Abstract
Introduction
We report on a meta-analysis of Silexan, a proprietary active substance produced from Lavandula angustifolia, in subthreshold anxiety, mixed anxiety and depressive disorder (MADD), and generalized anxiety disorder (GAD).
Methods
The present analyses are based on all currently completed 5 double-blind, randomized, placebo-controlled trials investigating Silexan in adult out-patients who received Silexan 1 × 80 mg/day or placebo for ten weeks according to random assignment (n = 1213). Efficacy was assessed based on the Hamilton Anxiety Rating Scale (HAMA), several anxiety self-rating scales, the Clinical Global Impression (CGI) scale, and the Short Form-36 (SF-36) health status questionnaire.
Results
After ten weeks’ treatment, Silexan was significantly superior to placebo in reducing the HAMA total score (including the psychic and somatic anxiety sub-scores) and self-rated anxiety. Based on a ≥ 50% HAMA total score reduction, the responder rate ratio was 1.34 favoring Silexan, and the rate ratio of subjects much or very much improved according to the CGI was 1.51. Silexan was also significantly superior in improving the physical and mental health summary scores of the SF-36. There were no significant between-group differences concerning the occurrence of adverse events (AEs), serious AEs, and premature withdrawal due to AEs.
Conclusions
This meta-analysis demonstrates that Silexan exerts significant anxiolytic effects in subthreshold anxiety, GAD and MADD that were consistently reflected in investigator ratings and patient-reported outcomes, including improvement of health-related life-quality, while showing favorable tolerability and safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anxiety disorders are the most prevalent psychiatric disorders, the 12-month prevalence of anxiety disorders was estimated at 10.3% and a lifetime prevalence around 34% [4, 7]. While global health, measured by disability-adjusted life-years (DALYs) attributable to a pool of 369 diseases and injuries and standardized for population growth and ageing, has steadily improved over the last 30 years, the standardized rate of DALYs caused by anxiety disorders has remained stable [7]. Thus, their relative importance as a cause of disability has increased. In 2019, diagnosed anxiety disorders were ranked to be the 15th most important non-communicable cause of DALYs in patients of all sexes and ages, the 10th most important in patients between 25 and 49 years of age, and the 3rd most important in patients aged 10–24 years, with higher prevalence rates in females [21]. However, according to an Australian study, only 27% of 966 participants meeting the diagnostic criteria of a past-year anxiety disorder according to the International Classification of Diseases, Tenth Revision (ICD-10) sought the assistance of a health care professional. While 61% of those received an evidence-based intervention, 31% received minimally adequate treatment [27]. These findings are consistent with European data indicating that less than 20% of patients with an anxiety disorder are treated adequately [31]. Since anxiety disorders are associated with a high burden of illness [5, 7], they may have negative consequences, including disability, low life-quality, reduced ability to work leading to loss of productivity, and a high suicidal risk when remaining un- and undertreated [31].
With regard to the pharmacotherapy of anxiety disorders, current international practice guidelines [e.g., 1, 3, 6, 7, 20, 40, 48, 59] mainly recommend selective serotonin reuptake inhibitors (SSRIs–e.g., citalopram, escitalopram, paroxetine, sertraline) and serotonin-norepinephrine reuptake inhibitors (SNRIs–e.g., venlafaxine, duloxetine) as first-line and tricyclic antidepressants (TCAs) and moclobemide as second-line treatments. Further second-line recommendations exist for add-on benzodiazepines in short-term given their potential to develop abuse and dependence [e.g., 5, 9, 55] as well as undesired sedation [5, 34]. The latter adverse effect (AE) refers also to buspirone, representing further second-line psychopharmacotherapeutic option, and partly to pregabalin that can be very effectively applied as add-on treatment in patients with generalized anxiety disorder (GAD).
Due to the potential AEs mentioned above and those of SSRIs and SNRIs, which may include jitteriness, nausea, restlessness, headache, fatigue, altered appetite, weight gain or loss, tremor, sweating, QTC prolongation, sexual dysfunction, diarrhea, and constipation [5], and potential paradoxical and discontinuation symptoms [17, 18, 49], which are, importantly, less pronounced under SSRIs and SNRIs as compared to TCAs [7], the currently recommended medication for anxiety disorders may be suboptimal in terms of tolerability [52}. In turn, the potentially associated reluctance to adhere to the psychopharmacotherapy may explain why anxiety disorders remain un- or undertreated [12]. After years of relative stagnation in anxiolytic drug development [24], a growing interest in the investigation of novel psychopharmaceutic targets has led to an increased investigation and introduction of promising compounds including the effective and well tolerable phyto-pharmacotherapeutic alternative Silexan.
The pharmacological profile of the herbal compound Silexan,Footnote 1 an essential oil for oral administration manufactured from Lavandula angustifolia flowers complying with and exceeding the quality definition the monograph Lavender oil of the Ph. Eur. [38, 46], has been assumed to be based on a potent inhibition of voltage-dependent calcium channels (VDCCs) as demonstrated in studies with murine synaptosomes, primary hippocampal neurons and stably overexpressing cell lines [56]. Inhibition of VDCCs is thought to attenuate the overreaching, situationally inadequate stress response of the central nervous system associated with anxiety and mood disorders [53]. Furthermore, Silexan has been shown to significantly increase the density of 5-HT1A receptors and to reduce the serotonin-1A receptor binding potential, leading to increases in extracellular serotonin, dopamine, and norepinephrine [2, 41].
