Abstract
Dengue fever is an arboviral disease transmitted to humans through the bites of infected female Aedes mosquitoes. Dengue virus is a member of the Flaviviridae family, and human infection can be caused by any of the four antigenically distinct serotypes (DENV 1–4). The infection has become recognized as the most important and prevalent arboviral disease in humans, endemic in almost 100 countries worldwide. Nearly 3 billion people live in areas with transmission risk. Autochthonous transmission of the virus in previously disease-free areas, increased incidence in endemic areas, and epidemic resurgence in controlled regions could increase the risk of contracting more severe forms of the disease, such as dengue hemorrhagic fever (DHF)/dengue shock syndrome (DSS). Symptomatic dengue virus infection can present with a wide range of clinical manifestations, from mild fever to life-threatening DSS. Thoracic complications may manifest as pleural effusion, pneumonitis, non-cardiogenic pulmonary edema, and hemorrhage/hemoptysis. No vaccine is currently available and no specific treatment for dengue fever exists, but prevention and prompt management of complications in patients with DHF can help reduce mortality. This review describes the main clinical, pathological, and imaging findings of thoracic involvement in DHF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dengue fever (DF) is an arthropod-borne viral disease transmitted to humans by the bites of infected female Aedes mosquitoes. Due to its high adaptability to urban environments, Aedes aegypti is considered to be the most important vector worldwide, with other species such as Ae. albopictus playing a minor role in disease transmission [1]. Dengue virus is a single-stranded positive-sense RNA virus of the genus Flavivirus (family Flaviviridae). Infection can be caused by any of the four antigenically distinct serotypes (DENV 1–4) [2].
The infection has become recognized as the most important and prevalent arboviral disease in humans. A recent estimate indicated that 390 million dengue infections occur per year, of which 96 million are symptomatic or sub-clinically impaired [3].
Dengue infection represents a major challenge to public health, as it is endemic in almost 100 countries worldwide and nearly 3 billion people live in areas with transmission risk [3,4,5]. Regions in which dengue infection is endemic are widespread throughout the tropics; Asia, Africa, and the Americas contribute with approximately 70, 16, and 14% of the global total infections, respectively [3]. Brazil and Mexico together, and India alone contribute with half of the Americas and Asia continental rates, respectively [3].
Dramatic expansion of the geographic areas of endemic dengue transmission worldwide has been noticed, as well as resurgent dengue activity [2]. Over the past five decades, the incidence of dengue virus infection has increased 30-fold [2]. Also, cases of autochthonous transmission have been reported, in which the virus is acquired in supposed free-diseased areas, without history of traveling to endemic regions [6]. Native female mosquitos are infected by biting a viraemic human (infected in other territory) and transmit the virus to other humans in the same territory [6, 7].
The introduction of autochthonous transmission, increased incidence in endemic areas, and epidemic resurgence in controlled regions could lead to an increased risk of more severe forms of the disease, such as dengue hemorrhagic fever (DHF)/dengue shock syndrome (DSS) or severe dengue (SD) [6, 7]. Symptomatic dengue virus infection can present with a wide range of clinical manifestations, from mild fever to life-threatening SD [7]. Lung involvement in dengue remains a controversial issue. Viral antigens have been demonstrated in lung tissue in experimental infection and autopsy specimens, and the virus appears to potentially infect macrophages and lung endothelial and epithelial cells [8, 9]. Pulmonary complications can present as pleural effusion, pneumonitis, non-cardiogenic pulmonary edema [acute respiratory distress syndrome (ARDS)], and hemorrhage/hemoptysis. These complications coincide with capillary leak syndrome and thrombocytopenia. Evaluations of the clinical spectrum of lung infection, however, are scarce in the literature; they are generally limited to case reports, and few comprehensive data on chest imaging findings are available [10,11,12,13,14,15,16,17].
