Abstract
Purpose
In humans, granulosa cells (GCs) are part of the follicle and nourish the growing oocyte. GCs produce estrogen and, after ovulation, progesterone. They are embedded in a multicellular tissue structure of the ovary, which consists of a variety of different cell types that are essential for the physiological function of the ovary. However, the extent to which individual ovarian cell types contribute to overall functionality has not yet been fully elucidated. In this study, we aim to investigate the effects of co-culturing human granulosa cells with ovarian cancer cells on their progesterone and estrogen production in an in vitro model.
Methods
After seeding, the cells were stimulated with 200 µM forskolin in DMEM for 72 h and the medium of the different cell culture experiments was collected. Subsequently, progesterone and oestradiol concentrations were determined using an Elisa assay.
Results
Morphologically, it was striking that the cells self-organize and form spatially separated areas. Compared to culturing granulosa cells alone, co-culturing human granulosa cells together with the ovarian cancer cell line OvCar-3 resulted in a significant increase in progesterone production (20.3 ng/ml versus 50.2 ng/ml; p < 0.01).
Conclusions
Using a simple in vitro model, we highlight the importance of cellular crosstalk between different ovarian cells in a complex cellular network and that it strongly influences granulosa cell hormone production. This could have potential implications for the procedure of transplanting endocrine tissues after cryopreservation, as it highlights the importance of survival of all cells for the functionality of the transplanted tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The proposed in vitro model, using ovarian cells as an example, suggests that when ovarian tissue is re-transplanted, the cell types that are most severely damaged can determine the success or failure of the intervention. Furthermore, it indicates a remarkable influence of ovarian cancer cells on its cellular environment. |
Introduction
The ovaries—as part of the female reproductive organs—represent a polymorphic complex structure consisting of a multitude of different cell types, each with different functions. To ensure full functionality of the ovary as an organ, all tissue and cell types must interact with each other in a finely orchestrated manner [1, 2].
An essential feature of a morphologically and physiologically intact ovary is the ability to produce sex steroid hormones under the control of gonadotropins. It is well established that granulosa cells (GC) and theca cells (TC) play a key role in this physiological process, being the sites of estrogen and progesterone production. For in vitro studies on ovarian hormone production, GC-based in vitro cell model systems have been developed and provide a valuable tool for an analysis of molecular pathways in hormone production [3, 4]. The major source of human GCs for in vitro studies is usually derived from patients undergoing artificial reproductive technologies (ART). However, these cells are accessible only in limited amounts, which make it difficult to perform widespread experiments related to detailed molecular analysis. Furthermore, and because of the therapy-specific gonadotropin-stimulation with ovulation induction, clinically obtained GCs are mostly luteinized. These GCs have a restricted life span with a slow proliferation rate, and they do not stay viable in vitro after many passages [3, 5]. In addition, primary GCs derived from specific patients may exhibit very high variability, which further complicates the achievement of reproducible results. Due to these problems, permanent cell models with primary GCs are difficult to establish. Therefore, in in vitro studies, human GC cell lines are often considered an attractive option [3, 6]. For example, the immortalized Granulosa cell lines KGN and HGL- 5 have been shown to be valuable in ovarian functional studies [7]. While the KGN cell line produces significant amounts of progesterone after stimulation with cyclic adenosine monophosphate (cAMP) inducing agents other cell lines do not. The KGN cell line was therefore considered particularly useful for in vitro studies of ovarian steroid hormone production.
Recently, it was shown that cell-to-cell contact is a pre-requisite to improve cellular vitality and that a specific microenvironment is necessary for promotion of endocrine function in various tissues including the ovary [8,9,10]. In addition, Fozzatti and co-authors have shown that cancer development and cancer progression depend on the mutual interaction between growing tumor cells and their surrounding cellular microenvironment [11].
In the ovary. the influence of other cells on GC triggered hormonal production has not been extensively studied. We hypothesize that GC surrounding cells may have an impact on hormone production of GCs. To address this question, we developed a simple two-cell model consisting of the human granulosa cell line KGN and the human carcinoma cell line OvCar-3 and analyzed the impact of this ovarian cell lines on hormone production by GCs.
Materials and methods
Except otherwise stated, all chemicals were obtained from Sigma (Sigma Chemical Co., St Louis, USA).
Cell culture and stimulation
The human granulosa cell line KGN was established by Nishi et al., 2001 from a stage III granulosa cell carcinoma [12]. Human KGN cells were cultured as previously described in DMEM (Dulbecco's Modified Eagle Medium), 10% FCS (Fetal calf serum) and a final concentration of 100 units/ml of penicillin and 100 µg/ml of streptomycin. (1% Pen/Strep) at 37 °C and 5% CO2 [13, 14]. Cell passages were 3–5.
The OvCar-3 cell line was cultivated in DMEM, 10% FCS (Fetal calf serum) and 1% Pen/Strep at 37 °C and 5% CO2. Cell passages were 2–5.
