Abstract
Introduction
Due to favorable antidepressant (AD) efficacy and tolerability, selective-serotonin reuptake inhibitors (SSRIs) are consistently recommended as substances of first choice for the treatment of major depressive disorder (MDD) in international guidelines. However, little is known about the real-world clinical correlates of patients primarily prescribed SSRIs in contrast to those receiving alternative first-line ADs.
Methods
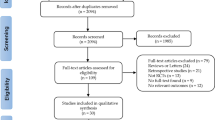
These secondary analyses are based on a naturalistic, multinational cross-sectional study conducted by the European Group for the Study of Resistant Depression at ten research sites. We compared the socio-demographic and clinical characteristics of 1410 patients with primary MDD, who were either prescribed SSRIs or alternative substances as first-line AD treatment, using chi-squared tests, analyses of covariance, and logistic regression analyses.
Results
SSRIs were prescribed in 52.1% of MDD patients who showed lower odds for unemployment, current severity of depressive symptoms, melancholic features, suicidality, as well as current inpatient treatment compared to patients receiving alternative first-line ADs. Furthermore, patients prescribed SSRIs less likely received add-on therapies including AD combination and augmentation with antipsychotics, and exhibited a trend towards higher response rates.
Conclusion
A more favorable socio-demographic and clinical profile associated with SSRIs in contrast to alternative first-line ADs may have guided European psychiatrists’ treatment choice for SSRIs, rather than any relevant pharmacological differences in mechanisms of action of the investigated ADs. Our results must be cautiously interpreted in light of predictable biases resulting from the open treatment selection, the possible allocation of less severely ill patients to SSRIs as well as the cross-sectional study design that does not allow to ascertain any causal conclusions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective-serotonin reuptake inhibitors (SSRIs) represent a very well studied class of antidepressant (AD) medication that is consistently recommended as the first-line psychopharmacotherapy for major depressive disorder (MDD) in clinical practice guidelines (CPG) throughout the world [25]. Accordingly, it is not surprising that SSRIs are the most commonly prescribed ADs in numerous patient populations with different ethnical and geographical backgrounds [2, 21, 27, 29, 46].
Despite the frequency of SSRIs prescriptions, rather heterogeneous conclusions were drawn in terms of efficacy. While SSRIs, particularly sertraline and escitalopram, were meta-analytically evidenced as gold standard ADs in MDD [12], other publications reported no substantial difference between SSRIs and other ADs [26]. The largest and most recent network meta-analysis (NMA) comprising over 116,000 patients reported rather small differences between the 21 investigated ADs that all performed better than placebo [11]. The SSRIs escitalopram and paroxetine, along with agents with a different mode of action, were, however, among the most efficacious, whereas the opposite was found for fluoxetine and fluvoxamine. Acceptability in that study was comparable between the studied ADs. As for individual SSRIs, escitalopram, citalopram, sertraline, and fluoxetine exhibited the lowest drop-out rates, while fluvoxamine the highest [11].
The efficacy and acceptability of SSRIs in MDD treatment may be only two of the important aspects influencing treatment choice. In spite of potential adverse effects (AE) that are most frequently related to the gastrointestinal tract and sexual dysfunction [10], SSRIs were repeatedly suggested to be less toxic in overdose and thus safer when compared to other drugs including the most ADs, especially tricyclic ADs (TCAs), but also more recently introduced AD substances as serotonin and norepinephrine reuptake inhibitors (SNRIs) and the noradrenergic and specific serotonergic AD (NaSSA) mirtazapine [31, 56]. Furthermore, previous studies underscored that SSRIs exhibit beneficial effects on life quality [36], cognitive functioning [63], and reduce relapse risk [13].
Although valuable knowledge on efficacy, tolerability and further important aspects distinguishing SSRIs from other ADs in MDD treatment could be retrieved from randomized-controlled trials (RCTs) and meta-analyses, extrapolation to real-world conditions found in everyday clinical practice is challenging, because of the manifold presentation of MDD which may vary in severity and course and which may include suicidality, psychotic-, melancholic- and atypical features, and/or comorbidities. Therefore, factors that may mediate clinicians’ choices to administer SSRIs over other ADs as first-line ADs in MDD in real-world settings are of interest. To shed light on these aspects, we aimed to illustrate the real-world prescription rates of SSRIs and other AD substances administered as first-line psychopharmacotherapy in 1410 MDD patients from Europe and Israel, and to reveal possible differences in their socio-demographic and clinical patterns.
Materials and methods
Study concept
The current analyses refer to the international and multicentric, observational, cross-sectional and non-interventional study with retrospective assessment of treatment response conducted by the European Group for the Study of Resistant Depression (GSRD) [3]. These secondary analyses are based on the GSRD project “Clinical and biological correlates of resistant depression and related phenotypes” performed from 2011 to 2016 at ten research centers (Vienna, Brussels, Toulouse, Elancourt, Halle, Athens, Bologna, Siena, Geneva and Tel Hashomer) in seven European countries and Israel. The design and all procedures of the GSRD study, which were introduced and comprehensively described in our previous reports [3], were approved by the ethics committees of each participating site.
Study collective
Adult in- and outpatients of both sexes were recruited in academic as well as non-academic clinical routine centers in Austria, Belgium, France, Germany, Greece, Italy, Switzerland, and Israel that are mentioned above. In case of interest and eligibility for participation in the present study, all related procedures were thoroughly explained to the patients before signing written informed consent. To be included in the present study, the patients had to be diagnosed with a current single or recurrent major depressive episode (MDE) occurring in the course of MDD as their primary psychiatric diagnosis. Furthermore, they had to undergo an adequate psychopharmacotherapy with at least one AD agent employed in sufficient daily doses and treatment duration of minimally four weeks during the current MDE [3, 19]. The exclusion criteria comprised any primary psychiatric diagnosis other than MDD and co-occurring severe personality disorders and/or substance use disorders (except nicotine and/or caffeine) present six months before study enrollment. Other psychiatric and/or somatic comorbidities and potential additional features as psychotic and/or melancholic features and/or suicidality occurring during the current MDE were not excluded to ensure the naturalistic real-world conditions [3].
