972) The role of estradiol withdrawal in the etiology of menstrual migraine. Neurology 22:355–365
Epstein MT, Hockaday JM, Hockaday TD (1975) Migraine and reproductive hormones throughout the menstrual cycle. Lancet 1:543–548
Horth CE, Wainscott G, Neylan C, Wilkinson MI (1975) Proceedings: progesterone, oestradiol and aldosterone levels in plasma during the menstrual cycle of women suffering from migraine. J Endocrinol 65:24P–25P
Martin VT, Wernke S, Mandell K, Ramadan N, Kao L, Bean J, Liu J, Zoma W, Rebar R (2005) Defining the relationship between ovarian hormones and migraine headache. Headache 45:1190–1201
MacGregor EA, Frith A, Ellis J, Aspinall L, Hackshaw A (2006) Prevention of menstrual attacks of migraine: a double-blind placebo-controlled crossover study. Neurology 67:2159–2163
Pavlović JM, Allshouse AA, Santoro NF, Crawford SL, Thurston RC, Neal-Perry GS, Lipton RB, Derby CA (2016) Sex hormones in women with and without migraine: evidence of migraine-specific hormone profiles. Neurology 5(87):49–56
Hassan S, Muere A, Einstein G (2014) Ovarian hormones and chronic pain: a comprehensive review. Pain 155:2448–2460
Downie J, Poyser NL, Wunderlich M (1974) Levels of prostaglandins in human endometrium during the normal menstrual cycle. J Physiol 236:465–472
Moskowitz MA (1984) The neurobiology of vascular head pain. Ann Neurol 16:157–168
Ho TW, Edvinsson L, Goadsby PJ (2010) CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol 6:573–582
Eftekhari S, Warfvinge K, Blixt FW, Edvinsson L (2013) Differentiation of nerve fibers storing CGRP and CGRP receptors in the peripheral trigeminovascular system. J Pain 14:1289–1303
Russell FA, King R, Smillie SJ, Kodji X, Brain SD (2014) Calcitonin gene-related peptide: physiology and pathophysiology. Physiol Rev 94:1099–1142
Antonova M, Wienecke T, Olesen J, Ashina M (2013) Prostaglandins in migraine: update. Curr Opin Neurol 26:269–275
Matsuda M, Huh Y, Ji RR (2019) Roles of inflammation, neurogenic inflammation, and neuroinflammation in pain. J Anesth 33:131–139
Stevenson JC, Macdonald DW, Warren RC, Booker MW, Whitehead MI (1986) Increased concentration of circulating calcitonin gene related peptide during normal human pregnancy. Br Med J (Clin Res Ed) 293:1329–1330
Yallampalli C, Chauhan M, Thota CS, Kondapaka S, Wimalawansa SJ (2002) Calcitonin gene-related peptide in pregnancy and its emerging receptor heterogeneity. Trends Endocrinol Metab 13:263–269
Valdemarsson S, Edvinsson L, Hedner P, Ekman R (1990) Hormonal influence on calcitonin gene-related peptide in man: effects of sex difference and contraceptive pills. Scand J Clin Lab Investig 50:385–388
Gupta P, Harte A, Sturdee DW, Sharma A, Barnett AH, Kumar S, Mc Ternan PG (2008) Effects of menopausal status on circulating calcitonin gene-related peptide and adipokines: implications for insulin resistance and cardiovascular risks. Climacteric 11:364–372
Gupta S, Villalon CM, Mehrotra S, De Vries R, Garrelds IM, Pramod R, Saxena PR, MaassenVanDenBrink A (2007) Female sex hormones and rat dural vasodilatation to CGRP, periarterial electrical stimulation and capsaicin. Headache 47:225–235
Gupta S, Mehrotra S, Villalón C, De Vries R, Garrelds I, Saxena P, Vandenbrink AM (2007) Effects of female sex hormones on responses to CGRP, acetylcholine, and 5-HT in rat isolated arteries. Headache 47:564–575
Ibrahimi K, van Oosterhout WP, van Dorp W, Danser AH, Garrelds IM, Kushner SA, Lesaffre EM, Terwindt GM, Ferrari MD, van den Meiracker AH, MaassenVanDenBrink A (2015) Reduced trigeminovascular cyclicity in patients with menstrually related migraine. Neurology 84:125–131
Sandweiss AJ, Cottier KE, McIntosh MI, Dussor G, Davis TP, Vanderah TW, Largent-Milnes TM (2017) 17-β-Estradiol induces spreading depression and pain behavior in alert female rats. Oncotarget 8:114109–114122
Eikermann-Haerter K, Dileköz E, Kudo C, Savitz SI, Waeber C, Baum MJ, Ferrari MD, van den Maagdenberg Arn MJM, Moskowitz MA, Ayata C (2009) Genetic and hormonal factors modulate spreading depression and transient hemiparesis in mouse models of familial hemiplegic migraine type 1. J Clin Investig 119:99–109