In brief, cells were seeded in 6-well plates at a density of 1 × 105 cells per ml. After 24 h, the medium was discarded and the remaining cells were washed twice with PBS and new media were added. Stimulation was carried by adding Forskolin to a final concentration of 1, 10, 50, 100, 200 µM, respectively. After 72 h, the supernatants were collected and stored for hormone quantification. In the case of co-culturing 5 × 104 of each cell line were seeded.
For cell passaging media was discarded and cells were treated with 3 ml Trypsin/EDTA solution containing 0.5 g trypsin and 0.2 g EDTA for 3 min at 37 °C, 5% CO2 after washing with PBS. The reaction was stopped by adding 2 ml of media containing 10% FCS. The detached cells were centrifuged for 5 min at 800 g. The media was discarded and new media was added to the cell pellet. The cell pellet was solved by gentle pipetting and cells were counted after Trypan Blue staining in a counting chamber.
Hormone quantification
Cell culture media was collected after 72 h of treatment and kept frozen at − 80 °C prior to testing.
Enzyme-linked immunosorbent assays (ELISAs) for estrogen (17beta-estradiol) and progesterone were performed using an ELISA kit according to the manufacturer's instructions (IBL international, Hamburg, Germany). Essentially, 25 µl of each sample was added in duplicate to a 96-well ELISA plate and incubated for 1 h at room temperature. Unbound material was washed out three times with washing solution. After addition of substrate solution, plates were incubated for an additional 15 min and stop solution was added. Absorbance (OD) was determined using a microplate reader (LumiStar Optima, BMG, Kumberg, Austria) at 450 nm.
Intra-assay variability and inter-assay variability for the progesterone ELISA ranged from 5.4 to 6.99% CV and from 4.34 to 9.96% CV, respectively. Intra-assay variability and inter-assay variability for the estrogen ELISA ranged from 8.70 to 90.23% CV and from 6.87 to 14.91% CV, respectively.
Statistics
The results of the hormone quantification experiments have been analyzed using ANOVA for independent samples followed by Tukey's HSD test. Differences were considered statistically significant at p < 0.05. Statistical analyses were performed at the statskingdom website at https://www.statskingdom.com.
Results
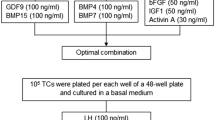
To investigate the effect on steroid hormone production by co-culturing a granulosa cell line and an epithelial carcinoma cell line, both cell lines were cultured under standard cell culture conditions separately and in a 1:1 ratio for 72 h. Morphologically, Fig. 1 shows that OvCar-3 and KGN together build distinguishable areas and the cell lines do not completely intermix. To investigate the hormone production capacity of the cells after culturing, we stimulated the cells with increasing amounts of forskolin, a cyclic adenosine monophosphate (cAMP)-inducing agent. Although OvCar-3 cells were not known to produce progesterone, we assessed this possibility by measuring progesterone concentration after stimulation with increasing amounts of forskolin. As demonstrated in Fig. 2, the stimulation of the OvCar-3 cells has no detectable effect including a concentration of 200 µM forskolin. Stimulation of the human granulosa cell line KGN demonstrates a concentration-dependent increase in progesterone production from 2.2 ng/ml at a progesterone concentration of 10 µM to an amount of 20.3 ng/ml at a concentration of 200 µM forskolin. When we cultivated both cell lines in a co-culture and a ratio of 1:1, we observed an increase in progesterone production from 2.8 ng/ml at a concentration of 10 µM forskolin up to 50.2 ng/ml at a concentration of 200 µM forskolin. We would like to point out that the amount of progesterone-producing KGN cells in these co-culture experiments is about half the amount of the KGN single-culture experiments. Additionally, we performed the same series of experiments and determined the estrogen production of both cell lines. However, significant amounts of estrogen was not detectable (data not shown).
Progesterone production. Effect of various concentrations of forskolin (1 µM to 200 µM) on the progesterone production of KGN, KGN + OvCar-3 and OvCAR-3 cells. All cultures were carried out for 72 h. Each bar represents mean ± STD. Individual experiments were repeated at least 4 times (n = 4). *Significant at a p-level < 0.05, **significant different at a p-level < 0.01
Discussion
In our study, we were able to show that the KGN–OvCar-3 co-culture system is a suitable model for demonstrating a stimulatory paracrine effect of co-culturing these two ovarian cell lines on progesterone production.
The progesterone synthesis of the human granulosa cell line KGN is mediated by a cAMP-triggered mechanism involving protein kinase A (PKA) dependent pathways [15]. Therefore, it is suitable to increase progesterone production either by increasing the amount of cAMP in the cells or by stimulating the enzyme adenylate cyclase with forskolin as we did in our study.