The rapidly growing number of international studies, reviews and meta-analyses indicates a huge interest in lavender oil preparations for the treatment of the so-called subthreshold anxiety [60], anxiety disorders, their frequent comorbidities and related symptoms [8, 58, 61]. In terms of subthreshold anxiety and anxiety disorders, Donelli et al. [15] as well as Sayed et al. [54] reviewed randomized and non-randomized studies investigating different lavender oil preparations with various routes of administration (e.g., oral, aromatherapy, massage oil), while Generoso et al. [22] and Yap et al. [63] focused on Silexan. Hereby, meta-analyses of different strengths of Silexan, that was investigated in one reference-controlled and four placebo-controlled clinical trials in anxiety disorders, were presented. Furthermore, Möller et al. [44] reviewed the effects of Silexan in placebo-controlled trials in subthreshold anxiety disorders. Our research adds to the existing evidence by presenting a meta-analysis of all placebo-controlled, therapeutic trials with the currently marketed dosage of 1 × 80 mg/day Silexan in subthreshold anxiety, mixed anxiety and depressive disorder (MADD) and GAD completed to date.
Materials and methods
Study and participant characteristics
A total of five randomized, double-blind, placebo-controlled clinical trials investigating the efficacy and tolerability of Silexan in subthreshold anxiety and anxiety disorders were completed by the manufacturer of Silexan at the end of the year 2020 [33, 35,36,37, 39]. Additionally, free-text searches of all fields of PubMed as well as of the EU Clinical Trials Register, the ISRCTN Register and of the ClinicalTrials.gov register were performed to identify any other studies with Silexan in subthreshold anxiety and anxiety disorders performed independently of the manufacturer. Search terms were ‘anxiety’ in combination with either ‘Silexan’, ‘Lasea’, ‘WS1265’ or ‘WS 1265’ (‘WS 1265’ was the internal code used by the manufacturer for Silexan) and suppressing the automatic PubMed translation of ‘Silexan’ to ‘lavender oil’ when building the search query. Searches were performed from the earliest record until December 2022. Searching PubMed resulted in 37 matches, none of which referred to a double-blind, randomized, placebo-controlled, therapeutic clinical trial with Silexan in subthreshold anxiety and anxiety disorders beyond those already mentioned. Searches in the indicated trial registers also did not add any clinical trials meeting these criteria.
The 5 trials included into our analysis were performed according to essentially similar protocols that differed mainly in the diagnosis for inclusion and in the derived inclusion and exclusion criteria as well as in some secondary outcome measures (Table 1). Trial A reported by Kasper et al. [35] (trial A) assessed patients with subthreshold anxiety, Kasper et al. [33] (trial B) investigated patients with restlessness and sleep disturbances, the trial of Kasper et al. [39] (trial C) was performed in patients with MADD, and Kasper et al. [37] (trial D) as well as Kasper et al. [36] (trial E) investigated patients suffering from GAD. In all trials, the participants were male or female out-patients between 18 and 65 years of age who sought treatment by a psychiatrist or by a general practitioner. In addition to meeting the diagnostic criteria for inclusion shown in Table 1, eligible participants had to have a baseline Hamilton Anxiety Rating Scale (HAMA; [26]) total score ≥ 18 points and had to meet other anxiety specific eligibility criteria as shown in Table 1.
The schedule of each trial started with a 3–7-day qualification phase after which eligible subjects entered a 10-week double-blind, randomized treatment phase. Eligibility criteria had to be met both at the start (screening) and at the end of the qualification phase (baseline). In trials A, B, D, and E, post-baseline outcome assessments were scheduled every two weeks while the protocol of trial C included assessments at the end of weeks one, two, four, seven, and ten.
Interventions
Participants took Silexan or matching placebo for 10 weeks. Treatments were available in immediate-release soft gelatin capsules. Silexan is a proprietary essential oil manufactured from Lavandula angustifolia flowers by steam distillation that complies with the monograph Lavender oil of the European Pharmacopoeia and exceeds the quality requirements of the monograph. Batch to batch consistency is assured by a well-defined, standardized manufacturing process. To avoid inadvertent unblinding, the smell of the capsules containing Silexan was matched by flavoring the capsules containing placebo with 1/1000 of the amount of lavender oil contained in the Silexan capsules.
Analyses were performed on trial participants who received either the recommended daily dose of the marketed product, i.e., 1 × 80 mg Silexan, or placebo. Trial D also included additional treatment arms with 10 and 40 mg/day Silexan. In trial E, paroxetine served as an active control, and another group received Silexan 160 mg/day. The results of these treatment groups were not considered in our meta-analysis.
Meta-analysis outcomes
Meta-analyses were conducted according to a prospectively defined analysis plan. Analyses were performed for change between baseline and individual end of treatment of the 14-item HAMA as an observer rating scale of anxiety using the total score, HAMA sub-scores ‘Psychic anxiety’ and ‘Somatic anxiety’ [42] as well as the single HAMA items ‘Anxious mood’, ‘Tension’, ‘Sleep’, ‘Intellectual’, ‘Depressed mood’, ‘Somatic – muscular’, and ‘Somatic – sensory’. Additional analyses were performed on the following outcomes: the total scores of the Zung Self-Rating Anxiety Scale (SAS; [66]), of the Covi Anxiety Scale (CAS; [13]), and the anxiety score of the Hospital Anxiety and Depression Scale (HADS; [65]). These rating scales were applied in different trials (Table 1) and were used in our meta-analysis as subject self-ratings of anxiety. Clinical Global Impressions scale (CGI; [48]) item ‘Global improvement’ was evaluated as a global, observer-rated assessment of change in mental health. The ‘Mental health’ and ‘Physical health’ summary scores of the Short Form Health Survey (SF-36; [62]) administered in 4 out of the 5 trials were included as patient-reported measures of disease-associated quality of life. Moreover, we assessed treatment response defined prospectively as a ≥ 50% reduction of the HAMA total score compared to baseline or a score ≤ 2 (‘much improved’) for CGI item ‘Global improvement’ as well as full remission defined as a HAMA total score < 7 points at the end of the treatment [43].
