Abstract
Purpose
Platelet-rich fibrin (PRF) results in satisfactory wound healing. This analysis focuses on assessing the effectiveness of PRF in the treatment of tympanic membrane (TM) perforations.
Materials and methods
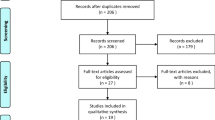
The literature was searched using PubMed, Embase, Cochrane Library and Web of Science databases from inception to February 28th, 2021. The following healing and hearing outcomes were measured: closure rate, pre-and postoperative auditory results, and incidence of postoperative infections. Data were pooled and expressed as the odds ratio (OR).
Results
Ten studies were eligible for qualitative review, and seven of them were included for the final quantitative comparison. The OR for the closure rate of acute perforations was 4.30 (95% CI 1.35–13.70, I2 = 0%), and the OR in the chronic subgroup was 5.42 (95% CI 2.57–11.43, I2 = 0%). The total OR value for the completed closure rate was 5.10 (95% CI 2.72–9.54, I2 = 0%), indicating that the utilization of PRF can enhance the closure of both acute and chronic perforations. The qualitative review did not find improved hearing results with the use of PRF. In addition to promoting closure, PRF can reduce the incidence of infections (OR = 0.14). The sensitivity analysis did not change the final results, and there was no publication bias in this analysis.
Conclusion
PRF can increase the closure rate of acute perforations, enhance the survival rate of autografts in TM surgeries and reduce the incidence of infections. However, the literature indicates that PRF does not influence the hearing outcomes. This study shows that PRF is an effective agent for TM regeneration.





Similar content being viewed by others
References
Shen Y, Redmond SL, Teh BM et al (2013) Tympanic membrane repair using silk fibroin and acellular collagen scaffolds. Laryngoscope 123:1976–1982. https://doi.org/10.1002/lary.23940
Lin YS, Lin LC, Lee FP et al (2009) The prevalence of chronic otitis media and its complication rates in teenagers and adult patients. Otolaryngol Head Neck Surg 140:165–170. https://doi.org/10.1016/j.otohns.2008.10.020
Huang J, Teh BM, Eikelboom RH et al (2020) The effectiveness of bFGF in the treatment of tympanic membrane perforations: a systematic review and meta-analysis. Otol Neurotol 41:782–790. https://doi.org/10.1097/MAO.0000000000002628
Shen Y, Redmond SL, Teh BM et al (2013) Scaffolds for tympanic membrane regeneration in rats. Tissue Eng Part A 19:657–668. https://doi.org/10.1089/ten.TEA.2012.0053
Stavrakas M, Karkos PD, Markou K et al (2016) Platelet-rich plasma in otolaryngology. J Laryngol Otol 130:1098–1102. https://doi.org/10.1017/S0022215116009403
Riaz N, Ajmal M, Khan MS (2021) Efficacy of platelet rich fibrin in myringoplasty. Pak J Med Sci. https://doi.org/10.12669/pjms.37.1.3059
Awady MKE, Sharkawy MEL, Mohamed NMA (2021) Effect of addition of platelet-rich fibrin to tragal perichondrium graft in the endoscopic trans-canal myringoplasty. Egypt J Otolaryngol 37:11. https://doi.org/10.1186/s43163-021-00068-y
Gökçe KS, Özdaş T (2019) Impact of platelet-rich fibrin therapy in tympanoplasty type 1 surgery on graft survival and frequency-specific hearing outcomes: a retrospective analysis in patients with tympanic membrane perforation due to chronic otitis media. J Laryngol Otol 133:1068–1073. https://doi.org/10.1017/S0022215119002391
Nair NP, Alexander A, Abhishekh B et al (2019) Safety and efficacy of autologous platelet-rich fibrin on graft uptake in myringoplasty: a randomized controlled trial. Int Arch Otorhinolaryngol 23:77–82. https://doi.org/10.1055/s-0038-1649495
Hosam M, Shaker M, Aboulwafa A (2017) Effect of topical use of platelet-rich fibrin in repairing central tympanic membrane perforation using the endoscopic inlay butterfly cartilage myringoplasty technique. Egypt J Otolaryngol 33:557. https://doi.org/10.4103/ejo.ejo_7_17