Clinical assessment
To assure a high standard of data quality and inter-rater reliability, exclusively experienced psychiatrists undergoing specific rater trainings were allowed to assess socio-demographic, clinical, and treatment patterns of the enrolled MDD patients who were treated by senior consultants for psychiatry in all recruiting centers. In the course of a comprehensive clinical assessment, medical records of the included MDD patients were considered and the Mini International Neuropsychiatric Interview (MINI) [68] was applied to establish the primary psychiatric diagnosis according to the DSM-IV-TR criteria [73], the presence of potential additional specific features occurring during the current MDE, and/or psychiatric comorbidities. Furthermore, all administered treatments during the current MDE including the first-line AD treatment representing the initial AD agent were thoroughly assessed at study entry and documented accordingly. To measure depressive symptoms at study entry, reflecting a time-point after at least four weeks of adequate AD treatment, the 21-item Hamilton Rating Scale for Depression (HAM-D) [30] and the Montgomery and Åsberg Depression Rating Scale (MADRS; current MADRS, cMADRS) [58] were employed. To estimate the extent of depressive symptoms at the onset of the current MDE, reflecting a time-point prior to initiation of the first-line AD treatment that was minimally four weeks before study inclusion, the so-called retrospective MADRS (rMADRS) was calculated based on the MDD patients’ assertions and their medical records.
To determine treatment response patterns based on the GSRD staging model [3], the MADRS total score change (rMADRS–cMADRS) was calculated after at least one adequate AD trial administered during the current MDE. Accordingly, treatment response was defined by a cMADRS total score of < 22 and a ≥ 50% reduction of the MADRS total score after an AD trial of adequate daily dosing and duration lasting at least four weeks. A total cMADRS score of ≥ 22 and a < 50% MADRS total score reduction after one adequate AD trial was mandatory to categorize treatment non-response. Treatment resistance was determined as a non-response to two or more consecutive AD trials that were each administered in adequate daily dosing and duration during the current MDE [3].
In analogy to existing evidence, the current suicidal risk and its extent were ascertained according to the HAM-D item 3 that specifically assesses suicidality [17, 42]. Where applicable, low suicidality levels were reflected by the item-score of 1, while moderate to high degree of the current suicidal risk was depicted by the item-scores 2–4.
Statistical computations
The enrolled 1410 patients suffering from primary MDD [3] were subdivided into two groups according to their first-line AD treatment with either SSRIs or alternative AD substances that was administered during the current MDE. Hereby, their socio-demographic and clinical patterns were represented with descriptive statistics (means, standard deviation (SD), and/or percentages) and, subsequently, dichotomously compared (Table 1). The initial analyses included chi-squared tests and analyses of covariance (ANCOVAs) for categorical and continuous variables, respectively. For ANCOVAs, the prescribed first-line AD treatment was included as fixed effect and recruitment center as covariate. The Bonferroni correction for multiple comparisons was applied in our initial analyses, whereby the alpha level, that was originally set at < 0.05, was further adjusted according to the number of variables tested (n = 50). Accordingly, the alpha level was set at = 0.001 (0.05/50 = 0.001). Uncorrected p values are displayed in Table 1, whereby statistical significance after the abovementioned correction for multiple tests is indicated in bold. Binary logistic regression analyses with the relevant independent variables withstanding the Bonferroni correction for multiple comparisons in our initial analyses were performed post hoc to quantify their association with the respective first-line AD treatment that represented the dichotomous dependent variable. The recruitment center served as covariate in the post hoc binary logistic regression analyses (Table 2), whereby the Bonferroni correction for multiple comparisons was applied in analogy to our initial analyses (α = 0.001). Data were analyzed employing the version 27 of IBM SPSS Statistics.
Results
The total sample included 1410 MDD patients [3] who were treated with either SSRIs (n = 734, 52.1%) or other AD substances (n = 676, 47.9%) including SNRIs (n = 336), noradrenergic-dopamine reuptake inhibitors (NDRIs; n = 32), NaSSAs (n = 121), serotonin antagonist and reuptake inhibitors (SARIs; n = 28), noradrenaline reuptake inhibitors (NARIs; n = 3), TCAs (n = 74), monoamine oxidase inhibitors (MAOIs; n = 5), agomelatine (n = 69), tianeptine (n = 2), and vortioxetine (n = 6) as their first-line AD psychopharmacotherapy during their current MDE. With respect to the individual SSRIs, all six existing substances were distributed in our MDD patients, whereby the majority received escitalopram (n = 257) that was followed by sertraline (n = 163), paroxetine (n = 126), fluoxetine (n = 97), citalopram (n = 71), and fluvoxamine (n = 20; Fig. 1).
Individual substances administered in 734 MDD patients treated with SSRIs as their first-line AD treatment. Displayed cumulative percentages refer to the individual SSRIs administered as first-line AD treatment in 734 MDD patients. AD antidepressant, MDD major depressive disorder, SSRIs selective serotonin reuptake inhibitors
The socio-demographic and clinical patterns of the whole sample were comprehensively described in our previous reports and are shown in Table 1 [3]. Table 1 further displays the respective characteristics of the two patient groups split according to their first-line treatment with either SSRIs or other AD substances, and the identified between-group differences. The results of our post hoc binary logistic regression analyses reflecting the association between the administered first-line AD treatment and parameters for which significant between-group contrasts were observed in our initial analyses are depicted in Table 2. Exclusively robust statistical parameters derived from our initial analyses are provided below (p values remaining significant in our initial analyses after our correction for multiple testing).
MDD patients who underwent first-line AD treatment with SSRIs during their current MDE showed lower odds for unemployment as compared to their counterparts receiving other agents (48.4% vs 58.4%, p < 0.001). The current occurrence of melancholic features (54.5% vs 67.5%, p < 0.001) and suicidal risk (40.1% vs 52.5%, p < 0.001; Fig. 2) was less frequent in patients treated with first-line SSRIs in relation to those with other substances. Patients receiving SSRIs were less frequently treated as inpatients during their current MDE (25.2% vs 44.8%, p < 0.001). The severity of depressive symptoms measured with the MADRS at onset of the current MDE (mean rMADRS total score 33.1 ± 7.7 vs 35.1 ± 7.6, p < 0.001) as well as at study entry (mean cMADRS total score 23.2 ± 11.4 vs 26.1 ± 11.0, p < 0.001) was lower in this subgroup than in patients receiving alternative agents. While response to the first-line AD treatment occurred more frequently in patients treated with SSRIs (28.5% vs 20.3%), TRD was diagnosed more commonly in patients with alternative first-line AD psychopharmacotherapy (35.0% vs 46.6%, p < 0.001; Fig. 3).