Tolerability was assessed by analyzing the proportions of subjects in each treatment group with at least one AE, at least one serious AE (SAE), and subjects prematurely withdrawn due to an AE.
Statistical methods
Meta-analyses were performed on the individual subject data of the included trials that were obtained from the study sponsor. The applicable analysis data sets included the full analysis set (FAS) of the original protocols for all efficacy-related outcomes and the safety analysis set for analyses of AEs as well as for premature withdrawal. For efficacy outcomes, missing data were imputed by carrying forward the last valid observation in order to maintain comparability with the published results of the trials.
To characterize the study populations, descriptive statistics were computed for age, sex, and premature withdrawal rate. Meta-analyses were based on a two-stage approach [10, 50]: within each trial, continuous outcomes were analyzed using analysis of covariance (ANCOVA) with the difference between baseline and end of treatment for the outcome of interest as the dependent variable, treatment as a factor, and the baseline value of the analyzed outcome as a covariate. For the analysis of CGI item ‘Global improvement’, the baseline score of the item ‘Severity of illness’ was used as a covariate. Scores from items and (sub-)scales were analyzed as continuous outcomes. Marginal (adjusted) mean values and their standard deviations were then used as input for a random-effects meta-analysis on the treatment group mean difference. Inverse variance weighting was used for combining the results of the single trials, and the DerSimonian-Laird method was applied for calculating the variance between the trials. Mean differences (MD) were estimated for the continuous outcomes when the same scale was used in all trials. These effect sizes were presented in forest plot visualizations. Additionally, standardized mean differences (SMD) based on bias-corrected Hedges´ g were indicated within the text to provide better comparability with the literature. Where different scales were used (i.e., various anxiety self-rating sores), SMDs were presented in the forest plot.
For binary outcomes, (1) risk ratios (RRs) (response and remission rates) and (2) odds ratios (ORs) (occurrence of AEs, attrition rates), both accompanied by 95% confidence intervals (CIs), were calculated as effect sizes. Meta-analyses of binary efficacy outcomes were performed using random effects models with the inverse variance method. For safety outcomes, fixed effects models were calculated using Mantel–Haenszel weighting for combining the results from single trials.
For the investigation of subgroups, we used mixed effects models assuming random effects within subgroups and a fixed effect across subgroups.
All p-values are two-sided; values ≤ 0.05 were considered descriptively significant.
Heterogeneity between the trials was assessed using the I2 statistic in accordance with the criteria proposed in Deeks et al. [14].
Meta-analyses were computed with R software (version 3.6.0) using functions ‘metacont’ (for continuous outcomes), ‘metabin’ (for binary outcomes), and ‘forest’ included in package meta (version 4.13–0). All other analyses were performed in SAS statistical software version 9.4 for Windows.
Results
Study participant characteristics
In the pooled data set including all five trials, a total of 1213 subjects (Silexan 610; placebo 603) were randomized and 1172 (Silexan 587; placebo 585) were analyzed for efficacy in the FAS (Table 2) and 1206 (Silexan 606; placebo 600) for safety. Overall withdrawal rates were low (12% in the Silexan group and 11% in the placebo group).
In total, 382 patients suffered from subsyndromal anxiety, 315 from MADD and 790 from GAD (FAS). The participants’ age averaged around 46 years. More than 2/3 of the subjects of all trials were female.
Within each trial, the HAMA total score baseline mean values were essentially comparable between treatment groups, with a mean value difference of 0.2 points for the pooled data set including all trials. Moreover, the average baseline HAMA total scores of subjects with diagnoses characterized by subthreshold anxiety (trials A-C) and of subjects with GAD (trials D, E) were in a comparable range.
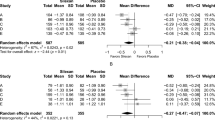
Anxiety: observer rating
Silexan was significantly more efficacious than placebo in the management of anxiety disorders. Analyzing the HAMA total score reduction, this meta-analysis revealed an average 2.9-point advantage for Silexan over placebo (p = 0.002) (Fig. 1), with an estimated minimum benefit of 1.1 points according to the lower bound of the 95% CI. The estimated mean difference corresponds to an SMD of 0.35 (95% CI 0.13; 0.56) favoring Silexan. During the 10-week randomized treatment period, the HAMA total score decreased by averages between 10.8 (trial C) and 16.0 points (trial A) for Silexan and by between 8.4 (trial C) and 11.4 points (trial D) in the placebo groups (Fig. 1).
Figure 1 also indicates that Silexan was significantly superior to placebo in 4 out of the 5 individual trials included in the meta-analysis. Substantial heterogeneity (I2 = 72.7%) was mainly attributable to between-trial differences in effect sizes favoring Silexan, not to different directions of the treatment effect.
Figure 2 summarizes the treatment group mean differences and their 95% CIs determined in meta-analyses of the HAMA psychic and somatic anxiety sub-scores (upper panel) and for individual HAMA items identified prospectively in the analysis plan (lower panel). According to the lower bounds of the 95% CIs, Silexan was significantly superior to placebo in reducing anxiety-associated symptoms for both sub-scales as well as for all single HAMA items investigated, with the largest effect sizes observed for anxious mood followed by tension and insomnia.
