Abstract
Purpose
To examine whether and how interleukin (IL)-1α is involved in chronic rhinosinusitis with nasal polyps (CRSwNP).
Methods
Nasal polyp (NP) and control tissues were collected from CRSwNP patients and control subjects. The expression of IL-1α and other proinflammatory cytokines (IL-1β, IL-8 and IL-13, etc.), as well as neutrophil and eosinophil accumulation, were examined in sinonasal tissues using immunohistochemical (IHC), immunofluorescent (IF) staining, qPCR, and Luminex, respectively. Moreover, the regulation of IL-1α expression and its effects on other proinflammatory cytokines were evaluated in cultured nasal epithelial cells (NECs).
Results
The mRNA and protein levels of IL-1α were significantly higher in NP tissues compared to that in control tissues. IL-1α in polyp tissues was mainly located in epithelial cells and neutrophils. Polyps IL-1α level was significantly associated with IL-8, IL-1β, IL-6, IL-4 and IL-13 production, as well as tissue neutrophil infiltration. Moreover, poly (I:C), lipopolysaccharides, Flagellin, R848 and cytokines (IL-4, IL-5, and IL-13) significantly increased the expression of IL-1α in cultured NECs in vitro, and recombinant IL-1α significantly promoted production of IL-8 and CXCL1 in cultured NECs.
Conclusions
These findings provided the evidence that IL-1α were significantly increased in NP tissues, which may contribute to tissue neutrophilia in CRSwNP patients in China.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a heterogeneous chronic inflammatory disorder characterized by visible formation of nasal polyp (NP) with massive tissue edema and distinct inflammatory endotype [1]. In western countries, the majority of CRSwNP patients have previously been reported to be a Th2-typed inflammatory profile with significant tissue eosinophilia, whereas neutrophilic inflammation and mixed Th1/Th17 inflammatory profiles are observed prominently in Asian CRSwNP patients [2]. However, recent evidences show activated neutrophils are significantly elevated in both Asian and Caucasian CRSwNP patients [3,4,5]. In China, we previously demonstrated that adult CRSwNP patients with enhanced tissue neutrophilia show poor respond to oral corticosteroids [3], and Liao et al. found increased IL-8 expression and more patients with difficult-to-treat CRSwNP in clusters with severe or moderate neutrophilic inflammation by performing a cluster analysis based on clinical variables and pathological features [6]. More recently, Kim et al. reported subepithelial neutrophil infiltration predicts a poor surgical outcome in Korean CRSwNP patients [7]. However, the key factors underlying tissue neutrophilia in these CRSwNP patients are not yet completely understood.
Interleukin (IL)-1 is a family of robust pro-inflammatory cytokines with an exceedingly narrow margin between effectivity and toxicity which needs to be strictly regulated in humans [8]. There are two major members of IL-1, IL-1α and IL-1β. IL‐1α could be produced by epithelial, mesenchymal, and hematopoietic cells, while IL‐1β is primarily produced by monocytes, macrophages, and neutrophils [9]. We previously showed IL-1β was upregulated in neutrophilic CRSwNP following NLRP3 inflammasome activation, which may contributes to NP neutrophilic inflammation [10], and an association between IL1A polymorphism and chronic rhinosinusitis has been demonstrated by other groups as well [11], but the possible role of IL-1α in the pathogenesis of CRSwNP remains unclear. This study thus aimed to investigate the expression of IL-1α and its association with tissue neutrophilia in Chinese CRSwNP patients.
Materials and methods
Subjects
This study was approved by the ethical committee of Eye and ENT Hospital, Fudan University, and written informed consent was obtained from all the subjects. All 45 CRSwNP patients were recruited from the Department of Otolaryngology, Eye and ENT hospital, Fudan University. The diagnosis of CRSwNP was made according to the international EPOS consensus [1]. As normal controls, 29 non-atopic patients undergoing septoplasty for nasal septum deviation, endoscopic optic nerve decompression because of traumatic optic neuropathy, or transnasal skull surgery because of anterior skull base tumors were enrolled. The atopic status of the patients and normal controls were evaluated by allergen skin prick tests or serum specific IgE assay. The diagnosis of asthma was made based on case history and pulmonary function test or a prior physician diagnosis. Subjects with acute infection, immunodeficiency, antrochoanal polyps, or allergic fungal sinusitis were excluded from the study.
