Abstract
Neonaticide is defined by the deliberate killing or homicide of a child within 24 h of its birth. In this context, three fundamental questions are generally asked of the forensic pathologist: what is the cause of death of the neonate? Was the child viable (i.e., what is the gestational age of the neonate)? Finally, was the neonate stillborn or liveborn?
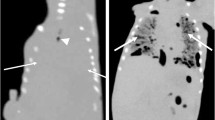
Postmortem imaging can help answer these questions by conducting (1) a complete lesional analysis of the body and the placenta, (2) an estimation of the gestational age by measuring the lengths of the diaphyseal long bones, and (3) an analysis of the aeration of the lungs and intestines. Using the details of 18 cases, we illustrate aspects of neonaticide cases in postmortem computed tomography (PMCT), offering detailed examples of notable postmortem changes and abnormalities, especially in the analysis of the pulmonary parenchyma. This article presents a useful iconography for the radiologist confronted with this rare yet complex forensic situation.












Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
Abbreviations
- CPR:
-
Cardiopulmonary resuscitation
- CT:
-
Computed tomography
- MIP:
-
Maximal intensity projection
- PMCT:
-
Postmortem computed tomography
- WG:
-
Weeks of gestation
References
Grabherr S, Egger C, Vilarino R et al (2017) Modern post-mortem imaging: an update on recent developments. Forensic Sci Res 2:52–64. https://doi.org/10.1080/20961790.2017.1330738
Redaktsiia, Thali M, Dirnhofer R, Vock P (2016) The virtopsy approach. 3D optical and radiological scanning and reconstruction in forensic medicine (CRC Press, Boca Raton, Fl: CRC Press. London NW. 2009). Sud-Meditsinskaya Ekspertiza 59:58. https://doi.org/10.17116/sudmed201659358-62
Baglivo M, Winklhofer S, Hatch GM et al (2013) The rise of forensic and post-mortem radiology—analysis of the literature between the year 2000 and 2011. J Forensic Radiol Imaging 1:3–9. https://doi.org/10.1016/j.jofri.2012.10.003
Shelmerdine SC, Gerrard CY, Rao P et al (2019) Joint European Society of Paediatric Radiology (ESPR) and International Society for Forensic Radiology and Imaging (ISFRI) guidelines: paediatric postmortem computed tomography imaging protocol. Pediatr Radiol 49:694–701. https://doi.org/10.1007/s00247-018-04340-x
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, de Bakker H, van Rijn RR (2014) Postmortem CT compared to autopsy in children; concordance in a forensic setting. Int J Legal Med 128:957–965. https://doi.org/10.1007/s00414-014-0964-6
Krentz BV, Alamo L, Grimm J et al (2016) Performance of post-mortem CT compared to autopsy in children. Int J Legal Med 130:1089–1099. https://doi.org/10.1007/s00414-016-1370-z
Gorincour G, Sarda-Quarello L, Laurent P-E et al (2015) The future of pediatric and perinatal postmortem imaging. Pediatr Radiol 45:509–516. https://doi.org/10.1007/s00247-014-3266-8
OMS (1977) Organisation Mondiale de la Santé. Classification Internationale des maladies, révision 1975, Genève
Guddat SS, Gapert R, Tsokos M, Oesterhelweg L (2013) Proof of live birth using postmortem multislice computed tomography (pmMSCT) in cases of suspected neonaticide: advantages of diagnostic imaging compared to conventional autopsy. Forensic Sci Med Pathol 9:3–12. https://doi.org/10.1007/s12024-012-9361-y
Griest K (2010) Pediatric homicide: medical investigation. CRC Press, Boca Raton
Beauthier J-P (2007) Traité de Médecine Legale, 2ème Edition. de Boeck
GroßeOstendorf A-L, Rothschild MA, Müller AM, Banaschak S (2013) Is the lung floating test a valuable tool or obsolete? A prospective autopsy study. Int J Legal Med 127:447–451. https://doi.org/10.1007/s00414-012-0727-1
Mazuchowski EL, Franco DM, Berran PJ, Harcke HT (2016) The virtual hydrostatic test. Am J Forensic Med Pathol 1. https://doi.org/10.1097/PAF.0000000000000287
Michiue T, Ishikawa T, Kawamoto O et al (2013) Postmortem CT investigation of air/gas distribution in the lungs and gastrointestinal tracts of newborn infants: a serial case study with regard to still- and live birth. Forensic Sci Int 226:74–80. https://doi.org/10.1016/j.forsciint.2012.12.011