The current suicidal risk of MDD patients receiving either SSRIs or other substances as their first-line AD treatment. Displayed cumulative percentages refer to the proportion of MDD patients receiving either SSRIs (n = 737; 52.1%; red colored) or alternative substances (n = 676; 47.9%; blue colored) as their first-line AD treatment itemized according to the current suicidal risk and its extent that were ascertained according to the HAM-D item 3 that is exclusively dedicated to suicidality [17]. While the absence of the current suicidal risk was reflected by the item-score of 0 (absent), its presence was represented by item-scores of 1 (feels life is not worth living), 2 (wishes to be dead or any thoughts of possible death to self), 3 (suicide ideas or gestures) or 4 (suicide attempts). While significant between-group differences were detected in terms of the presence of the current suicidal risk (p < 0.001), MDD patients receiving first-line SSRIs did not significantly differ from their counterparts with respect to its extent (p = 0.214). AD antidepressant, HAM-D Hamilton Depression Rating Scale, MDD major depressive disorder, SSRIs = selective serotonin reuptake inhibitors
Treatment outcome patterns in MDD patients receiving either SSRIs or other substances as their first-line AD treatment. Displayed cumulative percentages refer to the proportion of MDD patients receiving either SSRIs (n = 737; 52.1%; red colored) or alternative substances (n = 676; 47.9%; blue colored) as their first-line AD treatment itemized according to their treatment outcome patterns reflecting response, non-response and TRD that differed significantly between both patient groups in our initial analyses (p < 0.001). While non-response was defined by a previous single failed AD trial, at least two failed AD trials were mandatory for TRD. AD antidepressant; MDD major depressive disorder; SSRIs selective serotonin reuptake inhibitors, TRD treatment resistant depression
In terms of the administered therapeutic strategies during the current MDE, patients taking SSRIs received a lower mean number of psychopharmacotherapeutics (2.0 ± 1.2 vs 2.4 ± 1.3, p < 0.001) and underwent additional psychotherapy (27.1% vs 35.8%, p < 0.001) less frequently than patients treated with other first-line ADs. Psychopharmacotherapeutic augmentation and/or combination strategies in general (54.8% vs 67.0%, p < 0.001) and augmentations with at least one antipsychotic (AP) agent (21.7% vs 30.0%, p < 0.001), and combination treatment with at least one additional AD (24.0% vs 35.5%, p < 0.001) in particular were less commonly prescribed in patients treated with first-line SSRIs as compared to their counterparts.
The aforementioned between-group contrasts remained significant in our post hoc binary logistic regression analyses with exception of the associations between first-line AD treatment with SSRIs and treatment outcome (p = 0.012) as well as employment of additional psychotherapy (p = 0.019; Table 2).
Discussion
In the present multinational and naturalistic cross-sectional secondary investigation, about half of the included MDD patients (52.1%) received SSRIs as their first-line AD treatment during their current MDE, while the remaining group was treated with alternative ADs. Patients receiving SSRIs exhibited a favorable socio-demographic and clinical profile with reduced odds for unemployment and for additional features occurring during the current MDE such as melancholia and suicidality. Furthermore, they also showed reduced odds for current inpatient treatment and for additional therapeutic strategies including combination with other ADs and augmentation with APs. Importantly, patients undergoing first-line AD treatment with SSRIs exhibited a lower severity of depressive symptoms at the onset of the current MDE as well as at study inclusion. A trend towards higher rates of treatment response was observed in patients with SSRIs, while treatment resistance occurred trend-wise more commonly in patients taking alternative first-line ADs.
Our findings of preferred first-line treatment with ADs other than SSRIs in melancholic depression, that are in line with available international evidence, may reflect common clinical prescription practice in a severe MDD subtype with specific clinical manifestations and related neurobiological correlates [16, 52]. Specifically, patients with melancholia were previously shown to respond less to placebo and psychotherapeutic and psychosocial treatments [61], whereas rapid and better outcomes following biological treatments comprising ADs or electroconvulsive therapy were observed [60, 62]. In fact, a lately published meta-analytical report revealed that patients with melancholia in MDD appear to achieve a greater reduction of their symptoms with antidepressant treatment but also with placebo compared to those lacking these features [38]. Further, recent evidence reported differential response rates among several classes of ADs, whereby SSRIs seemed to be less efficacious than other ADs, especially TCAs [70, 71]. With respect to current treatment guidelines, exclusively the American Psychiatric Association specifically advises TCAs and SNRIs in the treatment of melancholic depression in their CPGs [25].
The lower proportion of SSRI prescriptions in MDD patients exhibiting current suicide risk is worth mentioning, since suicidality represents a major burden in MDD [39] that must be considered and regularly assessed in each patient, and since warnings on the provocation of suicidality with SSRIs were propagated previously. The question of AD agents including SSRIs and suicide risk in clinical trials has been subject to a vigorous scientific debate with disparate results and conclusions that often yielded from differential methodological analyses of the same data sets [33, 34, 40, 47]. Importantly, epidemiological data clearly displayed a reduction of suicides parallel to an increase of prescriptions of ADs and might, thus, more likely reflect the real-world situation of the respective risk inherent to this type of psychopharmacotherapy [14]. Hereby, the latter study results highlight that suicidality represents one of the most frequent and serious symptoms occurring during MDEs per se rather than a treatment-related consequence. Our data might be a demonstration that clinicians are reluctant to primarily prescribe SSRIs in patients who exhibit suicidal thoughts or ideations because of the exemplified controversial scientific discussion that used to be extensively reported in mainstream, non-scientific media. It is a well-known phenomenon that ADs acting via the reuptake inhibition of serotonin bear the potential to induce agitation or restlessness after their initiation [8]. It is, however, noteworthy in this context that the redoubtable related suicidal behavior is very well avoidable with adequate therapeutic strategies including co-administration of agents with tranquilizing effects and/or inpatient treatment setting and might be, hence, of clinical relevance exclusively in case of inadequate treatment [1, 5, 17, 57, 67].