Main results of subgroup meta-analyses of HAMA total score change broken down by subject sex, age, as well as by somatic complaints at baseline (based on the sum of the scores of HAMA items ‘Somatic muscular’ and ‘Somatic sensory’) and by intellectual impairment (based on HAMA item ‘Intellectual’) are presented in Fig. 3. Whereas the effect sizes for female and male subjects were comparable, elderly subjects showed a larger treatment effect than younger participants, and comparatively larger improvements were also observed for subjects with more pronounced somatic complaints and intellectual impairment (i.e., difficulty in concentration, poor memory) at baseline. Figure 3 also shows that Silexan was significantly superior to placebo in all subsets investigated.
Meta-analysis of trials A–E. Hamilton Anxiety Scale total score treatment group differences for change between baseline and end of treatment in pre-defined subsets of subjects (random effects model point estimates and 95% confidence intervals; number of valid subjects for Silexan/placebo in parentheses)
At end of treatment, 304/587 subjects (51.8%) of the Silexan 80 mg/day groups of the 5 trials and 227/585 subjects (38.8%) of the placebo groups showed a HAMA total score reduction by ≥ 50% of their baseline value and were thus classified as treatment responders, with a meta-analysis risk ratio of 1.34 favoring Silexan (p = 0.004; Fig. 4). The corresponding number needed to treat (NNT, with 95% CI) was 8 (5; 28) for trials A–E and 6 (4; 36) for trials A-C (performed in subthreshold anxiety). Complete remission (i. e., a HAMA total score < 7 points at end of treatment) was achieved by 167/587 (28.4%) and 130/585 subjects (22.2%) for Silexan and placebo, respectively (meta-analysis risk ratio: 1.29; p = 0.013).
Anxiety: self-rating
The results of the meta-analysis performed on change from baseline of the total scores of the anxiety self-rating scales (trials A, B: SAS, trial C: HADS, trials D, E: CAS) are presented in Fig. 5. To account for the different ranges of the scales, standardized mean differences (SMDs) based on Hedges’ g with bias correction were calculated as effect size. Significant superiority of Silexan group over placebo was determined with a SMD of 0.27 standard deviation units (p < 0.0001). For trial D, showing the lowest effect size (of the included/individual trials) in the observer-rated HAMA (Fig. 1), the standardized mean difference to placebo in the subject self-rating (Fig. 5) differed only marginally from the meta-analysis average across all trials.
Clinical global impression
Analyzing the CGI item ‘Global improvement’ as parameter for the participants’ general mental condition, Silexan 80 mg/day was significantly superior to placebo. (Fig. 6, upper panel; MD = 0.53; p < 0.001). The corresponding SMD amounted to 0.44 (95% CI 0.25; 0.63) favoring Silexan. In the accompanying meta-analysis of dichotomous/binary treatment response based on the CGI (Fig. 6, lower panel), Silexan-treated subjects were on average 51% more likely to be much or very much improved than placebo-treated subjects according to the risk ratio (p < 0.001), with a pooled responder rates of 59.5% (335/563 subjects) and 39.8% (226/568 subjects) for Silexan and placebo, respectively, and an NNT of 5 (95% CI: 4; 8).
Disease-associated quality of life
Figure 7 presents the meta-analysis results for the physical (upper panel) and mental health (lower panel) summary scores of the SF-36. Improvements in both domains of patient-reported, disease-associated quality of life were significantly more pronounced for Silexan than for placebo (MD = 5.83 [physical health]; MD = 8.13 [mental health]; p < 0.001 for both summary scores), corresponding to a SMD of 0.58 for physical health and of 0.81 for mental health.
Tolerability
No significant between-group differences for the occurrence of at least one AE (OR = 1.16, 95%-CI 0.91; 1.49, p = 0.24, fixed effect model) and at least one SAE (OR = 1.18, 95% CI 0.38; 3.69, p = 0.73, fixed effects model) could be determined. SAEs were reported in a total of 6/606 subjects (1.0%) for Silexan and in 5/600 (0.8%) for placebo.
There was no evidence for a difference between groups in the risk of premature withdrawal due to AE (OR = 1.14, 95% CI 0.55; 2.33, p = 0.73, fixed effect model). The corresponding attrition rates were 2.6% (16/606 subjects) for Silexan and 2.3% (14/600 subjects) for placebo.
Discussion
With 14 clinical trials of different development phases published by the end of the year 2020 and a total of about 2,200 subjects evaluated, Silexan is probably the best researched herbal medicinal product for the treatment of subthreshold anxiety, anxiety disorders and related clinical manifestations worldwide [8, 44, 58, 61]. The body of evidence includes 5 double-blind, randomized, placebo-controlled trials in subthreshold anxiety and anxiety disorders, all of which were included into our meta-analysis. Silexan, administered at the marketed dosage of 1 × 80 mg/day, was shown to be significantly superior to placebo in the observer-rated HAMA, including its psychic and somatic anxiety sub-scores and a set of prospectively selected single HAMA items, as well as in different patient-reported anxiety scales. Hence, the anxiolytic effect of Silexan was not exclusively observed by the attending physicians but also subjectively perceived by the study participants. Beyond the indication-specific symptoms assessed by means of the anxiety scales, the herbal medicinal product was also associated with significant improvements in patient's global functioning as assessed by the CGI, indicating a beneficial effect on mental health. Finally, our meta-analysis also showed a significant positive effect of Silexan on patient-reported, disease-associated quality of life, with comparable improvements over placebo in the areas of mental and physical health. The latter results correspond with existing evidence reporting beneficial effects of Silexan on co-occurring depressive symptoms [8], sleep disturbances [58], as well as psychosomatic symptoms as fatigue and pain for instance [61].
