Abstract
Purpose
Many studies have been conducted about the effect of cigarettes and other tobacco products on mucociliary clearance. However, there has been no study of the relationship between mucociliary clearance and Maras powder, which is a smokeless tobacco product. The aim of this study was to evaluate the effect of Maras powder use on mucociliary clearance through comparisons with cigarette smokers and those who used no tobacco products.
Methods
The study included 75 male volunteers, aged 23–54 years. Group 1 (n: 25) comprised subjects who do not use any tobacco products, Group 2 (n: 25) those who smoked cigarettes, and Group 3 (n: 25) those who used Maraş powder. The saccharin test was used to evaluate mucociliary clearance and the time was recorded in seconds. The groups were statistically compared in respect of mean age and mucociliary clearance time (MCCT).
Results
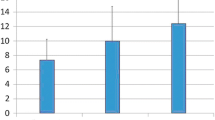
The mean MCCT was determined to be 645.8 ± 200 secs for the whole study sample, 497 ± 108 secs for Group 1, 796 ± 200 secs for Group 2, and 644 ± 161 secs for Group 3. The difference between the groups in respect of MCCT was statistically significant (p < 0.001). No statistically significant difference was determined between the groups in respect of mean age (p = 0.730).
Conclusion
The study results demonstrated that the nasal mucociliary clearance time was prolonged both by cigarettes and by the use of Maras powder, and that this time was prolonged more by cigarette smoking than the use of Maras powder.

Similar content being viewed by others
References
Taş B, Güre AO (2020) The effect of Maras powder and smoking on the microRNA deregulation of oral mucosa. J Appl Oral Sci. https://doi.org/10.1590/1678-7757-2019-0382
Organization WH (2011) Burden: mortality, morbidity and risk factors. Global status report on noncommunicable diseases 2010
Prasetyo A, Sadhana U, Budiman J (2021) Nasal mucociliary clearance in smokers: a systematic review. Int Arch Otorhinolaryngol 25:160–169. https://doi.org/10.1055/s-0040-1702965
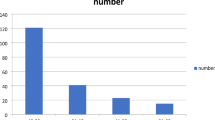
Glover ED, Glover PN (1992) The smokeless tobacco problem: risk groups in North America. Pounds (millions) 3
Dagli AF, Sahin N, Bozdag Z, Ucer O, Akatli AN, Artas G, Sahin İ, Yardim M, Dalkilic S, Akkoc RF (2017) Cytological and cytomorphometric characteristics of buccal mucosa cells from smokeless tobacco users. Diagn Cytopathol 45:976–982. https://doi.org/10.1002/dc.23803
Akbay C, Kafas A (2017) Kahramanmaraş il merkezinde tüketicilerin sigara ve maraş otu kullanımını etkileyen faktörlerin analizi. KSU J Nat Sci. 20:276–282. https://doi.org/10.18016/ksudobil.289471
Sagiroglu S, Erdogan A, Doganer A, Okyay RA (2019) Otorhinolaryngological symptoms among smokeless tobacco (Maras powder) users. North Clin Istanb 6:284. https://doi.org/10.14744/nci.2018.50024
Sucakli MH, Ozkan F, Inci MF, Celik M, Keten HS, Bozoglan O (2013) Effects of smokeless tobacco (Maras powder) use on carotid intima media thickness. Med Sci Monit 19:859. https://doi.org/10.12659/MSM.889654
Çömez A, Karaküçük Y, Beyoğlu A (2020) Evaluation of the effect of smokeless tobacco (Maras powder) on choroidal and retinal blood flow: an optical coherence tomography angiography study. Int Ophthalmol 40:1367–1376. https://doi.org/10.1007/s10792-020-01302-x
Yılmaz İnanç FÖO, İnanç Y (2018) The effects of Maras powder use on patients with migraine. Neuropsychiatr Dis Treat 14:1143. https://doi.org/10.2147/NDT.S164818
Buyukbese MA, Koksal N, Guven A, Cetinkaya A (2004) Effects of smokeless tobacco “Maras powder” use on respiratory functions. Tohoku J Exp Med 204:173–178. https://doi.org/10.1620/tjem.204.173
Paul B, Menon S, Vasthare R, Balakrishnan R, Acharya S (2018) Effect of bidi smoking on nasal mucociliary clearance: a comparative study. J Laryngolotol 132:1077–1082. https://doi.org/10.1017/S0022215118002049
Sinha DN, Gupta PC, Kumar A, Bhartiya D, Agarwal N, Sharma S, Singh H, Parascandola M, Mehrotra R (2018) The poorest of poor suffer the greatest burden from smokeless tobacco use: a study from 140 countries. Nicotine Tob Res 20:1529–1532. https://doi.org/10.1093/ntr/ntx276
Hatsukami D, Zeller M, Gupta P, Parascandola M, Asma S (2014) Smokeless tobacco and public health: a global perspective
Warnakulasuriya S, Straif K (2018) Carcinogenicity of smokeless tobacco: evidence from studies in humans and experimental animals. Indian J Med Res 148:681. https://doi.org/10.4103/ijmr.IJMR_149_18
Boffetta P, Hecht S, Gray N, Gupta P, Straif K (2008) Smokeless tobacco and cancer. Lancet Oncol 9:667–675. https://doi.org/10.1016/S1470-2045(08)70173-6