The observed lower prescription rates of SSRIs in suicidal MDD patients might as well refer to the fact that suicidality was repeatedly associated with chronicity as well as treatment resistant depression (TRD) and/or difficult-to-treat depression (DTD) [3, 17, 54] representing conditions, where AD agents with different mode of action, such as the MAOI tranylcypromine for instance, are preferably recommended in international treatment algorithms for MDD [49]. Furthermore, the NaSSA mirtazapine, that showed a faster onset in comparison to other ADs in several studies, was suggested as a noteworthy alternative consideration of initiating a first-line AD especially in MDD patients suffering from suicidality [6, 7, 42]. Even though not evaluated in our trial, the potent AD as well as anti-suicidal effects of esketamine have to be mentioned in this context, as this compound has an important field of application in this indication due to a very rapid AD onset of action [50, 51, 55, 72].
Our further associations between first-line SSRI treatment and a lower severity of depressive symptoms during the current MDE and a lesser need for current and/or previous inpatient treatment support our consensus postulating that a rather favorable disease profile may serve as a possible variable guiding clinicians’ treatment choice towards SSRIs. Another possible reason for the observed prescription rationale may have derived from evidence postulating a varying effectiveness of SSRIs in dependence of the severity of depressive symptoms [59]. Importantly, while a negative relationship between baseline severity of depressive symptoms and response to SSRIs was found in meta-analyses by some authors [23], others came to contrary conclusions [22]. Most recently, one of the largest and comprehensive patient-level investigations was able to deliver compelling evidence that SSRIs are efficacious in the whole spectrum from mild to severe depression by applying a different, coherent methodological approach, e.g. an item-based analysis [35].
In terms of treatment outcome, our results revealed a trend towards higher response rates in MDD patients treated with SSRIs as first-line AD treatment, while the prescription of ADs with different modes of action were associated with a trend towards treatment resistance. Being aware of existing international evidence on AD efficacy in MDD favoring alternative AD substances over SSRIs and vice versa [9, 15, 37, 59] as well as individual agents within the SSRI substance class [43], the largest NMAs dedicated to this topic suggested comparable AD potency of over 20 commonly prescribed ADs [11]. However, the highly selective patient populations derived from RCTs and the fact that conclusions from NMA about efficacy and/or tolerability of ADs are not equal to direct head to head comparisons [45] limit their overall explanatory power. Given the cross-sectional nature of our study with retrospective evaluation of treatment outcome, we cannot assume any difference in the efficacy of SSRIs compared to other AD classes with certainty. A possible bias resulting of allocating less severely ill patients to SSRIs rather than other ADs may have affected our results. To sum up, our naturalistic data may primarily represent a valuable contribution revealing a real-world AD prescription culture rather than providing any information about efficacy of the administered compounds.
The significantly reduced odds for add-on treatments including AD combinations and augmentation with APs in MDD patients who received SSRIs might represent complementary results highlighting that a further therapeutic escalation is inevitable in case of insufficient response to first-line ADs, that in general affects a considerable number of MDD patients worldwide [3, 5, 18, 48, 49] and that was more commonly encountered in our patients receiving alternative first-line substances. The trend-wise less frequently employed additional psychotherapies might go along with the fact that patients who achieve response or even remission under their first-line AD treatment, which consists of SSRIs in the most cases [5, 19, 64], more likely forgo additional psychotherapy for various reasons [4, 28].
Higher rates of unemployment in MDD patients receiving first-line ADs other than SSRIs represented our only significant between-group contrast in terms of socio-demographic aspects and was mostly interpreted in the context of illness severity as well as functional impairment that was more pronounced in our patients with alternative first-line ADs. Precisely, patients showing a lower severity of depressive symptoms as well as less functional impairment may predominantly have been allocated to SSRI first-line medication. The latter assumption might be supported by available international data reporting positive effects of different individual SSRIs and other classes of ADs on workplace functioning [53].
Noteworthy strengths of the present study are the naturalistic design and the large international sample which may best possibly reflect the broad everyday routine. In contrast to the most RCTs, such real-world patient population gathered from in- and outpatient units of university as well as non-academic centers in eight countries allows investigations of heterogeneous clinical manifestations of MDD including suicidality, psychotic features, psychiatric and/or somatic comorbidities, and varying disease course and severity ranging from single to recurrent MDEs with mild, moderate or severe extent of current depressive symptoms. However, potential cross-site differences of the prescription practice, driven by the type of recruiting institution (academic vs. non-academic), divergent insurance situations as well as availabilities and approvals of the specific psychopharmacotherapeutics which might have arisen by recruitments in different European countries, cannot be fully ruled out. To minimize a distortion of our result in these regards, the variable “research center” was accounted for in our statistical analyses. Furthermore, physician-related factors as exact number of years of their experience, which may have influenced treatment patterns and the findings, respectively, were not systematically assessed. To minimize potential biases related to the latter aspects and to assure a high standard of data quality and inter-rater reliability, exclusively experienced psychiatrists undergoing specific rater trainings were allowed to perform the comprehensive clinical assessments of the enrolled MDD patients who were treated by senior consultants for psychiatry in all recruiting centers. Furthermore, the present large multi-site project conducted by the GSRD [3, 66, 69] was primarily designed to elucidate clinical and genetic aspects of TRD, whereby the current secondary analyses focusing on the first-line AD treatment and the related socio-demographic and clinical characteristics represent an additional aspect which bears potential limitations.