Gür OE, Ensari N, Öztürk MT et al (2016) Use of a platelet-rich fibrin membrane to repair traumatic tympanic membrane perforations: a comparative study. Acta Otolaryngol 136:1017–1023. https://doi.org/10.1080/00016489.2016.1183042
Habesoglu M, Oysu C, Sahin S et al (2014) Platelet-rich fibrin plays a role on healing of acute-traumatic ear drum perforation. J Craniofac Surg 25:2056–2058. https://doi.org/10.1097/SCS.0000000000001140
Shukla A, Kaurav YS, Vatsyayan R (2020) Novel use of platelet rich fibrin membrane in transcanal myringoplasty: a prospective study. Indian J Otolaryngol Head Neck Surg 72:355–362. https://doi.org/10.1007/s12070-020-01851-8
Kumar RD (2019) Application of platelet rich fibrin matrix to repair traumatic tympanic membrane perforations: a pilot study. Indian J Otolaryngol Head Neck Surg 71:1126–1134. https://doi.org/10.1007/s12070-017-1239-6
Garin P, Peerbaccus Y, Mullier F et al (2014) Platelet-rich fibrin (PRF): an autologous packing material for middle ear microsurgery. B-ENT 10:27–34
Kaya İ, Şahin FF, Tanrıverdi OH et al (2021) A novel graft-harvesting technique in tympanoplasty: the cubism graft. Eur Arch Otorhinolaryngol 278:1289–1292. https://doi.org/10.1007/s00405-021-06646-3
Huang J, Shi Y, Wu L et al (2021) Comparative efficacy of platelet-rich plasma applied in myringoplasty: a systematic review and meta-analysis. PLoS ONE 161:e0245968. https://doi.org/10.1371/journal.pone.0245968
Higgins JPT, Green S (2013) Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Cochrane Collaboration, London
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Ensari N, Gür ÖE, Öztürk MT et al (2017) The effect of platelet-rich fibrin membrane on the repair of perforated tympanic membrane: an experimental study. Acta Otolaryngol 137:695–699. https://doi.org/10.1080/00016489.2017.1282169
Everts PAM, Knape JTA, Weibrich G et al (2006) Platelet-rich plasma and platelet gel: a review. J Extra Corpor Technol 38:174–187. https://doi.org/10.1177/0363546509349921
Lee DY, Kim YH (2018) Can Fat-plug myringoplasty be a good alternative to formal myringoplasty? A systematic review and meta-analysis. Otol Neurotol 39:403–409. https://doi.org/10.1097/MAO.0000000000001732
Kristensen S (1992) Spontaneous healing of traumatic tympanic membrane perforations in man: a century of experience. J Laryngol Otol 106:1037–1050. https://doi.org/10.1017/S0022215100121723
Sánchez BA, Lora PD, Villafruela SM et al (2015) Pediatric myringoplasty: prognostic factors in surgical outcome and hearing threshold recovery. Acta Otolaryngol 135:1233–1237. https://doi.org/10.3109/00016489.2015.1069396
Visvanathan V, Vallamkondu V, Bhimrao SK (2018) Achieving a successful closure of an anterior tympanic membrane perforation: evidence-based systematic review. Otolaryngol Head Neck Surg 158:1011–1015. https://doi.org/10.1177/0194599818764335
Alhabib SF, Saliba I (2017) Hyaluronic acid fat graft myringoplasty versus autologous platelet rich plasma. J Clin Med Res 9(1):30–34
Ghanad I, Polanik MD, Trakimas DR et al (2021) A systematic review of nonautologous graft materials used in human tympanoplasty. Laryngoscope 131:392–400. https://doi.org/10.1002/lary.28914
Funding
This study was supported by the National Natural Science Foundation of China (No.81670920), Zhejiang Provincial Natural Science Foundation (No.LY15H130003), Zhejiang Provincial Medical and Health Science Research Foundation (No.2020RC107 and No.2020KY274), Ningbo Natural Science Foundation (No.2018A610363), and Ningbo Huimin Technology Research and Development Project Fund (No.2015C50026).
Author information
Authors and Affiliations
Contributions
All persons designated as the authors have participated sufficiently in the work to take public responsibility for the content of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, J., Teh, B.M., Zhou, C. et al. Tympanic membrane regeneration using platelet-rich fibrin: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 279, 557–565 (2022). https://doi.org/10.1007/s00405-021-06915-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06915-1