Chauvel V, Multon S, Schoenen J (2018) Estrogen-dependent effects of 5-hydroxytryptophan on cortical spreading depression in rat: modelling the serotonin-ovarian hormone interaction in migraine aura. Cephalalgia 38:427–436
Borsook D, Erpelding N, Lebel A, Linnman C, Veggeberg R, Grant PE, Buettner C, Becerra L, Burstein R (2014) Sex and the migraine brain. Neurobiol Dis 68:200–214
Amandusson A, Hermanson O, Blomqvist A (1995) Estrogen receptor-like immunoreactivity in the medullary and spinal dorsal horn of the female rat. Neurosci Lett 196:25–28
Shughrue PJ, Bushnell CD, Dorsa DM (1992) Estrogen receptor messenger ribonucleic acid in female rat brain during the estrous cycle: a comparison with ovariectomized females and intact males. Endocrinology 131:381–388
Amandusson A, Blomqvist A (2013) Estrogenic influences in pain processing. Front Neuroendocrinol 34:329–349
Sutherland HG, Champion M, Plays A, Stuart S, Haupt LM, Frith A, MacGregor EA, Griffiths LR (2017) Investigation of polymorphisms in genes involved in estrogen metabolism in menstrual migraine. Gene 5(607):36–40
Rodriguez-Acevedo AJ, Smith RA, Roy B, Sutherland H, Lea RA, Frith A, MacGregor EA, Griffiths LR (2014) Genetic association and gene expression studies suggest that genetic variants in the SYNE1 and TNF genes are related to menstrual migraine. J Headache Pain 14(15):62
Pollock CE, Sutherland HG, Maher BH, Lea RA, Haupt LM, Frith A, MacGregor EA, Griffiths LR (2018) The NRP1 migraine risk variant shows evidence of association with menstrual migraine. J Headache Pain 19:31
MacGregor EA, Chia H, Vohrah RC, Wilkinson M (1990) Migraine and menstruation: a pilot study. Cephalalgia 10:305–310
Granella F, Sances G, Zanferrari C, Costa A, Martignoni E, Manzoni GC (1993) Migraine without aura and reproductive life events: a clinical epidemiological study in 1300 women. Headache 33:385–389
Cupini LM, Matteis M, Troisi E, Calabresi P, Bernardi G, Silvestrini M (1995) Sex-hormone-related events in migrainous females. A clinical comparative study between migraine with aura and migraine without aura. Cephalalgia 15:140–144
Vetvik KG, MacGregor EA, Lundqvist C, Russell MB (2010) Self-reported menstrual migraine in the general population. J Headache Pain 11:87–92
Vetvik KG, Macgregor EA, Lundqvist C, Russell MB (2014) Prevalence of menstrual migraine: a population-based study. Cephalalgia 34:280–288
Pavlović JM, Stewart WF, Bruce CA, Gorman JA, Sun H, Buse DC, Lipton RB (2015) Burden of migraine related to menses: results from the AMPP study. J Headache Pain 16:24
Güven B, Güven H, Çomoğlu S (2017) Clinical characteristics of menstrually related and non-menstrual migraine. Acta Neurol Belg 117:671–676
Melhado EM, Thiers Rister HL, Belitardo GA, de Oliveira DR, Buttarello A, Belucio IS, Oliveira Marcos JM, Tonhá Xavier ML, Prieto Peres MF (2019) Allodynia in menstrually related migraine: Score Assessment by Allodynia Symptom Checklist (ASC-12). Headache. https://doi.org/10.1111/head.13677(Epub ahead of print)
Ferreira KS, Guilherme G, Faria VR, Borges LM, Uchiyama AA (2017) Women living together have a higher frequency of menstrual migraine. Headache 57:135–142
Petrovski BÉ, Vetvik KG, Lundqvist C, Eberhard-Gran M (2018) Characteristics of menstrual versus non-menstrual migraine during pregnancy: a longitudinal population-based study. J Headache Pain 19:27
Wang SJ, Fuh JL, Lu SR, Juang KD, Wang PH (2003) Migraine prevalence during menopausal transition. Headache 43:470–478
Nierenburg Hdel C, Ailani J, Malloy M, Siavoshi S, Hu NN, Yusuf N (2015) Systematic review of preventive and acute treatment of menstrual migraine. Headache 55:1052–1071
Bigal M, Sheftell F, Tepper S, Tepper D, Ho TW, Rapoport A (2008) A randomized double-blind study comparing rizatriptan, dexamethasone, and the combination of both in the acute treatment of menstrually related migraine. Headache 48:1286–1293
Allais G, Rolando S, Schiapparelli P, Airola G, Borgogno P, Mana O, Benedetto C (2013) Frovatriptan plus dexketoprofen in the treatment of menstrually related migraine: an open study. Neurol Sci 34:S179–S181
Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T (2009) Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 339:b3914