The demographic characteristics of the subjects are listed in Table 1. NP tissues from CRSwNP patients and sinonasal tissues from normal controls were obtained during surgery. Tissue samples were separated into several portions for RNA and protein extraction, immunohistochemical (IHC) or immunofluorescence (IF) staining. Due to the limit of tissues, not all samples were included in every study protocol.
IHC and IF staining
4-μm sections were cut from paraffin-embedded tissues. For IHC staining, the sections were incubated with primary antibodies against IL-1α (1:100, Abcam, Cambridge, MA, USA), IL-1R1(1:800, Abcam), and neutrophil elastase (NE, 1:1000, Abcam) overnight at 4 °C. Thereafter, each section was incubated and visualized using the Dako REAL EnVision Detection System (Agilent Technologies, Santa Clara, CA, USA). The sections were examined via light microscopy by two investigators who were unaware of the clinical data. The number of NE positive cells was counted in 5 high-power fields (HPFs, 400 ×) with prominent inflammation and averaged. The IHC score of IL-1α was analyzed using the IHC Profiler plugin in ImageJ software. For IF staining, sections were incubated with primary antibodies against IL-1α (1:200, Abcam) and neutrophil elastase (NE, 1:400, Abcam) overnight at 4 °C in two rounds of staining, each using a separate fluorescent tyramide signal amplification system. Images were obtained using a fluorescence microscope (Nikon, Tokyo, Japan).
Quantitative real-time polymerase chain reaction (RT-qPCR) analysis
The mRNA expression in sinonasal tissues were evaluated using qPCR analysis. Total RNA from sinonasal tissues was extracted using TRIzol (Invitrogen, Carlsbad, CA, USA) and total RNA of cells was extracted using RNAsimple Total RNA Kit (Tiangen, Beijing, China) in accordance with the manufacturer’s instructions. Reverse transcription was performed to synthesized from 1 μg of total RNA using PrimeScript™ RT Master Mix (TaKaRa, Shiga, Japan). mRNA expression was determined using the ABI PRISM 7500 Detection System (Applied Biosystems, Foster City, CA) with SYBR Green Pro Taq HS qPCR Kit (Accurate Biology, Hunan, China). Primers were chosen based on the published data. Target gene expression was normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH) and analyzed using the 2−ΔΔCt method. The primer sequences are listed in Table 2.
Luminex and enzyme linked immunosorbent assay (ELISA)
Tissues were homogenized and lysed in RIPA buffer supplemented with protease inhibitors purchased from Beyotime Biotechnology. BCA kits were used to detect total protein concentration. The levels of IL-1α, IL-8, and C–X–C motif chemokine 1 (CXCL1) in tissues or cell-free culture supernatants were determined using Luminex kits (R&D Systems, Minneapolis, MN, USA) and ELISA kits (Neobioscience, Shenzhen, China) according to the manufacturer’s protocol, respectively.
Cell culture and stimulation
Human nasal epithelial cells (HNEpCs) were purchased from PromoCell and grown in minimal essential medium supplemented with 10% fetal bovine serum and Antibiotic–Antimycotic (1:100, Gibco, Grand Island, NY, USA). When a confluence of 80–90% was reached, the cells were washed with PBS, and were treated with Pan3CSK4 (5 μg/mL, Invivogen), poly (I:C) (20 μg/mL, Sigma-Aldrich, St. Louis, MO), Lipopolysaccharides (LPS, 10 μg/mL, Invivogen), Flagellin (200 ng/mL, Invivogen), R848 (5 μg/mL, MedChemExpress, Monmouth Junction, NJ, USA), IFN-γ (50 ng/mL, PeproTech, Cranbury, NJ, USA), IL-4 (50 ng/mL, PeproTech), IL-5(50 ng/mL, PeproTech), IL-6 (50 ng/mL, PeproTech), IL-8 (100 ng/mL, PeproTech), IL-13 (50 ng/mL, PeproTech), indeno(1,2,3-cd)pyrene (IP, 10 nM, Sigma-Aldrich), and multiple concentrations of IL-1α (PeproTech) as noted, respectively. In some experiments, cells were pre-incubated with dexamethasone (DEX, Sigma-Aldrich) for 2 h.
Statistical analysis
Data were presented as medians and interquartile ranges, or as mean and standard error of the mean. Data were carried out using Prism GraphPad (Prism 8, GraphPad Software, San Diego, CA, USA). The data were analyzed using the Mann–Whitney U test or Student’s t test. The Pearson’s or Spearman’s correlation coefficient test were used to assess the associations between data sets. A P value of less than 0.05 was considered as statistically significant.