Ducloyer M, Tuchtan L, Delteil C et al (2019) Lung density measurement in postmortem computed tomography: a new tool to assess immediate neonatal breath in suspected neonaticides. Int J Legal Med.https://doi.org/10.1007/s00414-019-02103-3
Barber JL, Sebire NJ, Chitty LS et al (2015) Lung aeration on post-mortem magnetic resonance imaging is a useful marker of live birth versus stillbirth. Int J Legal Med 129:531–536. https://doi.org/10.1007/s00414-014-1125-7
Dettmeyer RB (2018) Forensic histopathology: fundamentals and perspectives, 2nd edn. Springer, Berlin Heidelberg, New York
Knight B, Saukko PJ (2004) Knight’s forensic pathology, 3rd ed. Arnold ; Distributed in the United States of America by Oxford University Press, London : New York
Stocker JT, Dehner LP (2001) Pediatric pathology, 2nd edn. Lippincott Williams & Wilkins, Philadelphia
Tsokos M (2007) Forensic pathology reviews, vol 2. Humana Press, Totowa
Sieswerda-Hoogendoorn T, Soerdjbalie-Maikoe V, Maes A, van Rijn RR (2013) The value of post-mortem CT in neonaticide in case of severe decomposition: description of 12 cases. Forensic Sci Int 233:298–303. https://doi.org/10.1016/j.forsciint.2013.09.023
Levy AD, Harcke HT, Mallak CT (2010) Postmortem imaging: MDCT features of postmortem change and decomposition. Am J Forensic Med Pathol 31:12–17. https://doi.org/10.1097/PAF.0b013e3181c65e1a
Egger C, Vaucher P, Doenz F et al (2012) Development and validation of a postmortem Radiological Alteration Index: the RA-Index. Int J Legal Med 126:559–566. https://doi.org/10.1007/s00414-012-0686-6
Reichard R (2008) Birth injury of the cranium and central nervous system: birth injury of the cranium and CNS. Brain Pathol 18:565–570. https://doi.org/10.1111/j.1750-3639.2008.00205.x
Lee SJ, Kim JK, Kim SJ (2018) The clinical characteristics and prognosis of subgaleal hemorrhage in newborn. Korean J Pediatr 61:387–391. https://doi.org/10.3345/kjp.2018.06800
Ojumah N, Ramdhan RC, Wilson C et al2017) Neurological neonatal birth injuries: a literature review. Cureus.https://doi.org/10.7759/cureus.1938
Hughes CA, Harley EH, Milmoe G et al (1999) Birth trauma in the head and neck. Arch Otolaryngol Neck Surg 125:193. https://doi.org/10.1001/archotol.125.2.193
Prabhu SP, Newton AW, Perez-Rossello JM, Kleinman PK (2013) Three-dimensional skull models as a problem-solving tool in suspected child abuse. Pediatr Radiol 43:575–581. https://doi.org/10.1007/s00247-012-2546-4
Martin A, Paddock M, Johns CS et al (2020) Avoiding skull radiographs in infants with suspected inflicted injury who also undergo head CT: “a no-brainer?” Eur Radiol 30:1480–1487. https://doi.org/10.1007/s00330-019-06579-w
Idriz S, Patel JH, AmeliRenani S et al (2015) CT of normal developmental and variant anatomy of the pediatric skull: distinguishing trauma from normality. Radiographics 35:1585–1601. https://doi.org/10.1148/rg.2015140177
Dupuis O, Silveira R, Dupont C et al (2005) Comparison of “instrument-associated” and “spontaneous” obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol 192:165–170. https://doi.org/10.1016/j.ajog.2004.06.035
Nadas S, Reinberg O (1992) Obstetric fractures. Eur J Pediatr Surg 2:165–168. https://doi.org/10.1055/s-2008-1063431
Km J HS (2014) [Neonatal skull fracture]. In: Ugeskr. Laeger. https://pubmed.ncbi.nlm.nih.gov/25347566/?from_term=skull+fracture+newborn&from_pos=4. Accessed 15 Mar 2020
Wobus RE (1925) A pathognomonic sign of intrauterine death. Am J Obstet Gynecol 10:457. https://doi.org/10.1016/S0002-9378(25)90889-7
Silva MET, Oliveira DA, Roza TH et al (2015) Study on the influence of the fetus head molding on the biomechanical behavior of the pelvic floor muscles, during vaginal delivery. J Biomech 48:1600–1605. https://doi.org/10.1016/j.jbiomech.2015.02.032
Ami O, Maran JC, Gabor P et al (2019) Three-dimensional magnetic resonance imaging of fetal head molding and brain shape changes during the second stage of labor. PLoS ONE 14:e0215721. https://doi.org/10.1371/journal.pone.0215721