Furthermore, the open treatment design may be subject to bias regarding assessment and allocation. The fact that about a half of the included 1410 MDD patients received SSRIs as first-line psychopharmacotherapy and a comparable group of patients was treated with other ADs bears the limitation of relatively small proportions of AD agents that were individually prescribed in the group of patients receiving alternative ADs. This led us not to differentiate between the distinct individual ADs to enable investigations of comparable groups of MDD patients. Similarly, we did not differentiate between the individual SSRIs, which we deem justifiable in light of the fact that superiority of a specific substance could not be demonstrated with certainty and due to the unequal proportion of MDD patients treated with the respective individual SSRIs. While exclusively conventional on-label substances were involved in the current investigation, novel psychopharmacotherapeutic options that have recently been shown to be very effective and, hence, approved in MDD and/or TRD, as esketamine for instance [41, 44, 49, 65], have not yet been considered. Furthermore, it is noteworthy that the psychopharmacotherapeutic terminology applied in our work is based on the traditional indication-based nomenclature to ensure an unhampered interpretability and comparison to available international literature, even though we are very well aware of a new classification system that is increasingly replacing the current terminology. The so-called Neuroscience-based Nomenclature (NbN) is driven by the pharmacological profiles of the individual substances and is, hence, thought to support rational and lucid prescribing with the goal to increase therapeutic adherence of the patients [24, 74].
Most importantly, it has to be pointed out that the cross-sectional design of the study does not allow to ascertain any causal conclusions and, hence, represents an explicit limitation. Clearly acknowledging that this procedure yields less accurate results than prospective investigations, we would like to highlight our treatment outcome measures that were calculated according to the total score reduction between the rMADRS, referring to a time-point when the depressive symptoms reached their maximum (minimally 4 weeks prior inclusion), and the cMADRS, representing a time-point of study entry (at least after four weeks of an adequate psychopharmacotherapy). The respective variables reflecting a reduction of depressive symptoms during the current MDE might be, hence, regarded as longitudinal measures providing hints towards causality. We are aware that this approach is inferior to randomized-controlled, prospective conditions; however, in light of the fact that MDD patients were previously shown to adequately recall symptoms for a considerable period of time [20] and that many rating scales consider symptoms of MDD retrospectively, we deem our procedure justifiable. Additionally, to minimize such associated bias, all our raters were experienced psychiatrists undergoing extensive training in the respective scales.
Conclusion
The observed beneficial socio-demographic and clinical profile associated with first-line SSRI administration in contrast to the rather inferior characteristics related to alternative substances may reflect broad adherence of European psychiatrists to the current international treatment algorithms suggesting SSRIs for the initial treatment approach in MDD, while AD substance classes like MAOIs or TCAs are recommended once sufficient treatment response could not be achieved [49]. Furthermore, clinicians may deem SSRIs less appropriate in treating psychopathological features as suicidality and/or melancholia, which may partly result from previous evidence reflecting conflicting or ambiguous findings. The fact that the abovementioned contrasts between patients receiving SSRIs and other substances were identified in the course of a cross-sectional retrospective study with an open selection of either treatment leads us to interpret them as very useful variables to understand the criteria guiding the choice of the first-line AD in MDD in real-world settings, rather than they may reflect any relevant pharmacological differences in mechanisms of action of the investigated ADs.
References
Akiskal HS, Benazzi F, Perugi G, Rihmer Z (2005) Agitated “unipolar” depression re-conceptualized as a depressive mixed state: Implications for the antidepressant-suicide controversy. J Affect Disord 85:245–258
Ball S, Classi P, Dennehy EB (2014) What happens next? A claims database study of second-line pharmacotherapy in patients with major depressive disorder (mdd) who initiate selective serotonin reuptake inhibitor (SSRI) treatment. Ann Gen Psychiatry 13:8
Bartova L, Dold M, Kautzky A, Fabbri C, Spies M, Serretti A, Souery D, Mendlewicz J, Zohar J, Montgomery S, Schosser A, Kasper S (2019) Results of the european group for the study of resistant depression (gsrd)—basis for further research and clinical practice. World J Biol Psychiatry 20:427–448
Bartova L, Fugger G, Dold M, Swoboda MMM, Zohar J, Mendlewicz J, Souery D, Montgomery S, Fabbri C, Serretti A, Kasper S (2021) Combining psychopharmacotherapy and psychotherapy is not associated with better treatment outcome in major depressive disorder—evidence from the european group for the study of resistant depression. J Psychiatr Res 141:167–175
Bauer M, Severus E, Möller HJ, Young AH, WFSBP Task Force on Unipolar Depressive Disorders (2017) Pharmacological treatment of unipolar depressive disorders: summary of WFSBP guidelines. Int J Psychiatry Clin Pract 21(3):166–176
Behnke K, Sogaard J, Martin S, Bauml J, Ravindran AV, Agren H, Vester-Blokland ED (2003) Mirtazapine orally disintegrating tablet versus sertraline: A prospective onset of action study. J Clin Psychopharmacol 23:358–364
Benkert O, Szegedi A, Kohnen R (2000) Mirtazapine compared with paroxetine in major depression. J Clin Psychiatry 61:656–663
Bigos KL, Pollock BG, Aizenstein HJ, Fisher PM, Bies RR, Hariri AR (2008) Acute 5-ht reuptake blockade potentiates human amygdala reactivity. Neuropsychopharmacology 33:3221–3225
