Abstract
Objective
The objective of this study was to appreciate the tolerance and convenience of a new FFP2 mask allowed the realization of nasal examination in period of pandemic.
Methods
Fifty-one patients were prospectively recruited from two European hospitals to test the FFP2 mask prototype. The following outcomes were evaluated in patients after the clinical examination: fear about coronavirus disease 2019 (COVID-19) infection; easiness of mask placement; tolerability; reassurance; and overall satisfaction about the use of this kind of mask in a pandemic context. Seven otolaryngologists evaluated the mask acceptance and usefulness in patients through a standardized physician-reported outcome questionnaire.
Results
Fifty patients completed the evaluation. There were 25 males and 25 females. The mean age of patients was 41 years. Ninety percent of patients considered that the use of the mask reduced the risk to be infected during the examination. Seventy percent of patients reported high or very high satisfaction and should recommend mask to other patients in pandemic period. The realization of nasal examination was easier with optic compared with flexible trans-nasal examination (p = 0.001), which significantly impacted the satisfaction level of physician (p = 0.001). The physician difficulty to perform the examination significantly impacted the satisfactory of patient (p = 0.033).
Conclusion
The new bioserenity FFP2 mask allows the realization of the trans-nasal endoscopic examination during a pandemic. The use of this mask requires little training period of physician. The use of this mask prototype is well received by patients who reported better perception of self-protection against the virus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic started in December 2019 and the virus spread worldwide. To control the virus spread, the governments of many countries imposed lockdown, social distancing, and masks wear. Despite this, the November 3, 2021, 246,951,274 individuals have been infected worldwide, corresponding to 5,004,855 deaths [1].
The FFP2 mask has been demonstrated as effective in the protection of individuals and their entourage but in some situation, individuals must remove it. One of these situations remains the otolaryngological examination of mouth and nasal vestibule and the trans-nasal examination. In these situations, the risk of contamination from patient to otolaryngologist increases and vice versa, otolaryngologist being physicians at high risk of contamination [2]. Indeed, the virus droplet projection through cough process may reach 4 m, [3] while it has been demonstrated that the virus may be hanged 3 h in the air room. [4]
In the present study, we aimed to develop a FFP2 mask that is more protective for both patient and otolaryngologist during the trans-nasal examination and evaluate the satisfaction and tolerance of mask wearing.
Methods
From May to October 2021, patients were prospectively recruited from Foch Hospital (Paris, France) and CHU La Timone (AP-HM, Marseille, France) to test a new FFP2 mask developed to protect both physician and patient from aerosolized infection, such as COVID-19. Otolaryngologists explained the concept and objective of the mask in consultation and proposed to patient to test it during the optic or flexible trans-nasal examination. Institutional review board was not required for this study.
Mask development
The FFP2 mask was developed by BioSerenity® (Paris, France). The designer of the mask (Antoine Giovanni MD, PhD) aimed to develop a FFP2 mask allowing the realization of flexible fiberoptic or rigid nasal optic examination in patients who keep a mask. Several prototypes were developed and tested on individuals to get a final product reporting satisfaction of both patients and engineers. The product development was based on complex flow dynamics particles flow simulations on the medical situations to ensure the management of potential exposures. Materials have been upgraded to focus on viral agents and not only particulate and to provide an FFP levels standard protection. The project was driven from defined requirements (e.g., no nasal leak, easy to wear for the patient, easy to use for the practician) to the industrialization phase to have reliable process and to be trustable products. The medical device regulatory file was finalized and validated by the notify body, the product has the C.E. label.
Patient and physician-reported outcome questionnaires
The following outcomes were evaluated in patients: fear to be infected with COVID-19 in daily live; understand of the concept; self-protection regarding a potential risk of virus transmission by the physician; reassurance to protect the physician by a potential risk of virus transmission; interest of the concept idea; easiness to set the mask; annoyance by the examination; recommendation to other patients, and overall satisfaction regarding the mask. The patient-reported outcome questionnaire is available in Appendix 1.