Arthurs OJ, Barber JL, Taylor AM, Sebire NJ (2015) Normal perinatal and paediatric postmortem magnetic resonance imaging appearances. Pediatr Radiol 45:527–535. https://doi.org/10.1007/s00247-014-3166-y
Smith AB, Lattin GE, Berran P, Harcke HT (2012) Common and expected postmortem CT observations involving the brain: mimics of antemortem pathology. Am J Neuroradiol 33:1387–1391. https://doi.org/10.3174/ajnr.A2966
Sieswerda-Hoogendoorn T, Beenen LFM, van Rijn RR (2015) Normal cranial postmortem CT findings in children. Forensic Sci Int 246:43–49. https://doi.org/10.1016/j.forsciint.2014.10.036
Prayer D, Kasprian G, Krampl E et al (2006) MRI of normal fetal brain development. Eur J Radiol 57:199–216. https://doi.org/10.1016/j.ejrad.2005.11.020
Garel C, Elmaleh M, Chantrel E et al (2003) Fetal MRI: normal gestational landmarks for cerebral biometry, gyration and myelination. Childs Nerv Syst 19:422–425. https://doi.org/10.1007/s00381-003-0767-4
Mohan S, Rogan EA, Batty R et al (2013) CT of the neonatal head. Clin Radiol 68:1155–1166. https://doi.org/10.1016/j.crad.2013.06.011
Whitby E, Griffiths P, Rutter S et al (2004) Frequency and natural history of subdural haemorrhages in babies and relation to obstetric factors. Lancet 363:846–851. https://doi.org/10.1016/S0140-6736(04)15730-9
Kumpulainen V, Lehtola SJ, Tuulari JJ et al (2020) Prevalence and risk factors of incidental findings in brain MRIs of healthy neonates—the FinnBrain Birth Cohort Study. Front Neurol 10.https://doi.org/10.3389/fneur.2019.01347
Proisy M, Loget P, Bouvet R et al (2015) Non-specific post-mortem modifications on whole-body post-mortem computed tomography in sudden unexpected death in infancy. J Forensic Radiol Imaging 3:16–23. https://doi.org/10.1016/j.jofri.2015.02.001
Tindall VR, Scott JS (1965) Placental calcification a study of 3,025 singleton and multiple pregnancies. BJOG Int J Obstet Gynaecol 72:356–373. https://doi.org/10.1111/j.1471-0528.1965.tb01470.x
Jeacock MK, Scott J, Plester JA (1963) Calcium content of the human placenta. Am J Obstet Gynecol 87:34–40. https://doi.org/10.1016/S0002-9378(16)35139-0
Wei SH, Helmy M, Cohen AJ (2009) CT evaluation of placental abruption in pregnant trauma patients. Emerg Radiol 16:365–373. https://doi.org/10.1007/s10140-009-0804-z
Fadl SA, Linnau KF, Dighe MK (2019) Placental abruption and hemorrhage—review of imaging appearance. Emerg Radiol 26:87–97. https://doi.org/10.1007/s10140-018-1638-3
Fadl S, Moshiri M, Fligner CL et al (2017) Placental imaging: normal appearance with review of pathologic findings. Radiographics 37:979–998. https://doi.org/10.1148/rg.2017160155
MacDonald H (2002) Perinatal care at the threshold of viability. Pediatrics 110:1024–1027. https://doi.org/10.1542/peds.110.5.1024
Villar J, Ismail LC, Victora CG et al (2014) International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384:857–868. https://doi.org/10.1016/S0140-6736(14)60932-6
Créquat J, Duyme M, Brodaty G (2000) Biometry 2000. Fetal growth charts by the French College of fetal ultrasonography and the Inserm U 155. Gynecol Obstet Fertil 28:435–445
Collège français d’échographie fœtale (CFEF) (2017) Compte rendu du séminaire de travail du Collège français d’échographie fœtal (CFEF) sur les référentiels et standards de biométrie fœtale. Juin 2017. Gynécol Obstét Fertil Sénologie 45:545–551. https://doi.org/10.1016/j.gofs.2017.08.012
Scheuer L, Black SM (2000) Developmental juvenile osteology. Academic Press, San Diego
Fazekas IG, Kósa F (1978) Forensic fetal osteology. Akadémiai Kiadó, Budapest
Adalian P, Piercecchi-Marti MD, Bourliere-Najean B et al (2001) Postmortem assessment of fetal diaphyseal femoral length: validation of a radiographic methodology. J Forensic Sci 46:215–219
Piercecchi-Marti M-D, Adalian P, Bourliere-Najean B et al (2002) Validation of a radiographic method to establish new fetal growth standards: radio-anatomical correlation. J Forensic Sci 47:328–331
Adalian P, Piercecchi-Marti M-D, Bourlière-Najean B et al (2002) Nouvelle formule de détermination de l’âge d’un fœtus. C R Biol 325:261–269. https://doi.org/10.1016/S1631-0691(02)01426-9