Results
Expression of IL-1α in NP tissues of CRSwNP patients and sinonasal tissues of normal controls
As shown in Fig. 1, IL-1α and its receptor IL-1R1 were mainly localized in nasal epithelium and the stromal cells, as determined by IHC staining. The IHC score of IL-1α in NP tissues was significantly higher than that in control tissues (P < 0.01). Be consistent with the IHC results, the mRNA level of IL-1α but not IL-1R1 in NP tissues was significantly increased compared to control tissues (P < 0.05). As to the protein level, we found protein level of IL-1α was also significantly increased in NP tissues compared to control tissues (P < 0.05). We further examined the cellular sources of IL-1α in NP tissues by IF staining. As shown in Fig. 2, we found both nasal epithelial cells and neutrophils were able to produce IL-1α in NP tissues.
Increased expression of IL-1α in nasal polyp tissues (NP) in CRSwNP patients. A, B Representative immunohistochemistry (IHC) staining for IL-1α and IL-1R1 in control and polyp tissues. Scale bar, 50 μm. C IHC scores of IL-1α staining in control tissues (n = 10) and polyp tissues (n = 17). D, E mRNA levels of IL-1α and IL-1R1 in control tissues (n = 24 and 21, respectively) and polyp tissues (n = 39). F Protein level of IL-1α in control tissues (n = 22) and polyp tissues (n = 33). *P < 0.05, ***P < 0.001
Immunofluorescence staining of IL-1α in epithelial cells and neutrophils of polyp tissues in CRSwNP patients. Representative immunofluorescence staining of IL-1α (red) and neutrophil elastase (NE, green) in polyp tissue. Dotted lines indicate the epithelial cell layer boundary. Scale bars for top images, 50 μm. Scale bars for bottom images, 20 μm
Association of IL-1α protein level with inflammatory cells and cytokines in sinonasal tissues
We then evaluated the association of IL-1α protein level with the infiltrated neutrophils and eosinophils in sinonasal tissues. As shown in Fig. 3, we found IL-1α protein level was significantly associated with neutrophil number, but not eosinophil number, in sinonasal tissues(P < 0.05). Moreover, we found the protein level of IL-1α was significantly associated with IL-8, IL-1β, IL-6, IL-4, IL-13 but not CCL11 in NP tissues of CRSwNP patients (P < 0.05) (Fig. 4).
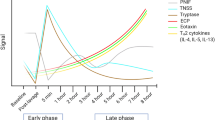
Regulation of IL-1α expression in cultured epithelial cells after stimulation
We next examined the mRNA expression of IL-1α in cultured human nasal epithelial cells (HNEpCs) after stimulation. As shown in Fig. 5, cultured HNEpCs were stimulated with TLR agonists (Pan3CSK4, poly (I:C), LPS, Flagellin, R848), cytokines (IFN-γ, IL-4, IL-5, IL-6, IL-8, IL-13) or a major environmental pollutant (IP) for 3 h and harvested. As to the TLR agonists, poly (I:C), LPS, Flagellin and R848 were able to significantly increased the mRNA expression of IL-1α in cultured HNEpCs (P < 0.05). As to the cytokines, we found IL-4, IL-5 and IL-13 were able to significantly increased the mRNA expression of IL-1α in cultured HNEpCs (P < 0.05). Moreover, a major environmental pollutant (IP) was shown to significantly increased the mRNA expression of IL-1α in cultured HNEpCs (P < 0.05).
Expression of IL-1α in cultured nasal epithelial cells in response to different stimuli. The mRNA expression of IL-1α in cultured human nasal epithelial cells (HNEpCs) after stimulation. HNEpCs were cultured alone or with TLR agonists (Pan3CSK4, poly (I:C), LPS, Flagellin, R848), cytokines (IFN-γ, IL-4, IL-5, IL-6, IL-8, IL-13) or a major environmental pollutant (IP) for 3 h (n = 3). *P < 0.05, **P < 0.01
Expression of IL-8 and CXCL1 in cultured epithelial cells after stimulation with recombinant IL-1α
We finally examined the expression of IL-8 and CXCL1 in cultured nasal epithelial cells after stimulation with recombinant IL-1α. As shown in Fig. 6, we found the mRNA levels of IL-8 and CXCL1 were significantly increased in cultured HNEpCs after stimulated with IL-1α in a time (peak point at 3 h) and dose-dependent manner. Consistently, the protein levels of IL-8 and CXCL1 were significantly increased in cell-free culture supernatants of HNEpCs after stimulated with IL-1α. When corticosteroid was added priorly, we found IL-1α-induced mRNA levels of IL-8 and CXCL1 in cultured HNEpCs were significantly suppressed by DEX (P < 0.01).
