Abstract
Background
It has been suggested that gestational diabetes mellitus (GDM) alters the growth trajectory of a fetus and increases the risk of abnormal birth weight. In spite of this, there is still a significant debate regarding the mode and optimal timing of diagnosing this condition. Our aim was to determine fetal growth velocity and birth biometry in pregnant women with GDM at varying risk levels.
Methods
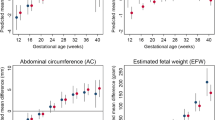
We conducted a cohort study involving 1023 pregnant women at a maternity hospital in Ma’anshan, China. All women completed an oral glucose tolerance test at 24–28 weeks’ gestation. We measured fetal head circumference (HC), femoral length (FL), abdominal circumference (AC), biparietal diameter (BPD), and estimate fetal weight (EFW) by ultrasound at 17, 24, 31, and 35 weeks’ gestation, respectively.
Results
Overall, 5115 ultrasound scans were performed. Among both low-risk and medium–high-risk pregnant women at 17–24 weeks’ gestation, GDM exposure was associated with an increase in fetal growth velocity. Neonates born to women with GDM at medium–high risk had significantly larger birth weights than those born to women without GDM, while this was not observed in women at low risk.
Conclusion
In medium–high-risk pregnant women, exposure to GDM has a greater effect on the fetus, leading to abnormal fetal growth velocity that lasts beyond week 24. It is evident from our results that the effects of GDM on fetal growth differ between medium–high-risk pregnant women and low-risk pregnant women, and therefore a different screening program based on the risk factor for GDM is warranted.


Similar content being viewed by others
Data availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Moyer VA (2014) Screening for gestational diabetes mellitus: U.S. preventive services task force recommendation statement. Ann Intern Med 160:414–420. https://doi.org/10.7326/m13-2905
Mirabelli M, Chiefari E, Tocci V, Greco E, Foti D, Brunetti A (2021) Gestational diabetes: implications for fetal growth, intervention timing, and treatment options. Curr Opin Pharmacol 60:1–10. https://doi.org/10.1016/j.coph.2021.06.003
Lawlor DA, Lichtenstein P, Långström N (2011) Association of maternal diabetes mellitus in pregnancy with offspring adiposity into early adulthood: sibling study in a prospective cohort of 280,866 men from 248,293 families. Circulation 123:258–265. https://doi.org/10.1161/CIRCULATIONAHA.110.980169
Association AD (2019) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care 42:S13–S28. https://doi.org/10.2337/dc19-S002
ACOG (2018) ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstet Gynecol 131:e49–e64. https://doi.org/10.1097/aog.0000000000002501
Blumer I, Hadar E, Hadden DR, Jovanovič L, Mestman JH, Murad MH et al (2013) Diabetes and pregnancy: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 98:4227–4249. https://doi.org/10.1210/jc.2013-2465
Catalano PM, Thomas A, Huston-Presley L, Amini SB (2003) Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol 189:1698–1704. https://doi.org/10.1016/s0002-9378(03)00828-7
Kim W, Park SK, Kim YL (2021) Fetal abdominal obesity detected at 24 to 28 weeks of gestation persists until delivery despite management of gestational diabetes mellitus. Diabetes Metab J 45:547–557. https://doi.org/10.4093/dmj.2020.0078
Wong SF, Chan FY, Oats JJ, McIntyre DH (2002) Fetal growth spurt and pregestational diabetic pregnancy. Diabetes Care 25:1681–1684. https://doi.org/10.2337/diacare.25.10.1681
Li M, Hinkle SN, Grantz KL, Kim S, Grewal J, Grobman WA et al (2020) Glycaemic status during pregnancy and longitudinal measures of fetal growth in a multi-racial US population: a prospective cohort study. Lancet Diabetes Endocrinol 8:292–300. https://doi.org/10.1016/S2213-8587(20)30024-3
Akiba Y, Ikenoue S, Endo T, Kasuga Y, Ochiai D, Miyakoshi K et al (2021) Differences in fetal fractional limb volume changes in normal and gestational diabetic pregnancies: an exploratory observational study. BJOG 128:329–335. https://doi.org/10.1111/1471-0528.16265
Farrar D, Simmonds M, Griffin S, Duarte A, Lawlor DA, Sculpher M et al (2016) The identification and treatment of women with hyperglycaemia in pregnancy: an analysis of individual participant data, systematic reviews, meta-analyses and an economic evaluation. Health Technol Assess 20:1–348. https://doi.org/10.3310/hta20860
Sovio U, Murphy HR, Smith GC (2016) Accelerated fetal growth prior to diagnosis of gestational diabetes mellitus: a prospective cohort study of nulliparous women. Diabetes Care 39:982–987. https://doi.org/10.2337/dc16-0160
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352:2477–2486. https://doi.org/10.1056/NEJMoa042973