The following outcomes were evaluated in physicians after the consultation: easiness to set the mask; annoyance to perform the examination; physician evaluation of patient understand of the concept; patient acceptability of the mask; patient reassurance about the risk to transmit the virus from physician to patient; patient reassurance about the risk to transmit the virus from patient to the physician; recommendation of the mask to colleagues; future use in case of new pandemic, and overall satisfaction (Appendix 2). Patients or physicians had to assess the propositions with the following 5-point Likert scale: strongly disagree (1), disagree (2), no opinion (3), agree (4), and strongly agree (5).
Statistical methods
Statistical analyses were performed using the Statistical Package for the Social Sciences for Windows (SPSS version 27.0; IBM Corp, Armonk, NY, USA). Descriptive analyses were performed with Chi-square. A correlation analysis was performed to study the outcome associations. A level of significance of p < 0.05 was used.
Results
Fifty patients participated in this study. Seven physicians have tested the mask through flexible trans-nasal examination (N = 37) or rigid optics (N = 13). The mean age of patients was 41 years, and there were 25 females and 25 males.
Patient outcomes
The questionnaire revealed that 32% of patients had fear of COVID-19 infection, while 14% had no opinion about the question (Table 1). Most of patients understood the concept (88%). The mask was easy to set in 74% of cases, while in 20% of cases, patients had no opinion. Patients believed that they were protected against the infection during the examination in 80% of cases, while they believed that the mask protected the physician in 86% of cases. In 76% of cases, they found the concept interesting. Thirty-two percent of patients found the masks uncomfortable during the examination. High and very high overall satisfaction outcomes about the mask were reported by 70% of patient, whereas 52% should recommend the use of the masks to other patients.
Physician outcomes
Most of otolaryngologists (90%) find that the mask setting was easy (Table 2). In 20 cases (40%), otolaryngologist reported difficulties to find the nasal vestibule with flexible trans-nasal examination. The patients understand the concept (94%) and accept positively the mask (88%) according to the otolaryngologist perception. In 62% of cases, otolaryngologists believed that the patient was reassured regarding the risk to be infected by the physician, while in 40% of cases, the otolaryngologist did not know. The otolaryngologist was reassured with the mask to be protected against contamination by the patient in 90% of cases. In case of pandemic, 82% of otolaryngologists will be ready to use the mask and 54% will recommend the mask to other colleagues. Overall, 56% of otolaryngologists reported high or very high satisfaction outcome.
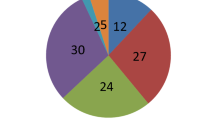
Otolaryngologist reported that the rigid optic examination was associated with better convenience during the examination in comparison with flexible trans-nasal examination (p = 0.015; Fig. 1A). The use of rigid optic examination was associated with better recommendation outcome (p = 0.001; Fig. 1B) and better acceptance outcome compared with the use of flexible trans-nasal examination (p = 0.033; Fig. 1C). Otolaryngologists who used optics rigid are more satisfied by the mask compared with those who used flexible trans-nasal examination (p < 0.001 Fig. 1D).
Comparison of outcomes according to the type of examination. Figure 1A reports the convenience of physician during the examination comparing rigid or trans-nasal examination is reported. The use of rigid optic examination was associated with better recommendation outcome (1B) and better acceptance outcome compared with the use of flexible trans-nasal examination (1C). Otolaryngologists who used optics rigid are more satisfied by the mask compared with those who used flexible trans-nasal examination (1D).
Association study
The more the physician had difficulties to perform the examination, at most the patient reported negative overall satisfaction score (rs = 0.316; p = 0.033) and, therefore, should not recommend the mask to other patients (rs = 0.295; p = 0.047). The enthusiasm of patient regarding the mask positively predicted the physician response in recommendation (rs = 0.347; p = 0.017) and the overall satisfaction (rs = 0.354; p = 0.015) outcomes. At most the patient was not afraid to be infected in daily life by COVID-19, at most they were reassured by the mask (rs = − 0.370; p = 0.010). Satisfaction responses of physicians and patients were positively correlated (rs = 0.339; p = 0.021) as well as the recommendation outcomes of both responder groups (rs = 0.378; p = 0.010).
Discussion
The high risk of COVID-19 transmissibility to the otolaryngologist led to the development of new protective strategies for the care workers. In this study, we reported the development of a new prototype of FFP2 mask allowing the realization of trans-nasal examination. In the present study, we observed two main findings.