IL-1α induced the production of IL-8 and CXCL1 in cultured nasal epithelial cells. A mRNA levels of IL-8 and CXCL1 were significantly increased in cultured human nasal epithelial cells (HNEpCs) after stimulated with different concentrations of IL-1α for 3 h (n = 3). B mRNA levels of IL-8 and CXCL1 were significantly increased in cultured HNEpCs after stimulated with IL-1α (10 ng/mL) for 3, 6 and 9 h, respectively (n = 3). C Protein levels of IL-8 and CXCL1 were significantly increased in cell-free culture supernatants of HNEpCs after stimulated with IL-1α (10 ng/mL) for 48 h (n = 3). D Corticosteroid suppressed the mRNA levels of IL-8 and CXCL1 in cultured HNEpCs in response to IL-1α stimulation. HNEpCs were pre-incubated with DEX (80 ng/mL) for 2 h and then stimulated with IL-1α (10 ng/mL) for 3 h (n = 3). **P < 0.01, ***P < 0.001
Discussion
In this study, we provided the evidence that the mRNA and protein levels of IL-1α were significantly increased in NP tissues of CRSwNP patients, which was positively associated with tissue neutrophil accumulation. These findings might improve our understanding on how IL-1α is involved in the pathogenesis of neutrophilic mucous inflammation in Eastern CRSwNP patients.
CRSwNP is well-known to be characterized by type 2 inflammation and tissue eosinophilia [1], whereas the pathogenesis of neutrophilic CRSwNP has not been fully understood. IL-1α is an important trigger for leukocyte recruitment and inflammation in other airway diseases [8], and epithelial cell-derived IL-1α could activate the expression of intercellular adhesion molecule 1 on endothelial cells in adenovirus type 37-induced airway inflammation [12]. These findings collectively indicate epithelial cell-derived IL-1α is an important trigger for leukocyte recruitment and the exacerbation of inflammation. However, whether IL-1α is involved in the pathogenesis of CRSwNP remains unclear. In this study, we first demonstrated the increased expression of IL-1α in NP tissues was significantly associated with tissue neutrophil accumulation. Interestingly, we found both epithelial cells and neutrophils were the cellular source of IL-1α in NP tissue, indicating a possible self-amplified loop in the neutrophilic inflammation in CRSwNP patients.
We further evaluated the association of IL-1α and other cytokines in NP tissues. As a consequence, we found the protein level of IL-1α was significantly associated with IL-8, IL-1β, IL-6, IL-4, IL-13, but not CCL11 in NP tissues of CRSwNP patients. Previously, we demonstrated that enhanced HIF-1α expression in NP tissues may cause tissue neutrophilia and poor steroid response, and provided an alternative to restore steroid sensitivity by adding clarithromycin [13], and Wang et al. showed that the IL-36γ/IL-36R pathway play a critical role in the development of neutrophilic inflammation and corticosteroid resistance in CRSwNP patients [14]. Collectively, these findings indicate NP neutrophils may be considered a heretofore unrecognized therapeutic target in the management of CRSwNP [15]. Considering both epithelial cells and neutrophils were the cellular source of IL-1α in NP tissue, our findings indicated polyp IL-1α in self-amplified loop may play a central role in the regulation of neutrophilic inflammation of NP tissues.
It has been reported that bronchial epithelial cells are able to release IL-1α to trigger the production of granulocyte macrophage colony-stimulating factor and IL-33 to recruit dendritic cells following TLR4 activation [16]. To further characterize the regulation of IL-1α in polyp epithelial cells in CRSwNP patients, we next examined the expression in cultured NECs in vitro. Consequently, we found IL-1α expression in NECs can be significantly stimulated by both TLR agonists and pro-inflammatory cytokines and environmental pollutant. As to the TLR agonists, poly (I:C), LPS, Flagellin and R848 were able to significantly increased the mRNA expression of IL-1α in cultured HNEpCs, indicating virus, bacteria and other external stimuli were able to stimulate IL-1α production through TLR-mediated pathway. As to the cytokines, we interestingly found Th2 cytokines (IL-4, IL-5 and IL-13) were able to significantly increased the mRNA expression of IL-1α in cultured HNEpCs. These findings may provide a clue that how Th2-dominant eosinophilic inflammation in NP tissues promoted tissue neutrophilia by inducing IL-1α production, to a lesser extent.