Guha N, Warnakulasuriya S, Vlaanderen J, Straif K (2014) Betel quid chewing and the risk of oral and oropharyngeal cancers: a meta-analysis with implications for cancer control. Int J Cancer 135:1433–1443. https://doi.org/10.1002/ijc.28643
Sinha DN, Suliankatchi RA, Gupta PC, Thamarangsi T, Agarwal N, Parascandola M, Mehrotra R (2018) Global burden of all-cause and cause-specific mortality due to smokeless tobacco use: systematic review and meta-analysis. Tob Control 27:35–42. https://doi.org/10.1136/tobaccocontrol-2016-053302
Huang H-M, Cheng J-J, Liu C-M, Lin K-N (2006) Mucosal healing and mucociliary transport change after endoscopic sinus surgery in children with chronic maxillary sinusitis. Int J Pediatr Otorhinolaryngol 70:1361–1367. https://doi.org/10.1016/j.ijporl.2006.01.016
Deniz M, Gultekin E, Ciftci Z, Alp R, Ozdemir DN, Isik A, Demirel OB (2014) Nasal mucociliary clearance in obstructive sleep apnea syndrome patients. Am J Rhinol Allergy 28:e178–e180. https://doi.org/10.2500/ajra.2014.28.4094
Utiyama DMO, Yoshida CT, Goto DM, de Santana CT, de Paula SU, Koczulla AR, Saldiva PHN, Nakagawa NK (2016) The effects of smoking and smoking cessation on nasal mucociliary clearance, mucus properties and inflammation. Clinics (Sao Paulo) 71:344–350. https://doi.org/10.6061/clinics/2016(06)10
di Gıuda D, Galli J, Calcagni ML, Corina L, Paludetti G, Ottaviani F, de Rossi G (2000) Rhinoscintigraphy: a simple radioisotope technique to study the mucociliary system. Clin Nucl Med 25:127. https://doi.org/10.1097/00003072-200002000-00010
Habesoglu M, Demir K, Yumusakhuylu AC, Sahin Yilmaz A, Oysu C (2012) Does passive smoking have an effect on nasal mucociliary clearance? Otolaryngol Head Neck Surg 147:152–156. https://doi.org/10.1177/0194599812439004
Valía PP, Valero FC, Pardo JM, Rentero DB, Monte CG (2008) Saccharin test for the study of mucociliary clearance: reference values for a Spanish population. Arch Bronconeumol 44:540–545. https://doi.org/10.1016/S1579-2129(08)60100-7
Mutti S, Reid JL, Gupta PC, Pednekar MS, Dhumal G, Nargis N, Hussain AG, Hammond D (2016) Patterns of use and perceptions of harm of smokeless tobacco in Navi Mumbai, India and Dhaka, Bangladesh. Indian J Community Med 41:280. https://doi.org/10.4103/0970-0218.193337
Boyle P, Ariyaratne MY, Barrington R, Bartelink H, Bartsch G, Berns A, de Valeriola D, Dinshaw KA, Eggermont AM, Gray N (2006) Tobacco: deadly in any form or disguise. Lancet 367:1710–1712. https://doi.org/10.1016/S0140-6736(06)68747-3
Lorenzi G, Böhm G, Guimarães E, Vaz C, King M, Saldiva P (1992) Correlation between rheologic properties and in vitro ciliary transport of rat nasal mucus. Biorheology 29:433–440. https://doi.org/10.3233/bir-1992-29406
Kılıç O, Yılmaz AŞ, Oysu Ç (2020) The effect of passive smoking on mucociliary clearance and ınferior concha reactivity. Am J Rhinol Allergy. https://doi.org/10.1177/1945892420967614
Arıcıgil M, Arbağ H (2018) Hookah smoking impairs nasal mucociliary clearance. Tob Induc Dis. https://doi.org/10.18332/tid/85067
Madan R, Matalon S, Vivero M (2016) Spectrum of smoking-related lung diseases. J Thoracic Imaging 31:78–91. https://doi.org/10.1097/RTI.0000000000000185
Navarrette CR, Sisson JH, Nance E, Allen-Gipson D, Hanes J, Wyatt TA (2012) Particulate matter in cigarette smoke increases ciliary axoneme beating through mechanical stimulation. J Aerosol Med Pulm Drug Deliv 25:159–168. https://doi.org/10.1089/jamp.2011.0890
Gudnadóttir AÝ, Ólafsdóttir IS, Middelveld R, Ekerljung L, Forsberg B, Franklin K, Lindberg E, Janson C (2017) An investigation on the use of snus and its association with respiratory and sleep-related symptoms: a cross-sectional population study. BMJ Open 7:e015486. https://doi.org/10.1136/bmjopen-2016-015486
Hounkpatin S, Flatin M, Bouraima A, Amegan H, Adios MT, Adjibabi W (2020) Rhinologic signs associated with snuff taking. Eur Ann Otorhinolaryngol Head Neck Dis 137:43–45. https://doi.org/10.1016/j.anorl.2019.10.002
Hajat C, Stein E, Ramstrom L, Shantikumar S, Polosa R (2021) The health impact of smokeless tobacco products: a systematic review. Harm Reduct J 18:1–21. https://doi.org/10.1186/s12954-021-00557-6
Funding
This study was funded by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was done in the ENT Department of Kahramanmaras Sutcu Imam University, Faculty of Medicine. Each of the authors has contributed to, read and approved this manuscript.
Rights and permissions
About this article
Cite this article
Kara, İ., Cınar, O.F., Doğaner, A. et al. Does Maras powder affect the nasal mucociliary clearence?. Eur Arch Otorhinolaryngol 279, 5701–5706 (2022). https://doi.org/10.1007/s00405-022-07487-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07487-4