Importantly, superiority over placebo was observed for all diagnostic categories represented in our meta-analysis (subthreshold anxiety disorder, MADD, GAD). While our analyses were limited to the marketed Silexan dosage of 1 × 80 mg/day, a pooled analysis of the placebo-controlled trials performed in GAD (trials D and E) published by Kasper et al. [37] showed a clear dose–response relationship for once-daily doses of Silexan between 10 and 160 mg, with 80 mg/day at the lower end of the therapeutic range and a substantially more pronounced anxiolytic effect at 160 mg/day, the maximum dosage investigated in these trials. It is also worth mentioning that 160 mg/day were not associated with a higher rate of AEs than lower dosages of Silexan or placebo [36, 37].
For HAMA total score reduction from baseline, our meta-analysis also indicates significant superiority of Silexan over placebo for prospectively defined subsets of subjects. While women are more frequently affected by anxiety disorders than men [21] and at least 2/3 of the subjects in each trial were female, our subgroup analysis indicates that subjects of both sexes show a similarly pronounced response to Silexan. For subsets defined by age, it is certainly of clinical interest that treatment with the herbal medicinal product was at least as efficacious in elderly subjects as in younger ones, even though the number of participants aged 60 or above was quite low since patients aged over 65 were excluded from the trials. Similar observations were reported in a meta-analysis by von Känel et al. [61] who found that the effect of Silexan on somatic symptoms and physical health of patients with anxiety disorders was largely independent of age and sex. Consistent with our findings, this meta-analysis could determine a superiority of Silexan over placebo in treating somatic manifestations of anxiety [61].
At baseline, close to 2/3 of the subjects in the pooled data set suffered from at least moderate, anxiety-related difficulties in concentration and poor memory (labelled ‘Intellectual impairment’ in the HAMA). Our subgroup meta-analysis indicates that subjects initially affected by these difficulties showed improvement of anxiety-associated symptoms, including impaired memory and concentration, and benefited from Silexan treatment to at least the same extent as those with lower or no baseline impairment. This is consistent with other research showing that, unlike several other anxiolytic drugs, Silexan is devoid of central depressant effects [57, 58].
For HAMA total score change, which served as a primary outcome measure of anxiolytic efficacy in all trials available for analysis, no minimal clinically important difference (MCID) has yet been derived empirically, and thus the interpretation of differences between medication and placebo with regard to clinical meaningfulness is not straightforward. According to the protocols of the included trials, a treatment group mean value difference in HAMA total score reduction of between 2.5 and 3.5 points was assumed to be clinically important. The observed meta-analysis mean value difference of 2.93 points was found to be within this range, and 4 out of the 5 analyzed trials showed mean differences between 2.43 and 8.5 points favoring Silexan. Standardized effect size comparisons between anxiolytic agents and placebo for HAMA total score change versus baseline in patients with GAD have been determined in several meta-analyses: Hidalgo et al. [29] (21 trials) reported effect sizes of 0.50 for pregabalin, 0.45 for hydroxyzine, 0.42 for venlafaxine, 0.38 for benzodiazepines, 0.35 for SSRIs, and 0.17 for buspirone. Gomez et al. [23] (56 trials) found effect sizes of 0.33 for SSRIs, 0.34 for SNRIs, 0.50 for benzodiazepines, and of 0.37 for all drug classes combined. In the analysis of Carl et al. [11], meta-analysis effect sizes were 0.38 for psychopharmacotherapy (43 trials) and 0.76 for psychotherapy (39 trials). With an SMD of 0.35, the standardized effect size for Silexan determined in this meta-analysis was thus in the range of the effect sizes for SNRIs and for SSRIs, which are currently recommended as first-line treatment for anxiety disorders [1, 6, 7, 29, 40, 47, 59]. Moreover, when comparing the efficacy of Silexan with that of other medicinal herbs, Silexan yielded the highest effect size when analyzing the herbs with an at least moderate cumulative sample size [64].
There is evidence that reluctance to accept the unwanted effects of conventional anxiolytic agents such as SSRIs, SNRIs and benzodiazepines, together with concerns regarding the sustainability of their anxiolytic effects [52], may contribute to the not seldom occurring under- or even un-treatment of anxiety disorders [12]. AEs attributed to Silexan were mainly limited to mild, transient gastrointestinal effects such as nausea or eructation [63]. The herbal product does, however, not interfere with activities of daily living [34], including driving performance [45], and has neither a sedating effect nor a potential for abuse [57, 58]. Silexan does also not cause withdrawal symptoms even when discontinued abruptly [19] and does not interact with oral contraceptives [28], which is an important finding since an appreciable proportion of patients affected by anxiety disorders and subthreshold anxiety are young female patients [60]. Generally, therapeutic doses of Silexan did not show any interaction potential with activities of cytochrome P450 enzymes CYP1A2, 2C9, 2C19, 2D6, and 3A4 [16].
In anxiety disorders, an appreciable proportion of patients has been shown to respond favorably to placebo treatment [25]. This is also a known issue in placebo-controlled trials in the indication, and placebo response rates have been shown to even rise during the last decades [51]. The results of the individual studies and our meta-analyses in favor of Silexan are remarkably consistent.
As a limitation of this work, all trials available for analysis were initiated by the manufacturer of Silexan and performed in one country (Germany). However, a number of reviews and meta-analyses of the effects of lavender preparations in general and of Silexan in particular has been published independently [15, 30, 54, 63], which underlines the scientific and clinical interest in the application of lavender oil preparations in and beyond anxiety disorders and the robustness and soundness of the results. Although there appears to be a general agreement among the authors that Silexan has a significant and clinically meaningful anxiolytic effect, further independent trials which would investigate the broad potential of its efficacy would be welcome. As a further potential limitation, it should be considered that the diagnoses of the enrolled patients differed between the individual trials. In one trial, participants suffering from mixed anxiety and depressive disorder were recruited [39]. However, in all included trials, patients had to fulfill an anxiety specific inclusion criterion (HAMA total score of ≥ 18 points).