Bradley AJ, Lenox-Smith AJ (2013) Does adding noradrenaline reuptake inhibition to selective serotonin reuptake inhibition improve efficacy in patients with depression? A systematic review of meta-analyses and large randomised pragmatic trials. J Psychopharmacol 27:740–758
Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA (2016) The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom 85:270–288
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JPT, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JPA, Geddes JR (2018) Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Focus (Am Psychiatr Publ) 16:420–429
Cipriani A, Furukawa TA, Salanti G, Geddes JR, Higgins JP, Churchill R, Watanabe N, Nakagawa A, Omori IM, McGuire H, Tansella M, Barbui C (2009) Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 373:746–758
Clevenger SS, Malhotra D, Dang J, Vanle B, IsHak WW (2018) The role of selective serotonin reuptake inhibitors in preventing relapse of major depressive disorder. Ther Adv Psychopharmacol 8:49–58
Courtet P, Lopez-Castroman J (2017) Antidepressants and suicide risk in depression. World Psychiatry 16:317–318
de Silva VA, Hanwella R (2012) Efficacy and tolerability of venlafaxine versus specific serotonin reuptake inhibitors in treatment of major depressive disorder: A meta-analysis of published studies. Int Clin Psychopharmacol 27:8–16
Dold M, Bartova L, Fugger G, Kautzky A, Mitschek MMM, Fabbri C, Montgomery S, Zohar J, Souery D, Mendlewicz J, Serretti A, Kasper S (2021) Melancholic features in major depression—a European multicenter study. Prog Neuropsychopharmacol Biol Psychiatry 110:110285
Dold M, Bartova L, Fugger G, Kautzky A, Souery D, Mendlewicz J, Papadimitriou GN, Dikeos DG, Porcelli S, Serretti A, Zohar J, Montgomery S, Kasper S (2018) Major depression and the degree of suicidality: results of the European group for the study of resistant depression (gsrd). Int J Neuropsychopharmacol 2:539–549
Dold M, Kasper S (2017) Evidence-based pharmacotherapy of treatment-resistant unipolar depression. Int J Psychiatry Clin Pract 21:13–23
Dold M, Kautzky A, Bartova L, Rabl U, Souery D, Mendlewicz J, Porcelli S, Serretti A, Zohar J, Montgomery S, Kasper S (2016) Pharmacological treatment strategies in unipolar depression in European tertiary psychiatric treatment centers—a pharmacoepidemiological cross-sectional multicenter study. Eur Neuropsychopharmacol 26:1960–1971
Dunlop BW, Granros M, Lechner A, Mletzko-Crowe T, Nemeroff CB, Mayberg HS, Craighead WE (2019) Recall accuracy for the symptoms of a major depressive episode among clinical trial participants. J Psychiatr Res 116:178–184
Dupuy JM, Ostacher MJ, Huffman J, Perlis RH, Nierenberg AA (2011) A critical review of pharmacotherapy for major depressive disorder. Int J Neuropsychopharmacol 14:1417–1431
Fountoulakis KN, Veroniki AA, Siamouli M, Moller HJ (2013) No role for initial severity on the efficacy of antidepressants: Results of a multi-meta-analysis. Ann Gen Psychiatry 12:26
Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J (2010) Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA 303:47–53
Frazer A, Blier P (2016) A neuroscience-based nomenclature (NbN) for psychotropic agents. Int J Neuropsychopharmacol 19(8):1–2
Gabriel FC, de Melo DO, Fraguas R, Leite-Santos NC, Mantovani da Silva RA, Ribeiro E (2020) Pharmacological treatment of depression: A systematic review comparing clinical practice guideline recommendations. PLoS ONE 15:e0231700
Gartlehner G, Gaynes BN, Hansen RA, Thieda P, DeVeaugh-Geiss A, Krebs EE, Moore CG, Morgan L, Lohr KN (2008) Comparative benefits and harms of second-generation antidepressants: background paper for the American college of physicians. Ann Intern Med 149:734–750
Gronemann FH, Petersen J, Alulis S, Jensen KJ, Riise J, Ankarfeldt MZ, Solem EJ, Bodker N, Osler M (2021) Treatment patterns in patients with treatment-resistant depression in Danish patients with major depressive disorder. J Affect Disord 287:204–213
Guidi J, Fava GA (2021) Sequential combination of pharmacotherapy and psychotherapy in major depressive disorder: a systematic review and meta-analysis. JAMA Psychiat 78:261–269
Hafferty JD, Wigmore EM, Howard DM, Adams MJ, Clarke TK, Campbell AI, MacIntyre DJ, Nicodemus KK, Lawrie SM, Porteous DJ, McIntosh AM (2019) Pharmaco-epidemiology of antidepressant exposure in a UK cohort record-linkage study. J Psychopharmacol 33:482–493
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Hawton K, Bergen H, Simkin S, Cooper J, Waters K, Gunnell D, Kapur N (2010) Toxicity of antidepressants: rates of suicide relative to prescribing and non-fatal overdose. Br J Psychiatry 196:354–358
Hayasaka Y, Purgato M, Magni LR, Ogawa Y, Takeshima N, Cipriani A, Barbui C, Leucht S, Furukawa TA (2015) Dose equivalents of antidepressants: evidence-based recommendations from randomized controlled trials. J Affect Disord 180:179–184
Hayes JF, Lewis G, Lewis G (2019) Newer-generation antidepressants and suicide risk. Psychother Psychosom 88:371–372
Hengartner MP, Ploderl M (2019) Newer-generation antidepressants and suicide risk in randomized controlled trials: a re-analysis of the FDA database. Psychother Psychosom 88:247–248
Hieronymus F, Lisinski A, Nilsson S, Eriksson E (2019) Influence of baseline severity on the effects of SSRIs in depression: An item-based, patient-level post-hoc analysis. Lancet Psychiatry 6:745–752
Hofmann SG, Curtiss J, Carpenter JK, Kind S (2017) Effect of treatments for depression on quality of life: a meta-analysis. Cogn Behav Ther 46:265–286
Huang KL, Lu WC, Wang YY, Hu GC, Lu CH, Lee WY, Hsu CC (2014) Comparison of agomelatine and selective serotonin reuptake inhibitors/serotonin-norepinephrine reuptake inhibitors in major depressive disorder: a meta-analysis of head-to-head randomized clinical trials. Aust N Z J Psychiatry 48:663–671
Imai H, Noma H, Furukawa TA (2021) Melancholic features (dsm-iv) predict but do not moderate response to antidepressants in major depression: an individual participant data meta-analysis of 1219 patients. Eur Arch Psychiatry Clin Neurosci 271:521–526