Despite many efforts over the past 70 years, no approved vaccine is available. Various types of vaccine have been developed, and some are currently under preclinical or clinical evaluation [18]. No specific treatment for DF exists, but awareness of potential evolution to SD and prevention and prompt management of complications frequently save the lives of patients with DHF. With appropriate intensive supportive therapy, mortality may be reduced to < 1% [19]. The aim of this review is to describe the main clinical, pathological, and imaging aspects of pulmonary involvement in DHF.
Pathogenesis
Elevated vascular permeability, thrombocytopenia, and hemorrhage are the hallmarks of DHF. The precise mechanism implicated in plasma leakage has yet to be elucidated. The condition seems to involve no vasculitis, and hence no direct endothelial damage. A mediator-related functional change in the endothelium has traditionally been proposed to be responsible for plasma leakage in DHF, and recovery is rapid, abrupt, and without sequelae in most cases [20].
Evolution to DHF is widely accepted to be a multifactorial process, due to complex interaction among three major factors: (a) the virulence of infecting dengue viruses, (b) the host immune response and the phenomenon of antibody-dependent enhancement, and (c) intrinsic host factors, such as genetic background, previous health status, sex, and age [21,22,23].
Clinical Features
Infection with dengue virus can cause a myriad of signs and symptoms, although the majority of cases are asymptomatic or subclinical. Following an incubation period of 4–8 days, symptoms start and the patient usually undergoes a triphasic clinical course comprising (a) a febrile phase; (b) a so-called critical phase, in which fever usually remits; and (c) a recovery phase [24].
The febrile phase can be described by the occurrence of fever, retro-orbital pain, headache, myalgia, arthralgia, vomiting, prostration, lymphadenopathy, dysgeusia, and transient rash. Typically, this phase lasts 3–7 days. Mild to moderate leukopenia and thrombocytopenia, as well as an increase in hepatic aminotransferase blood level, may occur [25].
Defervescence and evident signs of increased capillary permeability characterize the critical phase, which lasts for 24–48 h. Hematocrit elevation, ascites, pleural effusion, hypoproteinemia, and even mild hemorrhage are common associated findings, with compensatory mechanisms taking place to maintain hemodynamics. Patients with young and old age, Caucasian race, AB blood type, and coexisting medical conditions (e.g., asthma, diabetes, sickle cell anemia) are at a higher risk of lacking an adequate hemodynamic response and progress to SD. Clinical signs of worsening disease include increasingly severe abdominal pain, hepatomegaly, and cold extremities [7, 26, 27]. Hemorrhagic manifestations along the DF spectrum are usually mild, and most commonly consist of scattered tiny petechiae on the skin and, occasionally, the submucosa. Tourniquet test positivity, which signals increased capillary fragility, skin petechiae, and ecchymoses are common findings that appear early in DHF. Epistaxis and gingival bleeding are also common and may be severe. Massive bleeding requiring blood transfusion is less common, usually occurs after the onset of shock, and is most commonly located in the gastrointestinal tract [28].
Gradual clinical improvement with reabsorption of transudated fluids takes place in the following 48–72 h, delineating the recovery phase. A second, sometimes pruritic, morbilliform rash may occur, often described as “white islands in a sea of red” [29]. It generally resolves with desquamation within 1–2 weeks. Electrocardiographic alterations are common, as is hypervolemia from prior fluid overload [29, 30].
Disease Classification
In the 1960s, the WHO began classifying symptomatic dengue infection cases as DF or DHF/DSS [31]. DHF was said to be present when all of the following four criteria were met: fever or history of fever lasting 2–7 days, hemorrhagic phenomenon, thrombocytopenia (platelet count < 100,000), and evidence of plasma leakage due to increased vascular permeability [31]. DHF could be further classified according to four grades of severity, where grades III and IV were considered to represent DSS.
A revised World Health Organization (WHO) case classification was introduced in 2009, replacing the traditional categories of DF and DHF/DSS with dengue with and without warning signs and SD [7]. However, the old WHO classification from 1960s continues to be widely used [7].