First, the use of the mask had a significant positive impact on patient assurance regarding the risk to be infected or to infect the otolaryngologist. This point may strengthen the patient-physician relationship and the quality of care provided by the otolaryngologist. Indeed, it has been demonstrated that a substantial number of patients avoided hospital, consultations, and related cares during the pandemic because fear of catching the COVID-19 [5, 6].
Second, otolaryngologists were overall favorable to use the mask in pandemic period, but the use may involve a short learning period especially for flexible trans-nasal examination. Indeed, the location of the nasal vestibule may be difficult in the first uses of the mask.
The literature comparison remains limited because to the best of our knowledge, there is no data reporting the development and the validation of similar FFP2 mask concept. This mask may represent an additional tool to protect otolaryngologists and to reassure patients about the risk of virus transmission. Other recent tools were developed to protect the otolaryngologists, including simple modification of the standard headlight used during the ear, nose, and throat visit [7], droplet protective barrier to the patient’s chair [7], or UV-C light and negative air pressure chamber for endoscopic examination [8].
The first limitation of the present study is the low number of patients and the low number of otolaryngologists who used the mask. However, this is a preliminary study that aimed to investigate the acceptance and tolerance of this new FFP2 mask. The second limitation of this study is the lack of evaluation of the virus risk transmission according to the use of the mask.
The main advantage of BioSerenity® FFP2 mask remains the possibility to use it everywhere (e.g., emergency room, intensive care unit, private consultation) by otolaryngologists who frequently perform trans-nasal examination. Moreover, this kind of mask could be useful in gastroenterology for gastrointestinal endoscopy procedure. Future controlled studies are needed to shed light the advantages of this mask over the current practice and to determine the prevalence of virus transmission according to the use of the mask.
Conclusion
The new BioSerenity® FFP2 mask allows the realization of flexible or rigid trans-nasal flexible examination during the pandemic with better outcomes for rigid examination. The use of this mask may require learning period but may improve the patient-physician relationship, and the feeling of protection of both during the examination.
References
Covid19. (2021) Who.int consulted November 3
Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E (2020) COVID-19 and the otolaryngologist: preliminary evidencebased review. Laryngoscope 130(11):2537–2543. https://doi.org/10.1002/lary.28672
Guo ZD, Wang ZY, Zhang SF, Li X, Li L, Li C, Cui Y, Fu RB, Dong YZ, Chi XY, Zhang MY, Liu K, Cao C, Liu B, Zhang K, Gao YW, Lu B, Chen W (2020) Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis 26(7):1583–1591. https://doi.org/10.3201/eid2607.200885
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382(16):1564–1567. https://doi.org/10.1056/NEJMc2004973
Mayo-Yáñez M, Palacios-García JM, Calvo-Henríquez C, Ayad T, Saydy N, León X, Parente P, Chiesa-Estomba CM, Lechien JR (2021) COVID-19 pandemic and its impact on the management of head and neck cancer in the Spanish healthcare system. Int Arch Otorhinolaryngol 25(4):e610–e615. https://doi.org/10.1055/s-0041-1736425
Adigwu Y, Osterbauer B, Hochstim C (2021) Disparities in access to pediatric Otolaryngology care during the COVID-19pandemic. Ann Otol Rhinol Laryngol. https://doi.org/10.1177/00034894211048790
Farneti P, Sorace F, Tasca I (2020) Personal protective equipment for ENT activity during COVID-19 pandemic. Eur Arch Otorhinolaryngol 277(10):2933–2935. https://doi.org/10.1007/s00405-020-06177-3
Sayin İ, Devecioğlu İ, Yazıcı ZM (2020) A closed chamber ENT examination unit for aerosol-generating endoscopic examinations of COVID-19 patients. Ear Nose Throat J 99(9):594–596. https://doi.org/10.1177/0145561320931216
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethics approval
Research involving human participants and/or animals: IRB was not required for this study.
Consent to participate
Patients agreed to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Marrez, L.G., Radulesco, T., Chiesa-Estomba, C.M. et al. Proof-of-concept of a new FFP2 mask adapted to Otolaryngological practice in pandemic: a prospective study. Eur Arch Otorhinolaryngol 279, 3563–3567 (2022). https://doi.org/10.1007/s00405-022-07319-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07319-5