Abstract
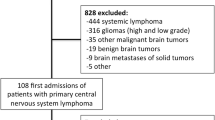
The purpose of this study is to describe the reasons for ICU admission and to evaluate the outcome and prognostic factors of patients with primary malignant brain tumors (PMBT) admitted to the intensive care unit (ICU). This is a retrospective observational cohort study of 196 PMBT patients admitted to two ICUs over a 19-year period. Acute respiratory failure was the main reason for ICU admission (45%) followed by seizures (25%) and non-epileptic coma (14%). Seizures were more common in patients with glial lesions (84 vs. 67%), whereas patients with primary brain lymphoma were more frequently admitted for shock (42 vs. 18%). Overall ICU and 90-day mortality rates were 23 and 50%, respectively. Admission for seizures was independently associated with lower ICU mortality [odds ratio (OR) 0.06], whereas the need for mechanical ventilation (OR 6.85), cancer progression (OR 7.84), respiratory rate (OR 1.11) and Glasgow coma scale (OR 0.85) were associated with higher ICU mortality. Among the 95 patients who received invasive mechanical ventilation, ICU mortality was 37% (n = 35). For these patients, admission for seizures was associated with lower ICU mortality (OR 0.050) whereas cancer progression (OR 7.49) and respiratory rate (OR 1.08) were associated with higher ICU mortality. The prognosis of PMBT patients admitted to the ICU appears relatively favorable compared to that of hematologic malignancies or solid tumors, especially when the patient is admitted for seizures. The presence of a PMBT, therefore, does not appear to be sufficient for refusal of ICU admission. Predictive factors of mortality may help clinicians make optimal triage decisions.



Similar content being viewed by others
References
Soares M, Caruso P, Silva E, Teles JM, Lobo SM, Friedman G et al (2010) Characteristics and outcomes of patients with cancer requiring admission to intensive care units: a prospective multicenter study. Crit Care Med 38:9–15
Puxty K, McLoone P, Quasim T, Kinsella J, Morrison D (2014) Survival in solid cancer patients following intensive care unit admission. Intensive Care Med 40:1409–1428
Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, Afessa B (2011) Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care 1:5
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H et al (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49:1374–1403
Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J et al (2004) Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med 32:2311–2317
Broessner G, Helbok R, Lackner P, Mitterberger M, Beer R, Engelhardt K et al (2007) Survival and long-term functional outcome in 1,155 consecutive neurocritical care patients. Crit Care Med 35:2025–2030
Kiphuth IC, Schellinger PD, Köhrmann M, Bardutzky J, Lücking H, Kloska S et al (2010) Predictors for good functional outcome after neurocritical care. Crit Care 14:R136
Omuro A, DeAngelis LM (2013) Glioblastoma and other malignant gliomas: a clinical review. JAMA 310:1842–1850
Taphoorn MJB, Sizoo EM, Bottomley A (2010) Review on quality of life issues in patients with primary brain tumors. Oncologist 15:618–626
Giovagnoli AR, Silvani A, Colombo E, Boiardi A (2005) Facets and determinants of quality of life in patients with recurrent high grade glioma. J Neurol Neurosurg Psychiatry 76:562–568
Authors (1999) Guidelines for intensive care unit admission, discharge, and triage. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med 27:633–8
Daniels TB, Brown PD, Felten SJ, Wu W, Buckner JC, Arusell RM et al (2011) Validation of EORTC prognostic factors for adults with low-grade glioma: a report using intergroup 86-72-51. Int J Radiat Oncol Biol Phys 81:218–224
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Westphal M, Lamszus K (2015) Circulating biomarkers for gliomas. Nat Rev Neurol 11:556–566
Azoulay E, Mokart D, Pène F, Lambert J, Kouatchet A, Mayaux J et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium-a groupe de recherche respiratoire en réanimation onco-hématologique study. J Clin Oncol 31:2810–2818
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Vaquero J, Martínez R, Manrique M (2000) Stereotactic biopsy for brain tumors: is it always necessary? Surg Neurol 53:432–437
Ferreri AJM, Marturano E (2012) Primary CNS lymphoma. Best Pract Res Clin Haematol 25:119–130
Le Gall JR, Lemeshow S, Saulnier FA (1993) new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H et al (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–980