Criteria to diagnose probable dengue include history of living in or traveling to an endemic area, fever, and two of the following: nausea or vomit; rash; aches and pains; tourniquet test positive; leukopenia; and any warning sign [7]. Warning signs are defined by abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation, lethargy, hepatomegaly, and rapid decrease in platelet count concurrent with increase in hematocrit [7]. Characterizing SD requires the presence of one of the following: severe bleeding; severe organ impairment; and dengue shock (plasma leakage that can lead to shock of fluid accumulation, with or without respiratory insufficiency [7].
Diagnosis
Dengue virus infection produces a broad spectrum of symptoms, many of which are non-specific. Thus, a diagnosis based only on clinical symptoms is unreliable. Early laboratory confirmation of clinical diagnosis may be valuable because some patients progress over a short period from mild to severe disease, and sometimes to death. Early intervention may be lifesaving [24].
Diagnostic options include assays to detect the virus or its components (genome and antigen) or the host response to the virus. Assay choice depends on the timing of sample collection and the purpose of testing. Before day 5 of illness, during the febrile period, dengue infections may be diagnosed by virus isolation in cell culture, detection of viral RNA by nucleic acid amplification tests, or detection of viral antigens by enzyme-linked immunosorbent assay (ELISA) or rapid tests [2].
During the febrile phase, detection of viral nucleic acid in serum by reverse-transcriptase polymerase chain reaction (RT-PCR) assay, or detection of virus-expressed soluble non-structural protein 1 by ELISA or the lateral-flow rapid test, is sufficient for a confirmatory diagnosis [24]. Immunoglobulin M (IgM) seroconversion (≥ four-fold increase in antibody levels) between paired samples is considered to be a confirmatory finding, whereas IgM detection in a single specimen obtained from a patient with a clinical syndrome consistent with dengue is used widely to establish a presumptive diagnosis [7].
Pulmonary Involvement
Variable frequencies of respiratory symptoms in patients with dengue have been reported, but these symptoms are generally mild and mainly affect the upper airway. Thoracic involvement is common, in the form of pleural effusion as part of polyserositis found in DHF. Severe involvement of the lower respiratory system is rare in patients with dengue. DF is less likely than non-dengue febrile illness to present with respiratory symptoms [32,33,34,35].
Dyspnea may occur in patients with DF due to pleural effusion, ARDS, pulmonary hemorrhage, pneumonia, and shock [11, 36, 37]. Pleural effusion is the most frequent cause of dyspnea in patients with dengue, usually seen in the context of plasma leakage syndrome [38]. This effusion may be bloody, and a case of massive unilateral (right-sided) hemothorax has even been reported recently [16]. A small pleural effusion alone, however, is not a reliable marker of plasma leakage, as it is a common finding in patients with non-dengue febrile illness and those with DF [39].
ARDS is a heterogeneous clinical syndrome with a high mortality rate characterized by respiratory distress, severe hypoxemia, diffuse radiographic infiltrates, and decreased lung compliance [40]. Hypoxemia with a widened alveolar–arterial oxygen gradient is common in patients with SD. Non-cardiac pulmonary edema is a frequent complication of fluid replacement in patients with dengue and severe plasma leakage [41]. DSS is reported to be the third leading cause of ARDS in dengue-endemic areas [11, 12, 41]. Thus, especially in the setting of a dengue epidemic, the presence of DF should be investigated in patients with ARDS [42].
Diffuse alveolar hemorrhage (DAH), commonly defined as the association of hemoptysis, new pulmonary infiltrates on chest X-ray (CXR), and anemia, is a syndrome that results from diffuse bleeding into the acinar portion of the lung. However, DAH can present in about 40% of cases without hemoptysis [43]. As hemoptysis is an infrequent finding in DF, reported in 1.4% of dengue infections, and because imaging examinations are not routinely performed in patients diagnosed with dengue, some patients with dengue infection may have unrecognized pulmonary hemorrhage [15, 35]. DAH in DHF is, therefore, an even rarer event, scarcely reported in the literature [12,13,14,15].
