Abstract
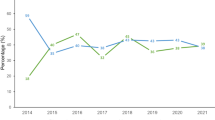
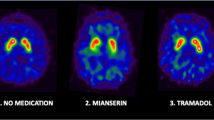
[123I]-FP-CIT is a single photon emission computed tomography (SPECT) ligand showing in vivo the loss of dopaminergic terminals in the brain and is now available in the market. Despite several systematic studies in clinically inconclusive cases, the use of such imaging in clinical routine is scarcely reported. We analyzed 516 files of subjects with movement disorders who were consecutively examined using [123I]-FP-CIT scan and determined whether the use of imaging was appropriate and if it improved clinical diagnosis or care of the patient. In addition, we determined if appropriate use was related to subspecialties in Neurology, e.g., movement disorders’ specialists vs. general neurologists, and if appropriate use was increasing over time. Among the 516 scans, 18 % were in agreement with the license, 62 % were classified as appropriate and 37 % were considered inappropriate. A change of management was obvious in 60 % of patients, but in 92 % of those with an appropriate request vs. 13 % of patients with an inappropriate request. Movement disorders’ specialists had more appropriate requests than other practitioners. Eventually, comparing the first 100 vs. the last 100 quantified SPECT, performed more than 2.5 years apart, we found no difference for the appropriateness of the examination. The use of [123I]-FP-CIT imaging in clinical routine does not fit a restrictive license. An inappropriate use is seen in nearly 40 % of cases, which reduces the real cost-effectiveness of the technique suggesting a need for continuing medical education on the topic.



Similar content being viewed by others
References
Tolosa E, Wenning G, Poewe W (2006) The diagnosis of Parkinson’s disease. Lancet Neurol 5:75–86
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Meara J, Bhowmick BK, Hobson P (1999) Accuracy of diagnosis in patients with presumed Parkinson’s disease. Age Ageing 28:99–102
Sixel-Doring F, Liepe K, Mollenhauer B, Trautmann E, Trenkwalder C (2011) The role of (123)I-FP-CIT-SPECT in the differential diagnosis of Parkinson and tremor syndromes: a critical assessment of 125 cases. J Neurol 258:2147–2154
Benamer TS, Patterson J, Grosset DG et al (2000) Accurate differentiation of parkinsonism and essential tremor using visual assessment of [123I]-FP-CIT SPECT imaging: the [123I]-FP-CIT study group. Mov Disord 15:503–510
Jeon BS, Jeong JM, Park SS et al (1998) Dopamine Transporter Density Measured by[123I]β-CIT ‘Single-Photon Emission Computed Tomography Is Normal in Dopa-Responsive Dystonia. Ann Neurol 43:792–800
Schwingenschuh P, Ruge D, Edwards MJ et al (2010) Distinguishing SWEDDs patients with asymmetric resting tremor from Parkinson’s disease: a clinical and electrophysiological study. Mov Disord 25:560–569
Lorberboym M, Djaldetti R, Melamed E, Sadeh M, Lampl Y (2004) 123I-FP-CIT SPECT Imaging of Dopamine Transporters in Patients with Cerebrovascular Disease and Clinical Diagnosis of Vascular Parkinsonism. J Nucl Med 45:1688–1693
Benaderette S, Zanotti Fregonara P, Apartis E et al (2006) Psychogenic parkinsonism: a combination of clinical, electrophysiological, and [(123)I]-FP-CIT SPECT scan explorations improves diagnostic accuracy. Mov Disord 21:310–317
Lorberboym M, Treves TA, Melamed E, Lampl Y, Hellmann M, Djaldetti R (2006) [123I]-FP/CIT SPECT imaging for distinguishing drug-induced parkinsonism from Parkinson’s disease. Mov Disord 21:510–514
Pirker W, Asenbaum S, Bencsits G et al (2000) [123I]-CIT SPECT in multiple system atrophy, progressive supranuclear palsy, and corticobasal degeneration. Mov Disord 15:1158–1167
Perju-Dumbrava LD, Kovacs GG, Pirker S et al (2012) Dopamine Transporter Imaging in Autopsy-Confirmed Parkinson’s Disease and Multiple System Atrophy. Mov Disord 27(1):65–71
Catafau AM, Tolosa E (2004) Impact of dopamine transporter SPECT using 123I-Ioflupane on diagnosis and management of patients with clinically uncertain Parkinsonian syndromes. Mov Disord 19:1175–1182
Tolosa E, Borght TV, Moreno E (2007) Accuracy of DaTSCAN (123I-Ioflupane) SPECT in diagnosis of patients with clinically uncertain parkinsonism: 2-year follow-up of an open-label study. Mov Disord 22:2346–2351
Antonini A, Berto P, Lopatriello S, Tamma F, Annemans L (2008) And Chambers M. Cost- effectiveness of 123I-FP-CIT SPECT in the differential diagnosis of essential tremor and Parkinson’s disease in Italy. Mov Disord 23:2202–2209
Kas A, Payoux P, Habert MO et al (2007) Validation of a standardized normalization template for statistical parametric mapping analysis of 123I-FP- CIT images. J Nucl Med 48:1459–1467
Lehnert BE (2010) Bree RL; Analysis of Appropriateness of Outpatient CT and MRI Referred From Primary Care Clinics at an Academic Medical Center: how Critical Is the Need for Improved Decision Support? J Am Coll Radiol 7:192–197
Kupsch A, Bajaj N, Weiland F et al (2013) Changes in clinical management and diagnosis following DaTscan™ SPECT imaging in patients with clinically uncertain Parkinsonian syndromes: a 12-week follow-up study. Neurodegener Dis 11:22–32
Van Laere K, Everaert L, Annemans L, Gonce M, Vandenberghe W (2008) Vander Borght T. The cost effectiveness of 123I-FP-CIT SPECT imaging in patients with an uncertain clinical diagnosis parkinsonism. Eur J Nucl Med Mol Imaging 35:1367–1376
Dodel RC, Höffken H, Möller C et al (2003) Dopamine transporter imaging and SPECT in diagnostic work-up of Parkinson’s disease: a decision-analytic approach. Mov Disord 18(Suppl 7):S52–S62
Newman EJ, Breen K, Patterson J, Hadley DM, Grosset KA, Grosset DG (2009) Accuracy of Parkinson’s disease diagnosis in 610 general practice patients in the West of Scotland. Mov Disord 24:2379–2385
Conflict of interest
The authors declare that they have no conflict of interest which could influence the content of the manuscript submitted. However, Emmanuel Itti declares a partnership between GE HealthCare and a non-profit association the 14/01/14. Claire Thiriez declares grants from Boston Scientific for another study, and congress funding from Orkyn, novartis, and Lundbeck-Teva. Gilles Fenelon declares speaker honoraria from Teva Pharma and Lundbeck SAS, and travel funding from Teva Pharma and Lundbeck SAS. Eva Evangelista and Michel Meignan reported no financial disclosure. Pierre Cesaro deceased before giving his financial disclosure. Philippe Remy declares consultancies from Lundbeck, and advisory Boards from Novartis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thiriez, C., Itti, E., Fénelon, G. et al. Clinical routine use of dopamine transporter imaging in 516 consecutive patients. J Neurol 262, 909–915 (2015). https://doi.org/10.1007/s00415-014-7634-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7634-y