Jaffe DH, Rive B, Denee TR (2019) The burden of suicidal ideation across Europe: a cross-sectional survey in five countries. Neuropsychiatr Dis Treat 15:2257–2271
Kaminski JA, Bschor T (2020) Antidepressants and suicidality: a re-analysis of the re-analysis. J Affect Disord 266:95–99
Kasper S, Cubala WJ, Fagiolini A, Ramos-Quiroga JA, Souery D, Young AH (2020) Practical recommendations for the management of treatment-resistant depression with esketamine nasal spray therapy: basic science, evidence-based knowledge and expert guidance. World J Biol Psychiatry 1–15
Kasper S, Montgomery SA, Moller HJ, van Oers HJ, Jan Schutte A, Vrijland P, van der Meulen EA (2010) Longitudinal analysis of the suicidal behaviour risk in short-term placebo-controlled studies of mirtazapine in major depressive disorder. World J Biol Psychiatry 11:36–44
Kasper S, Sacher J, Klein N, Mossaheb N, Attarbaschi-Steiner T, Lanzenberger R, Spindelegger C, Asenbaum S, Holik A, Dudczak R (2009) Differences in the dynamics of serotonin reuptake transporter occupancy may explain superior clinical efficacy of escitalopram versus citalopram. Int Clin Psychopharmacol 24:119–125
Kaur U, Pathak BK, Singh A, Chakrabarti SS (2021) Esketamine: a glimmer of hope in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci 271:417–429
Kendrick T, Taylor D, Johnson CF (2019) Which first-line antidepressant? Br J Gen Pract 69:114–115
Kern DM, Cepeda MS, Defalco F, Etropolski M (2020) Treatment patterns and sequences of pharmacotherapy for patients diagnosed with depression in the United States: 2014 through 2019. BMC Psychiatry 20:4
Khan A, Fahl Mar K, Gokul S, Brown WA (2018) Decreased suicide rates in recent antidepressant clinical trials. Psychopharmacology 235:1455–1462
Kolovos S, van Tulder MW, Cuijpers P, Prigent A, Chevreul K, Riper H, Bosmans JE (2017) The effect of treatment as usual on major depressive disorder: a meta-analysis. J Affect Disord 210:72–81
Kraus C, Kadriu B, Lanzenberger R, Zarate CA Jr, Kasper S (2019) Prognosis and improved outcomes in major depression: a review. Transl Psychiatry 9:127
Kraus C, Rabl U, Vanicek T, Carlberg L, Popovic A, Spies M, Bartova L, Gryglewski G, Papageorgiou K, Lanzenberger R, Willeit M, Winkler D, Rybakowski JK, Kasper S (2017) Administration of ketamine for unipolar and bipolar depression. Int J Psychiatry Clin Pract 21:2–12
Kraus C, Wasserman D, Henter ID, Acevedo-Diaz E, Kadriu B, Zarate CA Jr (2019) The influence of ketamine on drug discovery in depression. Drug Discov Today 24:2033–2043
Lamers F, Vogelzangs N, Merikangas KR, de Jonge P, Beekman AT, Penninx BW (2013) Evidence for a differential role of hpa-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol Psychiatry 18:692–699
Lee Y, Rosenblat JD, Lee J, Carmona NE, Subramaniapillai M, Shekotikhina M, Mansur RB, Brietzke E, Lee JH, Ho RC, Yim SJ, McIntyre RS (2018) Efficacy of antidepressants on measures of workplace functioning in major depressive disorder: a systematic review. J Affect Disord 227:406–415
McAllister-Williams RH, Arango C, Blier P, Demyttenaere K, Falkai P, Gorwood P, Hopwood M, Javed A, Kasper S, Malhi GS, Soares JC, Vieta E, Young AH, Papadopoulos A, Rush AJ (2020) The identification, assessment and management of difficult-to-treat depression: an international consensus statement. J Affect Disord 267:264–282
McIntyre RS, Rosenblat JD, Nemeroff CB, Sanacora G, Murrough JW, Berk M, Brietzke E, Dodd S, Gorwood P, Ho R, Iosifescu DV, Lopez Jaramillo C, Kasper S, Kratiuk K, Lee JG, Lee Y, Lui LMW, Mansur RB, Papakostas GI, Subramaniapillai M, Thase M, Vieta E, Young AH, Zarate CA Jr, Stahl S (2021) Synthesizing the evidence for ketamine and esketamine in treatment-resistant depression: an international expert opinion on the available evidence and implementation. Am J Psychiatry 178:383–399
Mitschek MMM, Dremel M, Bartova L, Laggner A, Frey R (2021) The toxicity of antidepressants and antipsychotics in comparison with other medication, respectively alcohol (poster; topic: emergency psychiatry; young investigator award). In: 15th World Congress of Biological Psychiatry (virtual, 28–30062021)
Moller HJ, Baldwin DS, Goodwin G, Kasper S, Okasha A, Stein DJ, Tandon R, Versiani M, Pharmacopsychiatry WPASo, (2008) Do SSRIs or antidepressants in general increase suicidality? Wpa section on pharmacopsychiatry: consensus statement. Eur Arch Psychiatry Clin Neurosci 258(Suppl 3):3–23
Montgomery SA, Asberg M (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389
Montgomery SA, Baldwin DS, Blier P, Fineberg NA, Kasper S, Lader M, Lam RW, Lepine JP, Moller HJ, Nutt DJ, Rouillon F, Schatzberg AF, Thase ME (2007) Which antidepressants have demonstrated superior efficacy? A review of the evidence. Int Clin Psychopharmacol 22:323–329
Musil R, Seemüller F, Meyer S, Spellmann I, Adli M, Bauer M, Kronmüller KT, Brieger P, Laux G, Bender W, Heuser I, Fisher R, Gaebel W, Schennach R, Möller HJ, Riedel M (2018) Subtypes of depression and their overlap in a naturalistic inpatient sample of major depressive disorder. Int J Methods Psychiatr Res 27(1):e1569
Parker G, Fink M, Shorter E, Taylor MA, Akiskal H, Berrios G, Bolwig T, Brown WA, Carroll B, Healy D, Klein DF, Koukopoulos A, Michels R, Paris J, Rubin RT, Spitzer R, Swartz C (2010) Issues for dsm-5: Whither melancholia? The case for its classification as a distinct mood disorder. Am J Psychiatry 167:745–747
Pinna M, Manchia M, Oppo R, Scano F, Pillai G, Loche AP, Salis P, Minnai GP (2018) Clinical and biological predictors of response to electroconvulsive therapy (ECT): a review. Neurosci Lett 669:32–42
Prado CE, Watt S, Crowe SF (2018) A meta-analysis of the effects of antidepressants on cognitive functioning in depressed and non-depressed samples. Neuropsychol Rev 28:32–72
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, Ritz L, Biggs MM, Warden D, Luther JF, Shores-Wilson K, Niederehe G, Fava M, Team SDS (2006) Bupropion-sr, sertraline, or venlafaxine-xr after failure of SSRIs for depression. N Engl J Med 354:1231–1242