In conclusion, our meta-analysis shows a clinically important anxiolytic effect of Silexan at the marketed dosage of 1 × 80 mg/day in subthreshold anxiety and anxiety disorders, with statistically significant superiority over placebo. A beneficial effect was consistently observed for observer-rated and for patient-reported anxiety, for overall mental condition, as well as for self-rated, disease-associated quality of life. Moreover, significant superiority of Silexan was also stable within several pre-specified subsets of subjects defined by demographic features and baseline characteristics. The analyses do not indicate a systematic, Silexan-associated risk of AEs above the placebo level.
Data availability
Raw data cannot be shared both due to ethical reasons and to data protection laws. To the extent permitted by law, the trial data required for validation purposes have already been disclosed in result reports on corresponding databases. All relevant data are within the paper.
Notes
Silexan® is the proprietary active ingredient of Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany.
References
Andrews G, Bell C, Boyce P, Gale C, Lampe L, Marwat O, Rapee R, Wilkins G (2018) Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of panic disorder, social anxiety disorder and generalised anxiety disorder. Aust N Z J Psychiatry 52:1109–1172
Baldinger P, Höflich AS, Mitterhauser M, Hahn A, Rami-Mark C, Spies M, Wadsak W, Lanzenberger R, Kasper S (2015) Effects of Silexan on the serotonin-1A receptor and microstructure of the human brain: a randomized, placebo-controlled, double-blind, cross-over study with molecular and structural neuroimaging. Int J Neuropsychopharmacol 18:1–9
Bandelow B (2020) Current and novel psychopharmacological drugs for anxiety disorders. Adv Exp Med Biol 1191:347–365
Bandelow B, Michaelis S (2015) Epidemiology of anxiety disorders in the 21st century. Dial Clin Neurosci 17:327–335
Bandelow B, Michaelis S, Wedekind D (2017) Treatment of anxiety disorders. Dial Clin Neurosci 19:93–107
Bandelow B, Sher L, Bunevicius R, Hollander E, Kasper S, Zohar J, Möller HJ (2012) Guidelines for the pharmacological treatment of anxiety disorders, obsessive-compulsive disorder and posttraumatic stress disorder in primary care. Int J Psychiatry Clin Pract 16:77–84
Bandelow B, Werner AM, Kopp I, Rudolf S, Wiltink J, Beutel ME (2021) The German Guidelines for the treatment of anxiety disorders: first revision. Eur Arch Psychiatry Clin Neurosci 1–12
Bartova L, Dold M, Volz HP, Seifritz E, Möller HJ, Kasper S (2022) Beneficial effects of Silexan on co-occurring depressive symptoms in patients with subthreshold anxiety and anxiety disorders: randomized, placebo-controlled trials revisited. Eur Arch Psychiatry Clin Neurosci
Bonnet U, Scherbaum N (2017) How addictive are gabapentin and pregabalin? A systematic review. Eur Neuropsychopharmacol 27:1185–1215
Burke DL, Ensor J, Riley RD (2017) Meta-analysis using individual participant data: one-stage and two-stage approaches, and why they may differ. Stat Med 36:855–875
Carl E, Witcraft SM, Kauffman BY, Gillespie EM, Becker ES, Cuijpers P, Van Ameringen M, Smits JAJ, Powers MB (2020) Psychological and pharmacological treatments for generalized anxiety disorder (GAD): a meta-analysis of randomized controlled trials. Cogn Behav Ther 49:1–21
Collins KA, Westra HA, Dozois DJ, Burns DD (2004) Gaps in accessing treatment for anxiety and depression: challenges for the delivery of care. Clin Psychol Rev 24:583–616
Covi L, Rickels K, Lipman RS, McNair DM, Smith VK, Downing R, Kahn R, Fisher S (1981) Effects of psychotropic agents on primary depression. Psychopharmacol Bull 17:100–103
Deeks JJ, Higgins JPT, Altman DG (2020) Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds.) Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). The Cochrane Collaboration. http://www.training.cochrane.org/handbook. Updated Sept 2020
Donelli D, Antonelli M, Bellinazzi C, Gensini GF, Firenzuoli F (2019) Effects of lavender on anxiety: a systematic review and meta-analysis. Phytomedicine 65:153099
Doroshyenko O, Rokitta D, Zadoyan G, Klement S, Schläfke S, Dienel A, Gramatté T, Lück H, Fuhr U (2013) Drug cocktail interaction study on the effect of the orally administered lavender oil preparation Silexan on cytochrome P-450 enzymes in healthy volunteers. Drug Metab Dispos 41:987–993
Fava GA (2020) May antidepressant drugs worsen the conditions they are supposed to treat? The clinical foundations of the oppositional model of tolerance. Ther Adv Psychopharmacol 10:1–11
Fava GA, Cosci F (2019) Understanding and managing withdrawal syndromes after discontinuation of antidepressant drugs. J Clin Psychiatry 80:19com12794
Gastpar M, Müller WE, Volz HP, Möller HJ, Schläfke S, Dienel A, Kasper S (2017) Silexan does not cause withdrawal symptoms even when abruptly discontinued. Int J Psychiatry Clin Pract 21:177–180
Gautam S, Jain A, Gautam M, Vahia VN, Gautam A (2017) Clinical practice guidelines for the management of generalised anxiety disorder (GAD) and panic disorder (PD). Indian J Psychiatry 59:S67–S73
GBD Diseases and Injuries Collaborators, 2020 (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222
Generoso MB, Soares A, Taiar IT, Cordeiro Q, Shiozawa P (2017) Lavender oil preparation (Silexan) for treating anxiety: an updated meta-analysis. J Clin Psychopharmacol 37:115–117