Radiographic Findings
Rodrigues et al. [38] thoroughly evaluated lung involvement and CT imaging findings of DF. In a cohort of 2020 confirmed dengue cases, 29 patients (1.43%) underwent chest CT due to respiratory manifestations. In that series, 58.6% of patients who underwent chest CT showed abnormalities; pleural effusion was the major finding, observed in 55% of patients with abnormalities and constituting the sole finding in 35% of those patients [38]. Ground-glass opacity (GGO) was the most common finding of lung parenchymal involvement, noted in 27.5% of patients, followed by lung consolidation (20.6% of patients). Interlobar septal thickening and airspace nodules with no specific distribution were detected in two (6.82%) patients. No specific axial distribution was observed. The extent of disease in the chest tended to be greater in patients with SD than in those with DF, but this difference was not significant [38].
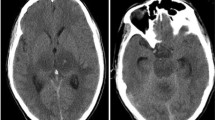
On CT, the acute abnormalities found in DAH correspond to patchy GGO without significant interlobular septal thickening. In the subacute phase, typically within 48 h, interlobular and intralobular interstitial thickening develop. Septal thickening may occur while GGOs persist, resulting in a crazy-paving pattern on CT images. Clearing of acute airspace opacities and septal thickening usually occur within 2 weeks in a monophasic episode of pulmonary hemorrhage [44]. Recent publications have described CT findings from isolated cases of pulmonary hemorrhage syndrome associated with DF. The patients presented similar aspects, with extensive areas of consolidation and/or diffuse GGO in both lungs [14, 45, 46]. These findings, although non-specific, are consistent with diffuse alveolar hemorrhage [43] (Figs. 1, 2, 3).
A 40-year-old woman with dengue hemorrhagic fever. Chest X-ray (a) performed in the intensive care unit showing extensive bilateral airspace consolidations. HRCT images (b–d) show peribronchovascular and peripheral ground-glass opacities associated with consolidations in both lungs as well as bilateral pleural effusion. Note also in d the presence of small right pneumothorax
Pathological Findings
DHF should be regarded as a multiorgan infection, and the lungs are invariably affected [42]. Pulmonary pathological findings in autopsy studies of dengue cases, particularly those of SD, are mononuclear inflammatory infiltrates, hyperplasia of alveolar macrophages, and hyaline membrane formation with hypertrophy of type II pneumocytes. Hyaline membrane is also found in the lungs of patients with ARDS in shock, but its pathogenesis seems to differ from that in dengue, as ARDS leads mainly to neutrophil inflammation, whereas mononuclear infiltrates have been described in dengue cases [9].
Dengue virus antigens and evidence of viral replication—such as negative-stranded RNA—have also been described in type II pneumocytes and pulmonary vascular endothelium [9]. Dilatation of subpleural lymphatic spaces, alveolar congestion, septal hemorrhage, acute DAH (Fig. 4), and pleural effusion have been reported in association with SD [12, 14, 41, 42, 47, 48]. Extensive lung involvement in fatal cases of dengue, especially in association with lung hemorrhage, is a terminal event and is probably associated with uncontrolled infection and shock [38].
Differential Diagnosis
Clinical and radiological distinction between dengue and other infections associated with diffuse pulmonary hemorrhage may be challenging. In immunocompetent patients, the most important infectious diseases for differential diagnosis include influenza A (H1N1), leptospirosis, malaria, and hantavirus pulmonary syndrome (HPS) [46, 49,50,51]. A few case reports have described co-infection of those pathogens with dengue virus. All of these conditions can occur in the context of similar epidemiological backgrounds, increasing the challenge of diagnosis [52,53,54,55,56]. A pattern of extensive or diffuse GGO and consolidation with a primarily peribronchovascular or subpleural distribution can be strongly related to influenza A (H1N1) infection [46]. Several diagnostic laboratory tests may be used to detect the presence of influenza viruses in respiratory specimens. Real-time RT-PCR has the greatest sensitivity and specificity [46, 51].
