Abstract
Purpose
Exercise-induced bronchoconstriction (EIB) affects approximately 50% of young asthma patients, impairing their participation in sports and physical activities. Eucapnic voluntary hyperpnea (EVH) is an approved surrogate challenge to exercise for objective EIB diagnosis, but the required minimum target hyperventilation rates remain unexplored in this population. This study aimed to evaluate the association between the achieved ventilation rates (VRs) during a challenge and EIB-compatible response (EIB-cr) in young asthma patients.
Methods
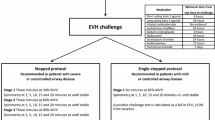
This cross-sectional study included 72 asthma patients aged 10–20 years. Forced expiratory volume in the first second (FEV1) was measured before and 5, 15, and 30 min after the EVH. The target VR was set at 21 times the individual’s baseline FEV1. A decrease of > 10% in FEV1 after the challenge was considered an EIB-cr. The challenge was repeated after 48–72 h in those without an EIB-cr.
Results
Thirty-six individuals had an EIB-cr at initial evaluation. The median VRs achieved was not different between individuals with and without an EIB-cr (19.8 versus 17.9; p = 0.619). The proportion of individuals with an EIB-cr was nor different comparing those who achieved (12/25) or not (24/47) the calculated target VRs (p = 0.804). At the repeated EVH challenge an EIB-cr was observed in 14/36 individuals with a negative response in the first evaluation, with no differences in achieved VRs between the two tests (p = 0.463).
Conclusion
Irrespective of the achieved VR, an EIB-compatible response after an EVH challenge must be considered relevant for clinical and therapeutic judgment and negative tests should be repeated.


Similar content being viewed by others
References
Rabe KF, Adachi M, Lai CK et al (2004) Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol 114:40–47. https://doi.org/10.1016/j.jaci.2004.04.042
Mancuso CA, Sayles W, Robbins L et al (2006) Barriers and facilitators to healthy physical activity in asthma patients. J Asthma 43:137–143. https://doi.org/10.1080/02770900500498584
Velsor-Friedrich B, Vlasses F, Moberley J, Coover L (2004) Talking with teens about asthma management. J Sch Nurs 20:140–148. https://doi.org/10.1177/10598405040200030401
Williams B, Powell A, Hoskins G, Neville R (2008) Exploring and explaining low participation in physical activity among children and young people with asthma: a review. BMC Fam Pract 9:40. https://doi.org/10.1186/1471-2296-9-40
Parsons JP, Hallstrand TS, Mastronarde JG et al (2013) An official American thoracic society clinical practice guideline: exercise-induced bronchoconstriction. Am J Respir Crit Care Med 187:1016–1027. https://doi.org/10.1164/rccm.201303-0437ST
Gotshall RW (2002) Exercise-induced bronchoconstriction. Drugs 62:1725–1739. https://doi.org/10.2165/00003495-200262120-00003
Weiler JM, Anderson SD, Randolph C et al (2010) Pathogenesis, prevalence, diagnosis, and management of exercise-induced bronchoconstriction: a practice parameter. Ann Allergy Asthma Immunol 105:S1–S47. https://doi.org/10.1016/j.anai.2010.09.021
Lang JE (2019) The impact of exercise on asthma. Curr Opin Allergy Clin Immunol 19:118–125. https://doi.org/10.1097/ACI.0000000000000510
Parsons JP, Kaeding C, Phillips G et al (2007) Prevalence of exercise-induced bronchospasm in a cohort of varsity college athletes. Med Sci Sport Exerc 39:1487–1492. https://doi.org/10.1249/mss.0b013e3180986e45
Hallstrand TS, Curtis JR, Koepsell TD et al (2002) Effectiveness of screening examinations to detect unrecognized exercise-induced bronchoconstriction. J Pediatr 141:343–349. https://doi.org/10.1067/mpd.2002.125729
Dantas FMNA, Correia MAV, Silva AR et al (2014) Mothers impose physical activity restrictions on their asthmatic children and adolescents: an analytical cross-sectional study. BMC Public Health 14:1–7. https://doi.org/10.1186/1471-2458-14-287
Parsons JP, Cosmar D, Phillips G et al (2012) Screening for exercise-induced bronchoconstriction in college athletes. J Asthma 49:153–157. https://doi.org/10.3109/02770903.2011.652329
Anderson SD, Argyros GJ, Magnussen H, Holzer K (2001) Provocation by eucapnic voluntary hyperpnoea to identify exercise induced bronchoconstriction. Br J Sport Med 35:344–347. https://doi.org/10.1136/bjsm.35.5.344