Gomez AF, Barthel AL, Hofmann SG (2018) Comparing the efficacy of benzodiazepines and serotonergic anti-depressants for adults with generalized anxiety disorder: a meta-analytic review. Expert Opin Pharmacother 19:883–894
Griebel G, Holmes A (2013) 50 years of hurdles and hope in anxiolytic drug discovery. Nat Rev Drug Discov 12:667–687
Grigorova O (2009) P01–156 Estimation of placebo effect in therapy of generalized anxiety disorder. Eur Psychiatry 24:S544
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55
Harris MG, Hobbs MJ, Burgess PM, Pirkis JE, Diminic S, Siskind DJ, Andrews G, Whiteford HA (2015) Frequency and quality of mental health treatment for affective and anxiety disorders among Australian adults. Med J Aust 202:185–189
Heger-Mahn D, Pabst G, Dienel A, Schläfke S, Klipping C (2014) No interacting influence of lavender oil preparation silexan on oral contraception using an ethinyl estradiol/levonorgestrel combination. Drugs R D 14:265–272
Hidalgo RB, Tupler LA, Davidson JR (2007) An effect-size analysis of pharmacologic treatments for generalized anxiety disorder. J Psychopharmacol 21:864–872
Kang H-J, Nam ES, Lee Y, Kim M (2019) How strong is the evidence for the anxiolytic efficacy of lavender?: Systematic review and meta-analysis of randomized controlled trials. Asian Nurs Res (Korean Soc Nurs Sci) 13:295–305
Kasper S (2006) Anxiety disorders: under-diagnosed and insufficiently treated. Int J Psychiatry Clin Pract 10:3–9
Kasper S (2015) Phytopharmaceutical treatment of anxiety, depression, and dementia in the elderly: evidence from randomized, controlled clinical trials. Wien Med Wochenschr 165:217–228
Kasper S, Anghelescu I, Dienel A (2015) Efficacy of orally administered Silexan in patients with anxiety-related restlessness and disturbed sleep—a randomized, placebo-controlled trial. Eur Neuropsychopharmacol 25:1960–1967
Kasper S, Dienel A (2015) Effects of Silexan on daily living skills and health related quality of life in patients with generalized anxiety disorder—results from a randomized, double-blind, placebo controlled trial, Annual Congress of the German Society for Psychiatry and Psychotherapy (DGPPN), Berlin, Germany
Kasper S, Gastpar M, Müller WE, Volz H-P, Möller H-J, Dienel A, Schläfke S (2010) Silexan, an orally administered Lavandula oil preparation, is effective in the treatment of “subsyndromal” anxiety disorder: a randomized, double-blind, placebo controlled trial. Int Clin Psychopharmacol 25:277–287
Kasper S, Gastpar M, Müller WE, Volz H-P, Möller H-J, Schläfke S, Dienel A (2014) Lavender oil preparation Silexan is effective in generalized anxiety disorder—a randomized, double-blind comparison to placebo and paroxetine. Int J Neuropsychopharmacol 17:859–869
Kasper S, Möller H-J, Volz H-P, Schläfke S, Dienel A (2017) Silexan in generalized anxiety disorder: investigation of the therapeutic dosage range in a pooled data set. Int Clin Psychopharmacol 32:195–204
Kasper S, Müller WE, Volz H-P, Möller H-J, Koch E, Dienel A (2018) Silexan in anxiety disorders: clinical data and pharmacological background. World J Biol Psychiatry 19:412–420
Kasper S, Volz H-P, Dienel A, Schläfke S (2016) Efficacy of Silexan in mixed anxiety-depression—a randomized, placebo-controlled trial. Eur Neuropsychopharmacol 26:331–340
Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M (2014) Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry 14(Suppl. 1):S1
Kehr J, Yoshitake T, Koch E, Noeldner M (2010) Effects of intraperitoneal administration of Silexan, an essential oil from flowers of Lavandula angustifolia on extracellular levels of noradrenaline, dopamine and serotonin in the prefrontal cortex of freely moving rats. Planta Med 76:1316
Maier W, Buller R, Philipp M, Heuser I (1988) The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord 14:61–68
Matza LS, Morlock R, Sexton C, Malley K, Feltner D (2010) Identifying HAM-A cutoffs for mild, moderate, and severe generalized anxiety disorder. Int J Methods Psychiatr Res 19:223–232
Möller H-J, Volz H-P, Dienel A, Schläfke S, Kasper S (2019) Efficacy of Silexan in subthreshold anxiety: meta-analysis of randomised, placebo-controlled trials. Eur Arch Psychiatry Clin Neurosci 269:183–193
Möller H-J, Volz H-P, Seifritz E, Müller H, Kenntner-Mabiala R, Kaussner Y, Schoch S, Kasper S (2021) Silexan does not affect driving performance after single and multiple dose applications: results from a double-blind, placebo and reference-controlled study in healthy volunteers. J Psychiatr Res 136:543–551
Müller WE, Sillani G, Schuwald A, Friedland K (2021) Pharmacological basis of the anxiolytic and antidepressant properties of Silexan®, an essential oil from the flowers of lavender. Neurochem Int 143:104899
National Institute for Health and Care Excellence (NICE) (2019) Generalised anxiety disorder and panic disorder in adults: management
National Institute of Mental Health (1970) 12—CGI. Clinical global impressions. In: Guy W (ed) EDCEU assessment in psychopharmacology. U.S. National Institute of Mental Health, Psychopharmacology Research Branch, Rockville, Md., pp 217–222
Pies RW (2019) Antidepressant discontinuation: a tale of two narratives. J Clin Psychopharmacol 39:185–188