Carneiro C, Curate F, Cunha E (2016) A method for estimating gestational age of fetal remains based on long bone lengths. Int J Legal Med 130:1333–1341. https://doi.org/10.1007/s00414-016-1393-5
Schaefer M, Scheuer L, Black SM (2009) Juvenile osteology: a laboratory and field manual. Elsevier/Academic Press, Amsterdam, Burlington
Graham CB (1972) Assessment of bone maturation–methods and pitfalls. Radiol Clin North Am 10:185–202
Brogdon BG (1998) The scope of forensic radiology. Clin Lab Med 18:203–240. https://doi.org/10.1016/S0272-2712(18)30169-0
Gentili P, Trasimeni A, Giorlandino C (1984) Fetal ossification centers as predictors of gestational age in normal and abnormal pregnancies. J Ultrasound Med 3:193–197. https://doi.org/10.7863/jum.1984.3.5.193
Adair FL, Scammon RE (1921) A study of the ossification centers of the wrist, knee and ankle at birth, with particular reference to the physical development and maturity of the newborn. Am J Obstet Gynecol 2:35–60. https://doi.org/10.1016/S0002-9378(21)90258-8
Naderi S, Bolandgray A, Ardekani MS, Rahimian H (1975) Evaluation of knee joint ossification centers for the assessment of fetal maturity in a developing country. Eur J Obstet Gynecol Reprod Biol 5:167–170. https://doi.org/10.1016/0028-2243(75)90001-5
Thali MJ (2011) Brogdon’s forensic radiology. CRC Press, Boca Raton
Durigon M (2007) Pratique médico-légale. Masson, Issy-les-Moulineaux
Mercer BM, Sklar S, Shariatmadar A et al (1987) Fetal foot length as a predictor of gestational age. Am J Obstet Gynecol 156:350–355. https://doi.org/10.1016/0002-9378(87)90282-1
Adamsbaum C, Rey-Salmon C (2013) Maltraitance chez l’enfant. Médecine sciences publications-Lavoisier, Paris
Resnick PJ (1970) Murder of the newborn: a psychiatric review of neonaticide. Am J Psychiatry 126:1414–1420. https://doi.org/10.1176/ajp.126.10.1414
Vellut N, Cook JM, Tursz A (2012) Analysis of the relationship between neonaticide and denial of pregnancy using data from judicial files. Child Abuse Negl 36:553–563. https://doi.org/10.1016/j.chiabu.2012.05.003
Stenton S, Cohen MC (2020) Assessment of neonaticide in the setting of concealed and denied pregnancies. Forensic Sci Med Pathol. https://doi.org/10.1007/s12024-019-00212-4
Porter T, Gavin H (2010) Infanticide and neonaticide: a review of 40 years of research literature on incidence and causes. Trauma Violence Abuse 11:99–112. https://doi.org/10.1177/1524838010371950
Currarino G (2000) Occipital osteodiastasis: presentation of four cases and review of the literature. Pediatr Radiol 30:823–829. https://doi.org/10.1007/s002470000337
Panda A (2014) Skeletal dysplasias: a radiographic approach and review of common non-lethal skeletal dysplasias. World J Radiol 6:808. https://doi.org/10.4329/wjr.v6.i10.808
Acknowledgements
The authors gratefully acknowledge Doctor Ana Carballeira Alvarez for her availability.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This work has been realised in accordance with the Helsinki Declaration on Medical Research.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• When neonaticide is suspected, the three fundamental forensic questions that must be answered are: what is the cause of death of the neonate? Was the child viable (i.e., what is the gestational age of the newborn)? Was the neonate stillborn or liveborn?
• Postmortem imaging can help answer these questions through (1) a complete lesional analysis of the body and the placenta, (2) an estimation of the gestational age by measuring the lengths of the diaphyseal long bones, and (3) an analysis of the aeration of the lungs and intestines.
• Non-specific postmortem changes must be identified to avoid misinterpretation.
• A relevant radiological analysis of the pulmonary parenchyma is fundamental.
Rights and permissions
About this article
Cite this article
Ducloyer, M., David, A., Dautreme, B. et al. Pictorial review of the postmortem computed tomography in neonaticide cases. Int J Legal Med 135, 2395–2408 (2021). https://doi.org/10.1007/s00414-021-02677-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-021-02677-x