In cystic fibrosis, rhinovirus- and hypoxia-induced epithelial necrosis causes IL-1α release and subsequent IL‐8 expression, which may promote neutrophilic inflammation [17, 18]. Since IL-8 and CXCL1 have been known to be the potent chemokines of circulated neutrophil, the underlying mechanism of IL-1α in driving NP tissue neutrophilia, we, therefore, evaluated them in cultured NECs in response to recombinant IL-1α in vitro. As estimated, we found the expression of IL-8 and CXCL1 were significantly increased in cultured HNEpCs after stimulated with IL-1α which can be inhibited by adding corticosteroid. Up to now, only limited studies reported the importance of IL-1α and associated neutrophil in the pathogenesis of CRSwNP. For example, Liu et al. reported increased IL-1α in CRSwNP patients, but they showed activated monocytes as a major source of IL-1α in the NP tissues [19]. In this study, our findings further show both epithelial cells and neutrophils were the cellular source of IL-1α, and established the positive association of IL-1α and neutrophils in NP tissues. Moreover, our results showed both TLR agonists and Th2 cytokines were able to stimulate IL-1α production in cultured epithelial cells, indicating a possible role of epithelial cell derived-IL-1α in linking external stimuli with subsequent IL-8 and CXCL1-mediated neutrophil chemotaxis by a self-amplified loop. These findings thus added a new insight into the possible molecular mechanisms underlying enhanced tissue neutrophilia in response to increased IL-1α in CRSwNP patients, which could be considered as the therapeutic target in the future.
Conclusions
In the present study, we found increased IL-1α were significantly associated with tissue neutrophil accumulation in CRSwNP patients. Our findings showed both epithelial cells and neutrophils were the cellular source of IL-1α, indicating a self-amplified loop of IL-1α in driving tissue neutrophilia in NP tissues. Moreover, we found both TLR agonists and Th2 cytokines were able to stimulate IL-1α production in cultured epithelial cells, indicating a possible role of IL-1α in linking external stimuli with subsequent IL-8 and CXCL1-mediated neutrophil chemotaxis.
References
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, Cohen N, Cervin A, Douglas R, Gevaert P, Georgalas C, Goossens H, Harvey R, Hellings P, Hopkins C, Jones N, Joos G, Kalogjera L, Kern B, Kowalski M, Price D, Riechelmann H, Schlosser R, Senior B, Thomas M, Toskala E, Voegels R, de Wang Y, Wormald PJ (2012) EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50:1–12
Liu Z, Chen J, Cheng L, Li H, Liu S, Lou H, Shi J, Sun Y, Wang D, Wang C, Wang X, Wei Y, Wen W, Yang P, Yang Q, Zhang G, Zhang Y, Zhao C, Zhu D, Zhu L, Chen F, Dong Y, Fu Q, Li J, Li Y, Liu C, Liu F, Lu M, Meng Y, Sha J, She W, Shi L, Wang K, Xue J, Yang L, Yin M, Zhang L, Zheng M, Zhou B, Zhang L (2020) Chinese Society of Allergy and Chinese Society of Otorhinolaryngology-Head and Neck Surgery guideline for chronic rhinosinusitis. Allergy Asthma Immunol Res 12:176–237
Wen W, Liu W, Zhang L, Bai J, Fan Y, Xia W, Luo Q, Zheng J, Wang H, Li Z, Xia J, Jiang H, Liu Z, Shi J, Li H, Xu G (2012) Increased neutrophilia in nasal polyps reduces the response to oral corticosteroid therapy. J Allergy Clin Immunol 129:1522–1528
Ruan JW, Zhao JF, Li XL, Liao B, Pan L, Zhu KZ, Feng QM, Liu JX, Yu ZE, Song J, Wang H, Liu Z (2021) Characterizing the neutrophilic inflammation in chronic rhinosinusitis with nasal polyps. Front Cell Dev Biol 9:793073
Delemarre T, Holtappels G, De Ruyck N, Zhang N, Nauwynck H, Bachert C, Gevaert E (2021) A substantial neutrophilic inflammation as regular part of severe type 2 chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol 147:179-188.e2