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 340:c221
Rutherford BR, Bailey VS, Schneier FR, Pott E, Brown PJ, Roose SP (2015) Influence of study design on treatment response in anxiety disorder clinical trials. Depress Anxiety 32:944–957
Sartori SB, Singewald N (2019) Novel pharmacological targets in drug development for the treatment of anxiety and anxiety-related disorders. Pharmacol Ther 204:107402
Satpute AB, Mumford JA, Naliboff BD, Poldrack RA (2012) Human anterior and posterior hippocampus respond distinctly to state and trait anxiety. Emotion 12:58–68
Sayed AM, Morsy S, Tawfik GM, Naveed S, Minh-Duc NT, Hieu TH, Ali ZA, Shinkar A, Doheim MF, Hashan MR, Huy NT (2020) The best route of administration of lavender for anxiety: a systematic review and network meta-analysis. Gen Hosp Psychiatry 64:33–40
Schjerning O, Pottegard A, Damkier P, Rosenzweig M, Nielsen J (2016) Use of Pregabalin—a nationwide pharmacoepidemiological drug utilization study with focus on abuse potential. Pharmacopsychiatry 49:155–161
Schuwald AM, Nöldner M, Wilmes T, Klugbauer N, Leuner K, Müller WE (2013) Lavender oil-potent anxiolytic properties via modulating voltage dependent calcium channels. PLoS ONE 8:e59998
Seifritz E, Möller H-J, Volz H-P, Müller WE, Hopyan T, Wacker A, Schläfke S, Kasper S (2021) No abuse potential of Silexan in healthy recreational drug users: a randomized controlled trial. Int J Neuropsychopharmacol 24:171–180
Seifritz E, Schläfke S, Holsboer-Trachsler E (2019) Beneficial effects of Silexan on sleep are mediated by its anxiolytic effect. J Psychiatr Res 115:69–74
Ströhle A, Gensichen J, Domschke K (2018) The diagnosis and treatment of anxiety disorders. Dtsch Arztebl Int 115:611–620
Volz H-P, Saliger J, Kasper S, Möller H-J, Seifritz E (2021) Subsyndromal generalised anxiety disorder: operationalisation and epidemiology—a systematic literature survey. Int J Psychiatry Clin Pract 27:1–10
von Känel R, Kasper S, Bondolfi G, Holsboer-Trachsler E, Hättenschwiler J, Hatzinger M, Imboden C, Heitlinger E, Seifritz E (2021) Therapeutic effects of Silexan on somatic symptoms and physical health in patients with anxiety disorders: a meta-analysis. Brain Behav 11:e01997
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Yap WS, Dolzhenko AV, Jalal Z, Hadi MA, Khan TM (2019) Efficacy and safety of lavender essential oil (Silexan) capsules among patients suffering from anxiety disorders: a network meta-analysis. Sci Rep 9:18042
Zhang W, Yan Y, Wu Y, Yang H, Zhu P, Yan F, Zhao R, Tian P, Wang T, Fan Q, Su Z (2022) Medicinal herbs for the treatment of anxiety: a systematic review and network meta-analysis. Pharmacol Res 179:106204
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Zung WW (1971) A rating instrument for anxiety disorders. Psychosomatics 12:371–379
Acknowledgements
Medical writing support was provided by Andreas Völp (psy consult scientific services, Hamburg, Germany).
Funding
Open access funding provided by Medical University of Vienna. This research and its publication were financially supported by Dr. Willmar Schwabe GmbH & Co. KG, Karlsruhe, Germany, manufacturer of Silexan.
Author information
Authors and Affiliations
Contributions
All authors designed the study. SS undertook the statistical analysis. All authors contributed to the interpretation of data and drafting of the manuscript. All authors critically revised the manuscript and gave their final approval for submission.
Corresponding author
Ethics declarations
Conflict of interest
MD has received travel grants and consultant/speaker honoraria from Medizin Medien Austria and Janssen. Within the last three years, LB has received travel grants and consultant/speaker honoraria from Medizin Medien Austria, Universimed, Schwabe Austria, Janssen and Angelini. Within the last three years, HPV has served as a consultant or on advisory boards for Astra/Zeneca, Eli Lilly, Lundbeck, Pfizer, Schwabe, Janssen, Otsuka, Angelini, and Sage and has served on speakers’ bureaus for Astra/Zeneca, Eli Lilly, Lundbeck, Schwabe, Janssen, Bayer, Recordati and neuraxpharm. ES received in the last three years honoraria and grants for advice and educational lectures from Lundbeck Switzerland, Schwabe Switzerland and Germany, Janssen Switzerland, Otsuka Switzerland, Mepha Pharma Switzerland, Otsuka Pharma Switzerland, Ricordati Switzerland and Sunovion Pharma UK and Angelini. HJM has received grant/research support, consulting fees and honoraria within the last years from AstraZeneca, Lundbeck, Otsuka, and Schwabe. SS is employee of Dr. Willmar Schwabe GmbH & Co. KG. SK has received grant/research support from Lundbeck; he has served as a consultant or on advisory boards for Angelini, Biogen, Esai, Janssen, IQVIA, Lundbeck, Mylan, Recordati, Sage and Schwabe; and he has served on speakers bureaus for Aspen Farmaceutica S.A., Angelini, Biogen, Janssen, Lundbeck, Neuraxpharma, Recordati, Sage, Sanofi, Schwabe, Servier and Sun Pharma.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dold, M., Bartova, L., Volz, HP. et al. Efficacy of Silexan in patients with anxiety disorders: a meta-analysis of randomized, placebo-controlled trials. Eur Arch Psychiatry Clin Neurosci 273, 1615–1628 (2023). https://doi.org/10.1007/s00406-022-01547-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-022-01547-w