The most frequent high-resolution CT finding in leptospirosis is extensive, bilateral GGO involving all lobes. Areas of consolidation, peripheral airspace nodules, and pleural effusion may be present. The diagnosis of leptospirosis is based on clinical findings: a history of direct or indirect exposure of mucous membranes or abraded skin to infected animals or their urine; location in an endemic area, especially in the context of urban flooding or other immersion in contaminated water; and positive serologic test results [46, 49, 50].
In patients living or having traveled in endemic areas, malaria should be considered as a possible cause of respiratory failure of obscure etiology. General radiographic and high-resolution CT findings in malaria are consistent with non-cardiogenic pulmonary edema. PE, diffuse interstitial edema, and lobar consolidation may also be seen. Parasites may be detected on thick and thin peripheral blood smears [46].
HPS should be considered in patients with epidemiological histories of exposure to rodent bodily fluids or excreta. On CT, HPS may present with bilateral areas of GGO, thickened interlobular septa, poorly defined small nodules, and bronchial wall thickening. The etiological diagnosis can be confirmed by serological tests and detection of the viral genome by RT-PCR [46].
Conclusion
Dengue infection has become increasingly more prevalent in tropical and subtropical regions, imposing economic and social burdens on hundreds of thousands people in large urban areas. Thrombocytopenia, hemorrhage, and plasma leakage are the cornerstones of dengue hemorrhagic fever, but its pathophysiology remains poorly understood. Lung alterations are seldom seen in dengue, and imaging findings are probably related to increased vascular permeability. In the febrile phase of illness, the presence of plasma leakage, such as pleural effusion or ascites, may suggest the diagnosis of dengue. Imaging findings in dengue are non-specific and must be distinguished from several other infections that share common presentations, can coexist, and can occur in the same epidemiological setting. Diffuse alveolar hemorrhage is more frequently related to severe—and often fatal—forms of the disease like dengue hemorrhagic fever. Thoracic imaging findings may show complications and signal potential evolution to severe dengue. Recognition of these findings may help clinicians initiate prompt treatment and prevent mortality.
References
Lambrechts L, Scott TW, Gubler DJ (2010) Consequences of the expanding global distribution of Aedes albopictus for dengue virus transmission. PLoS Negl Trop Dis 4:e646
Guzman MG, Harris E (2014) Dengue. Lancet 6736:1–13
Bhatt S, Gething PW, Brady OJ et al (2013) The global distribution and burden of dengue. Nature 496:504–507
Shepard DS, Coudeville L, Halasa Y et al (2011) Economic impact of dengue illness in the Americas. Am J Trop Med Hyg 84:200–207
Ooi E, Gubler DJ (2009) Global spread of epidemic dengue: the influence of environmental change. Futur Virol 4:571–580
Gubler D (2002) Epidemic dengue/dengue hemorrhagic fever as a public health, social and economic problem in the 21st century. Trends Microbiol 10:100–103
World Health Organization (2009) Dengue: guidelines for diagnosis, treatment, prevention and control. Geneva World Heal Organ, Geneva
Jessie K, Fong MY, Devi S et al (2004) Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J Infect Dis 189:1411–1418
Póvoa TF, Alves AM, Oliveira CA et al (2014) The pathology of severe dengue in multiple organs of human fatal cases: histopathology, ultrastructure and virus replication. PLoS ONE 9:e83386