Liao B, Liu JX, Guo CL, Li ZY, Pan L, Liu Z (2020) A panel of clinical and biological markers predict difficult-to-treat chronic rhinosinusitis. Allergy 75(4):946–949
Kim DK, Lim HS, Eun KM, Seo Y, Kim JK, Kim YS, Kim MK, Jin S, Han SC, Kim DW (2021) Subepithelial neutrophil infiltration as a predictor of the surgical outcome of chronic rhinosinusitis with nasal polyps. Rhinology 59:173–180
Dinarello CA (1996) Biologic basis for interleukin-1 in disease. Blood 87:2095–2147
Balazs A, Mall MA (2019) Mucus obstruction and inflammation in early cystic fibrosis lung disease: Emerging role of the IL-1 signaling pathway. Pediatr Pulmonol 54(Suppl 3):S5–S12
Wei Y, Zhang J, Wu X, Sun W, Wei F, Liu W, Lu T, Ji W, Li H, Wen W (2020) Activated pyrin domain containing 3 (NLRP3) inflammasome in neutrophilic chronic rhinosinusitis with nasal polyps (CRSwNP). J Allergy Clin Immunol 145(1002–5):e16
MfunaEndam L, Cormier C, Bossé Y, Filali-Mouhim A, Desrosiers M (2010) Association of IL1A, IL1B, and TNF gene polymorphisms with chronic rhinosinusitis with and without nasal polyposis: a replication study. Arch Otolaryngol Head Neck Surg 136:187–192
Chang CH, Huang Y, Issekutz AC, Griffith M, Lin KH, Anderson R (2002) Interleukin-1alpha released from epithelial cells after adenovirus type 37 infection activates intercellular adhesion molecule 1 expression on human vascular endothelial cells. J Virol 76:427–431
Yu Z, Wang Y, Hu X, Xu H, Han M, Zhang J, Wen W, Shu H, Li H (2020) Overexpression of hypoxia-inducible factor 1alpha is associated with neutrophilic inflammation in chronic rhinosinusitis with nasal polyps. Auris Nasus Larynx 47:401–409
Wang H, Li ZY, Jiang WX, Liao B, Zhai GT, Wang N, Zhen Z, Ruan JW, Long XB, Wang H, Liu WH, Liang GT, Xu WM, Kato A, Liu Z (2018) The activation and function of IL-36γ in neutrophilic inflammation in chronic rhinosinusitis. J Allergy Clin Immunol 141:1646–1658
Zhang L, Lan F (2020) Understanding the role of neutrophils in refractoriness of chronic rhinosinusitis with nasal polyps. Allergy Asthma Immunol Res 12:1–3
Willart MA, Deswarte K, Pouliot P, Braun H, Beyaert R, Lambrecht BN, Hammad H (2012) Interleukin-1alpha controls allergic sensitization to inhaled house dust mite via the epithelial release of GM-CSF and IL-33. J Exp Med 209:1505–1517
Montgomery ST, Frey DL, Mall MA, Stick SM, Kicic A, Arest CF (2020) Rhinovirus infection is associated with airway epithelial cell necrosis and inflammation via interleukin-1 in young children with cystic fibrosis. Front Immunol 11:596
Fritzsching B, Zhou-Suckow Z, Trojanek JB, Schubert SC, Schatterny J, Hirtz S, Agrawal R, Muley T, Kahn N, Sticht C, Gunkel N, Welte T, Randell SH, Langer F, Schnabel P, Herth FJ, Mall MA (2015) Hypoxic epithelial necrosis triggers neutrophilic inflammation via IL-1 receptor signaling in cystic fibrosis lung disease. Am J Respir Crit Care Med 191:902–913
Liu Y, Hamaguchi Y, Taya M, Sakakura Y (1993) Quantification of interleukin-1 in nasal polyps from patients with chronic sinusitis. Eur Arch Otorhinolaryngol 250:123–125
Acknowledgements
This study was supported by the National Natural Science Grants of China (no. 81725004, 82101191, 82271138) and Shanghai Science and Technology Committee Grants (19XD4010000, 20MC1920200).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
No conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cao, Y., Hu, X., Zhou, C. et al. Increased IL-1α expression in chronic rhinosinusitis with nasal polyps. Eur Arch Otorhinolaryngol 280, 1209–1217 (2023). https://doi.org/10.1007/s00405-022-07640-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07640-z