Carlton C, Banks M, Sundararajan S (2018) Oral contraceptives and ischemic stroke risk. Stroke 49:e157–e159
Sacco S, Merki-Feld GS, Ægidius KL, Bitzer J, Canonico M, Kurth T, Lampl C, Lidegaard Ø, MacGregor EA, MaassenVanDenBrink A, Mitsikostas DD, Nappi RE, Ntaios G, Sandset PM, Martelletti M, European Headache Federation (EHF), the European Society of Contraception, and Reproductive Health (ESC) (2017) Hormonal contraceptives and risk of ischemic stroke in women with migraine: a consensus statement from the European Headache Federation (EHF) and the European Society of Contraception and Reproductive Health (ESC). J Headache Pain 18:108
Warhurst S, Rofe CJ, Brew BJ, Bateson D, McGeechan K, Merki-Field GS, Garrick R, Tomlinson SE (2018) Effectiveness of the progestin-only pill for migraine treatment in women: a systematic review and meta-analysis. Cephalalgia 38:754–764
Burke BE, Olson RD, Cusack BJ (2002) Randomized, controlled trial of phytoestrogen in the prophylactic treatment of menstrual migraine. Biomed Pharmacother 56:283–288
Ferrante F, Fusco E, Calabresi P, Cupini LM (2004) Phyto-oestrogens in the prophylaxis of menstrual migraine. Clin Neuropharmacol 27:137–140
Grazzi L, Egeo G, Calhoun AH, McClure CK, Liebler E, Barbanti P (2016) Non-invasive vagus nerve stimulation (nVNS) as mini-prophylaxis for menstrual/menstrually related migraine: an open-label study. J Headache Pain 17:91
Coffee AL, Sulak PJ, Hill AJ, Hansen DJ, Kuehl TJ, Clark JW (2014) Extended cycle combined oral contraceptives and prophylactic frovatriptan during the hormone-free interval in women with menstrual-related migraines. J Womens Health (Larchmt) 23:310–317
Dima L, Bălan A, Moga MA, Dinu CG, Dimienescu OG, Varga I, Neculau AE (2019) Botulinum toxin a valuable prophylactic agent for migraines and a possible future option for the prevention of hormonal variations-triggered migraines. Toxins (Basel) 11(8):E465. https://doi.org/10.3390/toxins11080465
Ho TW, Ho AP, Ge YJ, Assaid C, Gottwald R, MacGregor EA, Mannix LK, van Oosterhout WP, Koppenhaver J, Lines C, Ferrari MD, Michelson D (2016) Randomized controlled trial of the CGRP receptor antagonist telcagepant for prevention of headache in women with perimenstrual migraine. Cephalalgia 36:148–161
Goadsby PJ, Reuter U, Hallström Y, Broessner G, Bonner JH, Zhang F, Sapra S, Picard H, Mikol DD, Lenz RA (2017) A controlled trial of erenumab for episodic migraine. N Engl J Med 377:2123–2132
Stauffer VL, Dodick DW, Zhang Q, Carter JN, Ailani J, Conley RR (2018) Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol 75:1080–1088
Dodick DW, Silberstein SD, Bigal ME, Yeung PP, Goadsby PJ, Blankenbiller T, Grozinski-Wolff M, Yang R, Ma Y, Aycardi E (2018) Effect of fremanezumab compared with placebo for prevention of episodic migraine: a randomized clinical trial. JAMA 319:1999–2008
Dodick DW, Goadsby PJ, Silberstein SD, Lipton RB, Olesen J, Ashina M, Wilks K, Kudrow D, Kroll R, Kohrman B, Bargar R, Hirman J, Smith J, for the ALD403 study investigators (2014) Safety and efficacy of ALD403, an antibody to calcitonin gene-related peptide, for the prevention of frequent episodic migraine: a randomised, double-blind, placebo-controlled, exploratory phase 2 trial. Lancet Neurol 13:1100–1107
Do TP, Guo S, Ashina M (2019) Therapeutic novelties in migraine: new drugs, new hope? J Headache Pain 20:37. https://doi.org/10.1186/s10194-019-0974-3
Author information
Authors and Affiliations
Contributions
Category 1, (a) conception and design: LMC, IC, PS; (b) acquisition of data: LMC, IC, PS; (c) analysis and interpretation of data: LMC, IC, PS. Category 2, (a) drafting the manuscript: LMC, IC, PS; (b) revising it for intellectual content: LMC, IC, PS. Category 3, (a) final approval of the completed manuscript: LMC, IC, PS.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Rights and permissions
About this article
Cite this article
Cupini, L.M., Corbelli, I. & Sarchelli, P. Menstrual migraine: what it is and does it matter?. J Neurol 268, 2355–2363 (2021). https://doi.org/10.1007/s00415-020-09726-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09726-2