Sanders Benjamin AQB (2021) Intranasal esketamine: From origins to future implications in treatment-resistant depression. J Psychiatr Res 137:29–35
Schosser A, Serretti A, Souery D, Mendlewicz J, Zohar J, Montgomery S, Kasper S (2012) European group for the study of resistant depression (gsrd)–where have we gone so far: Review of clinical and genetic findings. Eur Neuropsychopharmacol 22:453–468
Seemuller F, Riedel M, Obermeier M, Bauer M, Adli M, Mundt C, Holsboer F, Brieger P, Laux G, Bender W, Heuser I, Zeiler J, Gaebel W, Jager M, Henkel V, Moller HJ (2009) The controversial link between antidepressants and suicidality risks in adults: data from a naturalistic study on a large sample of in-patients with a major depressive episode. Int J Neuropsychopharmacol 12:181–189
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The mini-international neuropsychiatric interview (m.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for dsm-iv and icd-10. J Clin Psychiatry 59(Suppl 20):22–33
Souery D, Oswald P, Massat I, Bailer U, Bollen J, Demyttenaere K, Kasper S, Lecrubier Y, Montgomery S, Serretti A, Zohar J, Mendlewicz J, Group for the Study of Resistant D (2007) Clinical factors associated with treatment resistance in major depressive disorder: results from a European multicenter study. J Clin Psychiatry 68:1062–1070
Undurraga J, Vazquez GH, Tondo L, Baldessarini RJ (2020) Antidepressant responses in direct comparisons of melancholic and non-melancholic depression. J Psychopharmacol 34:1335–1341
Valerio MP, Szmulewicz AG, Martino DJ (2018) A quantitative review on outcome-to-antidepressants in melancholic unipolar depression. Psychiatry Res 265:100–110
Wang SM, Kim NY, Na HR, Lim HK, Woo YS, Pae CU, Bahk WM (2021) Rapid onset of intranasal esketamine in patients with treatment resistant depression and major depression with suicide ideation: a meta-analysis. Clin Psychopharmacol Neurosci 19:341–354
Wittchen H, Wunderlich U, Gruschwitz S, Zaudig M (1997) Skid-i, strukturiertes klinisches interview für dsm-iv. Hogrefe Göttingen, Germany
Zohar J, Stahl S, Moller HJ, Blier P, Kupfer D, Yamawaki S, Uchida H, Spedding M, Goodwin GM, Nutt D (2015) A review of the current nomenclature for psychotropic agents and an introduction to the neuroscience-based nomenclature. Eur Neuropsychopharmacol 25:2318–2325
Acknowledgements
The authors would like to thank all persons involved in the GSRD project and the patients who participated in the present study.
Funding
Open access funding provided by Medical University of Vienna. The European Group for the Study of Resistant Depression (GSRD) obtained an unrestricted grant sponsored by Lundbeck A/S. The sponsor played no role in designing the study, data collection and analyses, interpretation of the data, writing of the manuscript, and in the decision to submit the research for publication.
Author information
Authors and Affiliations
Contributions
Dr. LB and Dr. GF contributed equally to designing the study, implementation of the research, statistical analyses, and writing the report including the first draft of the manuscript. Dr. SK contributed to designing the study, implementation of the research, and writing the report. All authors substantially contributed to implementation of the research and have critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The present research complies with internationally accepted standards for research practice and reporting, and has been performed with approvals of appropriate ethics committees and with appropriate participants’ informed consent in compliance with the Helsinki Declaration.
Conflict of interest
Dr. Bartova has received travel grants and consultant/speaker honoraria from AOP Orphan, Medizin Medien Austria, Vertretungsnetz, Schwabe Austria, Janssen and Angelini. Dr. Fugger has received consultant/speaker honoraria from Janssen. Dr. Dold has received travel grants and consultant/speaker honoraria from Janssen-Cilag. Dr. Zohar has received grant/research support from Lundbeck, Servier, and Pfizer; he has served as a consultant or on the advisory boards for Servier, Pfizer, Solvay, and Actelion; and he has served on speakers’ bureaus for Lundbeck, GlaxoSmithKline, Jazz, and Solvay. Dr. Mendlewicz is a member of the board of the Lundbeck International Neuroscience Foundation and of the advisory board of Servier. Dr. Souery has received grant/research support from GlaxoSmithKline and Lundbeck; and he has served as a consultant or on advisory boards for AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Janssen, and Lundbeck. Dr. Montgomery has served as a consultant or on advisory boards for AstraZeneca, Bionevia, Bristol-Myers Squibb, Forest, GlaxoSmithKline, Grunenthal, Intellect Pharma, Johnson & Johnson, Lilly, Lundbeck, Merck, Merz, M's Science, Neurim, Otsuka, Pierre Fabre, Pfizer, Pharmaneuroboost, Richter, Roche, Sanofi, Sepracor, Servier, Shire, Synosis, Takeda, Theracos, Targacept, Transcept, UBC, Xytis, and Wyeth. Dr. Fabbri has been supported by Fondazione Umberto Veronesi (https://www.fondazioneveronesi.it). Dr. Serretti has served as a consultant or speaker for Abbott, Abbvie, Angelini, AstraZeneca, Clinical Data, Boehringer, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Innovapharma, Italfarmaco, Janssen, Lundbeck, Naurex, Pfizer, Polifarma, Sanofi, and Servier. Within the last three years, Dr. Kasper received grants/research support, consulting fees, and/or honoraria from Angelini, Celegne GmbH, Eli Lilly, Janssen-Cilag Pharma GmbH, KRKA-Pharma, Lundbeck A/S, Mundipharma, Neuraxpharm, Pfizer, Sanofi, Schwabe, Servier, Shire, Sumitomo Dainippon Pharma Co. Ltd., sun Pharma and Takeda. All other authors declare that they have no conflicts of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fugger, G., Bartova, L., Fabbri, C. et al. The sociodemographic and clinical profile of patients with major depressive disorder receiving SSRIs as first-line antidepressant treatment in European countries. Eur Arch Psychiatry Clin Neurosci 272, 715–727 (2022). https://doi.org/10.1007/s00406-021-01368-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-021-01368-3