Brummel NE, Mastronarde JG, Rittinger D et al (2009) The clinical utility of eucapnic voluntary hyperventilation testing for the diagnosis of exercise-induced bronchospasm. J Asthma 46:683–686. https://doi.org/10.1080/02770900902972178
Burman J, Elenius V, Lukkarinen H et al (2020) Cut-off values to evaluate exercise-induced asthma in eucapnic voluntary hyperventilation test for children. Clin Physiol Funct Imaging 40:343–350. https://doi.org/10.1111/cpf.12647
Hallstrand TS, Leuppi JD, Joos G et al (2018) ERS technical standard on bronchial challenge testing: pathophysiology and methodology of indirect airway challenge testing. Eur Respir J 52:1801033. https://doi.org/10.1183/13993003.01033-2018
Hull JH, Ansley L, Price OJ et al (2016) Eucapnic voluntary hyperpnea: gold standard for diagnosing exercise-induced bronchoconstriction in athletes? Sport Med 46:1083–1093. https://doi.org/10.1007/s40279-016-0491-3
Price OJ, Ansley L, Hull JH (2015) Diagnosing exercise-induced bronchoconstriction with eucapnic voluntary hyperpnea: is one test enough? J Allergy Clin Immunol Pract 3:243–249. https://doi.org/10.1016/j.jaip.2014.10.012
GINA (2018) Global initiative for asthma (GINA). http://www.ginasthma.org. Accessed 11 Feb 2022
Roxo JPF, Ponte EV, Ramos DCB et al (2010) Validação do Teste de Controle da Asma em português para uso no Brasil: validation for use in Brazil. J Bras Pneumol 36:159–166. https://doi.org/10.1590/S1806-37132010000200002
Miller MR (2005) Standardisation of spirometry. Eur Respir J 26:319–338. https://doi.org/10.1183/09031936.05.00034805
Pereira C (2002) Espirometria. J Pneumol 28:S1–S82
Iftikhar IH, Greer M, Jaiteh A (2019) A meta-analysis of diagnostic test agreement between eucapnic voluntary hyperventilation and cardiopulmonary exercise tests for exercise-induced bronchoconstriction. Lung 197:483–492. https://doi.org/10.1007/s00408-019-00233-4
Rizzo JÂ, de Rodrigues Filho E, Gonçalves AV et al (2021) Reproducibility of eucapnic voluntary hyperpnoea for exercise-induced bronchoconstriction diagnosis in asthmatic children and adolescents. Pediatr Allergy Immunol 00:1–9. https://doi.org/10.1111/pai.13610
Anderson SD, Pearlman DS, Rundell KW et al (2010) Reproducibility of the airway response to an exercise protocol standardized for intensity, duration, and inspired air conditions, in subjects with symptoms suggestive of asthma. Respir Res 11:120. https://doi.org/10.1186/1465-9921-11-120
Nicolai T, Mutius EV, Reitmeir P, Wjst M (1993) Reactivity to cold-air hyperventilation in normal and in asthmatic children in a survey of 5,697 schoolchildren in Southern Bavaria. Am Rev Respir Dis 147:565–572. https://doi.org/10.1164/ajrccm/147.3.565
Argyros GJ, Roach JM, Hurwitz KM et al (1996) Eucapnic voluntary hyperventilation as a bronchoprovocation technique. Chest 109:1520–1524. https://doi.org/10.1378/chest.109.6.1520
Spiering BA, Judelson DA, Rundell KW (2004) An evaluation of standardizing target ventilation for eucapnic voluntary hyperventilation using FEV1. J Asthma 41:745–749. https://doi.org/10.1081/JAS-200028004
Blackie SP, Fairbarn MS, McElvaney NG et al (1991) Normal values and ranges for ventilation and breathing pattern at maximal exercise. Chest 100:136–142. https://doi.org/10.1378/chest.100.1.136
Williams NC, Johnson MA, Hunter KA, Sharpe GR (2015) Reproducibility of the bronchoconstrictive response to eucapnic voluntary hyperpnoea. Respir Med 109:1262–1267. https://doi.org/10.1016/j.rmed.2015.08.006
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
LCBdeBA, CGdeA, and ERF contributed to data collection, analysis, conception, and design. JÂR, DM, MAMdosS, SH, NG, and MAVdeCJ contributed to conception, design, and interpretation of the data, the drafting of the paper, or revising it critically for intellectual content; and the final approval of the version to be published. All authors agree to be accountable for all aspects of the work related to its accuracy or integrity and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University B (Date. 2019/No.: 2.796.049).
Consent to Participate
All parents and adolescents signed an informed consent form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rizzo, J.Â., de Barros Albuquerque, L.C.B., Medeiros, D. et al. Ventilation Rates Achieved in Eucapnic Voluntary Hyperpnea Challenge and Exercise-Induced Bronchoconstriction Diagnosis in Young Patients with Asthma. Lung 200, 229–236 (2022). https://doi.org/10.1007/s00408-022-00519-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00519-0