Lum L, Thong M, Cheah Y et al (1995) Dengue-associated adult respiratory distress syndrome. Ann Trop Paediatr 15:335–339
Sen M, Ojha U, Chakrabarti S et al (1999) Dengue hemorrhagic fever (DHF) presenting with ARDS. Indian J Chest Dis 41:115–119
Setlik R, Ouellette D, Morgan J et al (2004) Pulmonary hemorrhage syndrome associated with an autochthonous case of dengue hemorrhagic fever. South Med J 97:688–691
Sharma SK, Gupta BS, Devpura G et al (2007) Pulmonary haemorrhage syndrome associated with dengue haemorrhagic fever. J Assoc Phys India 55:729–730
Marchiori E, Ferreira JL, Bittencourt CN et al (2009) Pulmonary hemorrhage syndrome associated with dengue fever, high-resolution computed tomography findings: a case report. Orphanet J Rare Dis 4:8
Liam C, Yap B, Lam S (1993) Dengue fever complicated by pulmonary hemorrhage manifesting as hemoptysis. J Trop Med Hyg 96:197–200
Karanth SS, Gupta A, Prabhu M (2012) Unilateral massive hemothorax in dengue hemorrhagic fever: a unique presentation. Asian Pac J Trop Med 5:753–754
Kumar N, Gadpayle AK, Trisal D (2013) Atypical respiratory complications of dengue fever. Asian Pac J Trop Med 6:839–840
Ishikawa T, Yamanaka A, Konishi E (2014) A review of successful flavivirus vaccines and the problems with those flaviviruses for which vaccines are not yet available. Vaccine 32:1326–1337
Chaturvedi UC (2006) The curse of dengue. Indian J Med Res 124:467–470
Libraty DH, Endy TP, Houng HH et al (2002) Differing influences of virus burden and immune activation on disease severity in secondary dengue-3 virus infections. J Infect Dis 185:1213–1221
Kliks S, Nisalak A, Brandt E et al (1989) Antibody-dependent enhancement of dengue virus grouth in human monocytes as a factor for dengue hemorrhagic fever. Am J Trop Med Hyg 40:444–451
Rico-Hesse R, Harrison LM, Salas RA et al (1997) Origins of dengue type 2 viruses associated with increased pathogenicity in the americas. Virology 230:244–251
Stephens H (2010) HLA and other gene associations with dengue disease severity. Curr Top Microbiol Immunol 338:99–114
Simmons CP, Farrar JJ, Van Nguyen VC (2012) Dengue. N Engl J Med 366:1423–1432
Green S, Rothman A (2006) Immunopathological mechanisms in dengue and dengue hemorrhagic fever. Curr Opin Infect Dis 19:429–436
Tantracheewathorn T, Tantracheewathorn S (2007) Risk factors of dengue shock syndrome in children. J Med Assoc Thai 90:272–277
Wichmann O, Hongsiriwon S, Bowonwatanuwong C et al (2004) Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Trop Med Int Health 9:1022–1029
Tsai C, Kuo C, Chen P et al (1991) Upper gastrointestinal bleeding in dengue fever. Am J Gastroenterol 86:33–35
Waterman S, Gubler D (1989) Dengue fever. Clin Dermatol 7:117–122
Radakovic-Fijan S, Graninger W, Müller C et al (2002) Dengue hemorrhagic fever in a British travel guide. J Am Acad Dermatol 46:430–433
World Health Organization (1997) Dengue hemorrhagic fever: diagnosis, treatment, prevention and control. 2nd ed Geneva World Heal Organ
Potts JA, Rothman AL (2008) Clinical and laboratory features that distinguish dengue from other febrile illnesses in endemic populations. Trop Med Int Heal 13:1328–1340
Mustafa B, Hani AW, Chem YK et al (2010) Epidemiological and clinical features of dengue versus other acute febrile illnesses amongst patients seen at government polyclinics. Med J Malaysia 65:291–296
Halsey ES, Marks MA, Gotuzzo E et al (2012) Correlation of serotype-specific dengue virus infection with clinical manifestations. PLoS Negl Trop Dis 6:e1638