Simmons D, Nema J, Parton C, Vizza L, Robertson A, Rajagopal R et al (2018) The treatment of booking gestational diabetes mellitus (TOBOGM) pilot randomised controlled trial. BMC Pregnancy Childbirth 18:151. https://doi.org/10.1186/s12884-018-1809-y
Kim W, Park SK, Kim YL (2019) Gestational diabetes mellitus diagnosed at 24 to 28 weeks of gestation in older and obese Women: Is it too late? PLoS One. 14:e0225955. https://doi.org/10.1371/journal.pone.0225955
Quaresima P, Visconti F, Chiefari E, Mirabelli M, Borelli M, Caroleo P et al (2020) Appropriate timing of gestational diabetes mellitus diagnosis in medium- and low-risk women: effectiveness of the Italian NHS recommendations in preventing fetal macrosomia. J Diabetes Res 2020:5393952. https://doi.org/10.1155/2020/5393952
Yf F, Xh Z, Xq Z, Ys X, Lq C (2022) Construction of risk prediction model for gestational diabetes mellitus and evaluation of prediction efficiency. Matern Child Health Care China 37:2133–7. https://doi.org/10.19829/j.zgfybj.issn.1001-4411.2022.12.001
Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline (2014). Diabetes Res Clin Pract 103(3):341–363. https://doi.org/10.1016/j.diabres.2013.10.012
Gupta Y, Kalra B, Baruah MP, Singla R, Kalra S (2015) Updated guidelines on screening for gestational diabetes. Int J Womens Health 7:539–550. https://doi.org/10.2147/IJWH.S82046
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK (1985) Estimation of fetal weight with the use of head, body, and femur measurements–a prospective study. Am J Obstet Gynecol 151:333–337. https://doi.org/10.1016/0002-9378(85)90298-4
Grantz KL, Kim S, Grobman WA, Newman R, Owen J, Skupski D et al (2018) Fetal growth velocity: the NICHD fetal growth studies. Am J Obstet Gynecol 219(285):e1–e36. https://doi.org/10.1016/j.ajog.2018.05.016
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG et al (2014) International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384:857–868. https://doi.org/10.1016/s0140-6736(14)60932-6
Brand JS, West J, Tuffnell D, Bird PK, Wright J, Tilling K et al (2018) Gestational diabetes and ultrasound-assessed fetal growth in South Asian and White European women: findings from a prospective pregnancy cohort. BMC Med 16:203. https://doi.org/10.1186/s12916-018-1191-7
Sovio U, White IR, Dacey A, Pasupathy D, Smith GCS (2015) Screening for fetal growth restriction with universal third trimester ultrasonography in nulliparous women in the Pregnancy Outcome Prediction (POP) study: a prospective cohort study. Lancet 386:2089–2097. https://doi.org/10.1016/S0140-6736(15)00131-2
Miailhe G, Kayem G, Girard G, Legardeur H, Mandelbrot L (2015) Selective rather than universal screening for gestational diabetes mellitus? Eur J Obstet Gynecol Reprod Biol 191:95–100. https://doi.org/10.1016/j.ejogrb.2015.05.003
Avalos GE, Owens LA, Dunne F (2013) Applying current screening tools for gestational diabetes mellitus to a European population: is it time for change? Diabetes Care 36:3040–3044. https://doi.org/10.2337/dc12-2669
Feldman RK, Tieu RS, Yasumura L (2016) Gestational diabetes screening: The International Association of the Diabetes and Pregnancy Study Groups Compared With Carpenter-Coustan Screening. Obstet Gynecol 127:10–17. https://doi.org/10.1097/aog.0000000000001132
Griffin ME, Coffey M, Johnson H, Scanlon P, Foley M, Stronge J et al (2000) Universal vs. risk factor-based screening for gestational diabetes mellitus: detection rates, gestation at diagnosis and outcome. Diabet Med 17:26–32. https://doi.org/10.1046/j.1464-5491.2000.00214.x
Acknowledgements
The authors wish to acknowledge the support of the Anhui Medical University and Ma'anshan Maternal and Child Health Hospital, as well as the mothers who informed for our study.
Funding
This research was funded by the National Natural Science Foundation of China (Grant No. 82073565), and Scientific Research Promotion Plan of Anhui Medical University (Grant No. 2021xkjT013).
Author information
Authors and Affiliations
Contributions
XZ and JW: designed the research. XC and JW: wrote the original manuscript. KZ, XC, and CH: reviewed and edited the manuscript. YL, XW, WY, and YM: performed the experiments. ZL and MC: helped with data collection. JZ, GG, and KZ: performed the statistical analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Ethics approval was obtained from Anhui Medical University (No. 20200592).
Consent to participate
All study participants provided the written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Cheng, X., Li, ZH. et al. The effects of gestational diabetes mellitus on fetal growth: is it different for low-risk and medium–high-risk pregnant women?. Arch Gynecol Obstet (2023). https://doi.org/10.1007/s00404-023-07229-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-023-07229-9