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Tabouret E, Boucard C, Devillier R, Barrie M, Boussen S, Autran D et al (2016) Neuro-oncological patients admitted in intensive-care unit: predictive factors and functional outcome. J Neurooncol 127:111–117
Arik Y, Leijten FS, Seute T, Robe PA, Snijders TJ (2014) Prognosis and therapy of tumor-related versus non-tumor-related status epilepticus: a systematic review and meta-analysis. BMC Neurol 14:152
Vooturi S, Jayalakshmi S, Sahu S, Mohandas S (2014) Prognosis and predictors of outcome of refractory generalized convulsive status epilepticus in adults treated in neurointensive care unit. Clin Neurol Neurosurg 126:7–10
Vecht CJ, Kerkhof M, Duran-Pena A (2014) Seizure prognosis in brain tumors: new insights and evidence-based management. Oncologist 19:751–759
Roques S, Parrot A, Lavole A, Ancel PY, Gounant V, Djibre M et al (2009) Six-month prognosis of patients with lung cancer admitted to the intensive care unit. Intensive Care Med 35:2044–2050
Soares M, Toffart AC, Timsit JF, Burghi G, Irrazábal C, Pattison N et al (2014) Intensive care in patients with lung cancer: a Multinational Study. Ann Oncol 25:1829–1835
Azoulay E, Thiéry G, Chevret S, Moreau D, Darmon M, Bergeron A et al (2004) The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 83:360–370
Soares M, Darmon M, Salluh JI, Ferreira CG, Thiéry G, Schlemmer B et al (2007) Prognosis of lung cancer patients with life-threatening complications. Chest 131:840–846
Slatore CG, Cecere LM, Letourneau JL, O’Neil ME, Duckart JP, Wiener RS et al (2012) Intensive care unit outcomes among patients with lung cancer in the surveillance, epidemiology, and end results-medicare registry. J Clin Oncol 30:1686–1691
Lemiale V, Mokart D, Resche-Rigon M, Pène F, Mayaux J, Faucher E et al (2015) Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure: a randomized clinical trial. JAMA 314:1711–1719
Newton HB, Newton C, Pearl D, Davidson T (1994) Swallowing assessment in primary brain tumor patients with dysphagia. Neurology 44:1927–1932
Azoulay E, Afessa B (2006) The intensive care support of patients with malignancy: do everything that can be done. Intensive Care Med 32:3–5
Acknowledgements
We are immensely grateful to Professor Jean-Yves Delattre for his valuable comments and strong support. We thank Paul Robinson for his help with English style and grammar.
Author information
Authors and Affiliations
Contributions
Conception and design: Maxens Decavèle, Nicolas Weiss, Isabelle Rivals, Alexandre Demoule. Collection and assembly of data: Maxens Decavèle, Julien Mayaux, Hélène Prodanovic, Alexandre Demoule. Data analysis and interpretation: Maxens Decavèle, Isabelle Rivals, Alexandre Demoule, Thomas Similowski. Manuscript writing: Maxens Decavèle, Alexandre Demoule. Final approval: All authors.
Corresponding author
Ethics declarations
Ethical standards
Consent was not collected because of retrospective design. The study was approved by the Institutional Review Board of the French Intensive Care Society.
Conflicts of interest
Alexandre Demoule has signed research contracts with Covidien, Maquet, Philips and Ait Liquide Santé; he has also received personal fees from Covidien, Maquet and MSD. Ahmed Idbaih reports research funding from La Fondation ARC pour la recherche sur le Cancer, Carthera, Beta-Innov, and Intselchimos; travel funding from Hoffmann-La Roche; and personal fees from Novartis, La Lettre du Cancérologue, BMS, and Cipla unrelated to the submitted work. Nicolas Weiss has signed research contracts with Eumedica, BMS, MedDay pharmaceuticals; he has also received personal fees from Norgine and Alpha-Wasserman. Thomas Similowski has received Grant research from Coviden, Philips, Pierre Fabre Médicaments, Air Liquide Medical Systems; he has also received personal fees from Takeda, Teva Pharma, Lungpacer Inc, Almirall France, Pierre Fabre Médicaments, Novartis, Mundipharma, Invacare, Astra Zeneca, Boehringer Ingelheim and GlaxoSmithKline. Julien Mayaux declares that he has no conflict of interest. Hélène Prodanovic declares that she has no conflict of interest. Isabelle Rivals declares that she has no conflict of interest. Maxens Decavèle declares that he has no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Decavèle, M., Weiss, N., Rivals, I. et al. Prognosis of patients with primary malignant brain tumors admitted to the intensive care unit: a two-decade experience. J Neurol 264, 2303–2312 (2017). https://doi.org/10.1007/s00415-017-8624-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8624-7