Hayes CG, Manaloto CR, Gonzales A et al (1988) Dengue infections in the Philippines: clinical and virological findings in 517 hospitalized patients. Am J Trop Med Hyg 39:110–116
Nelson ER (1960) Hemorrhagic fever in children in Thailand. Report of 69 cases. J Pediatr 56:101–108
Serufo JC, Nobre V, Rayes A et al (2000) Dengue: uma nova abordagem. Rev Soc Bras Med Trop 33:465–476
Rodrigues RS, Brum ALG, Paes MV et al (2014) Lung in dengue: computed tomography findings. PLoS ONE 9:e96313
Srikiatkhachorn A, Krautrachue A, Ratanaprakarn W et al (2007) Natural history of plasma leakage in dengue hemorrhagic fever a serial ultrasonographic study. Pediatr Infect Dis J 26:283–290
Devarajan TV, Prashant PS, Mani AK et al (2008) Dengue with ARDS. J Indian Acad Clin Med 9:146–149
Wang C, Liu S, Liao S et al (2007) Acute respiratory failure in adult patients with dengue virus infection. Am J Trop Med Hyg 77:151–158
Idirisinghe KAP (2013) Histopathological study of dengue haemorrhagic fever. J Diagn Pathol 2013:50–58
De Prost N, Parrot A, Cuquemelle E et al (2012) Diffuse alveolar hemorrhage in immunocompetent patients: etiologies and prognosis revisited. Respir Med 106:1021–1032
Balasubramanian S, Janakiraman L, Kumar SS et al (2006) A reappraisal of the criteria to diagnose plasma leakage in dengue hemorrhagic fever. Indian Pediatr 43:334–339
Lichtenberger JP, Digumarthy SR, Abbott GF et al (2014) Diffuse pulmonary hemorrhage: clues to the diagnosis. Curr Probl Diagn Radiol 43:128–139
Marchiori E, von Ranke F, Zanetti G et al (2012) Dengue hemorrhagic fever: another cause of diffuse alveolar hemorrhage in immunocompetent patients. Respir Med 106:1807–1808
von Ranke FM, Zanetti G, Hochhegger B et al (2013) Infectious diseases causing diffuse alveolar hemorrhage in immunocompetent patients: a state-of-the-art review. Lung 191:9–18
Weerakoon KG, Kularatne SA, Edussuriya DH et al (2011) Histopathological diagnosis of myocarditis in a dengue outbreak in Sri Lanka, 2009. BMC Res Notes 4:268
Aye KS, Charngkaew K, Win N et al (2014) Pathologic highlights of dengue hemorrhagic fever in 13 autopsy cases from Myanmar. Hum Pathol 45:1221–1233
Marchiori E, Müller NL (2002) Leptospirosis of the lung: high-resolution computed tomography findings in five patients. J Thorac Imaging 17:151–153
Marchiori E, Lourenço S, Setúbal S et al (2011) Clinical and imaging manifestations of hemorrhagic pulmonary leptospirosis: a state-of-the-art review. Lung 189:1–9
Marchiori E, Zanetti G, Fontes CA et al (2011) Influenza A (H1N1) virus-associated pneumonia: high-resolution computed tomography-pathologic correlation. Eur J Radiol 80:500–504
Ellis T, Imrie A, Katz AR et al (2008) Underrecognition of leptospirosis during a Dengue fever outbreak in Hawaii, 2001–2002. Vector-Borne Zoonotic Dis 8:541–547
Cadélis G (2012) Hémorragie intra-alvéolaire associée à une dengue et à une leptospirose. Rev Pneumol Clin 68:323–326
Borthakur B, Panwar D, Garg R et al (2011) Viral co-infection with dengue and H1N1 virus in a critical care setting. J Anaesthesiol Clin Pharmacol 27:236–238
Abbasi A, Butt N, Sheikh Q et al (2009) Clinical features, diagnostic techniques and management of dual dengue and malaria infection. J Coll Phys Surg Pak 19:25–29
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
de Almeida, R.R., Paim, B., de Oliveira, S.A. et al. Dengue Hemorrhagic Fever: A State-of-the-Art Review Focused in Pulmonary Involvement. Lung 195, 389–395 (2017). https://doi.org/10.1007/s00408-017-0021-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-017-0021-6