The progesterone amounts measured in our experiments for KGN cell culture after 72 h and stimulation with 200 µM forskolin are in the same physiological range as the values reported by Nishi et al., after (Bu)2cAMP stimulation (20.3 ng/ml vs. 15 ng/ml) (Nishi, Yanase et al. 2001). In the co-culture experiments together with OvCar-3 cells, however, we reached values up to 50.2 ng/ml, which corresponds to an increase by a factor of about five, taking into account that only half of the KGN cells have been seeded. A modulatory effect on cell viability and function by co-culturing different cell types was shown by Lancaster et al., for stem cell based organoid models [16]. In addition, a form of self-organization of granulosa cells and different other cells has already been described by Qiu et al. [17] as well as our group [18, 19]. De Souza and colleagues have shown that mesenchymal stem cells (MSC) increase viability and hormone production capacity of islets cells [20] and Jiang and colleagues reported a regulatory effect by endothelial cells on microglial cells [21]. A stimulatory effect by co-culturing on cell migration of cancer cells and on ovarian differentiation was reported by Dogan et al. [22] and Mackay et al. [23]. Our data are in line with results of other authors that co-cultivation of different cell types from ovarian origin can have a significant effect on hormone production. For example, the data of Qiu et al. have shown in in vitro experiments that co-culturing ovarian cortical stromal cells with primary granulosa cells derived from goat ovaries can stimulate both progesterone synthesis and cell proliferation.
Human granulosa cells are the site of hormone production in the ovary and play a crucial role in oocyte development trough interaction with a variety of other cells and cell types, resulting in a coordinated synergistic physiological process. It is justifiable to state that the failure of a small part of this system can lead to the breakdown of the entire physiological network. Our simple in vitro model of cooperation of granulosa cells and epithelial ovarian cells in hormone production supports the hypothesis that also in ovarian tissue, the cell types adjacent to the granulosa cells make an important contribution to hormone production and, thus, also to functionality. However, a restriction of the validity of our model is that we are dealing with two cell lines and therefore a generalization to the in vivo situation seems to be possible only to a limited extent. Our model uses cancer cells, not primary cells and cannot fully describe the complex interactions, which occur in vivo.
In the special situation of cryopreservation and re-transplantaion of ovarian tissue, fundamentally different cell types must cope with the stressors of freezing and the potentially toxic properties of the cryoprotective solutions. Therefore, special care should be taken in account to ensure that all cell types of the tissue are viable again after warming to return to full functionality after re-transplantation. Cell types that were most severely damaged by the procedure used may be decisive for the success or failure of the therapy in terms of different vitality.
Conclusion
Our model seems to be a simple and “easy to handle” model to study the effects of different cell types on the ability of human granulosa cells to produce progesterone. Furthermore, it highlights the relevance of survival of all cells in endocrine tissues after cryopreservation and subsequent re-transplantation.
Data availability
Data available on request from the authors.
References
Fan X, Bialecka M, Moustakas I, Lam E, Torrens-Juaneda V, Borggreven NV et al (2019) Single-cell reconstruction of follicular remodeling in the human adult ovary. Nat Commun 10:3164
Nelson SM, Telfer EE, Anderson RA (2013) The ageing ovary and uterus: new biological insights. Hum Reprod Update 19:67–83
Havelock JC, Rainey WE, Carr BR (2004) Ovarian granulosa cell lines. Mol Cell Endocrinol 228:67–78
Almeida CP, Ferreira MCF, Silveira CO, Campos JR, Borges IT, Baeta PG et al (2018) Clinical correlation of apoptosis in human granulosa cells-a review. Cell Biol Int 42:1276–1281
Lie BL, Leung E, Leung PC, Auersperg N (1996) Long-term growth and steroidogenic potential of human granulosa-lutein cells immortalized with SV40 large T antigen. Mol Cell Endocrinol 120:169–176
Rainey WH, Sawetawan C, Shay JW, Michael MD, Mathis JM, Kutteh W et al (1994) Transformation of human granulosa cells with the E6 and E7 regions of human papillomavirus. J Clin Endocrinol Metab 78:705–710
Ernst J, Grabiec U, Greither T, Fischer B, Dehghani F (2016) The endocannabinoid system in the human granulosa cell line KGN. Mol Cell Endocrinol 423:67–76
Félix-Martínez GJ, Nicolás-Mata A, Godínez-Fernández JR (2022) Computational reconstruction of pancreatic islets as a tool for structural and functional analysis. J Vis Exp. https://doi.org/10.3791/63351
Li Y, Zhang D, Xu L, Dong L, Zheng J, Lin Y et al (2019) Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol Immunol 16:908–920
Sugimura S, Kobayashi N, Okae H, Yamanouchi T, Matsuda H, Kojima T et al (2017) Transcriptomic signature of the follicular somatic compartment surrounding an oocyte with high developmental competence. Sci Rep 7:6815
Fozzatti L, Cheng SY (2020) Tumor cells and cancer-associated fibroblasts: a synergistic crosstalk to promote thyroid cancer. Endocrinol Metab (Seoul) 35:673–680
Nishi Y, Yanase T, Mu Y, Oba K, Ichino I, Saito M et al (2001) Establishment and characterization of a steroidogenic human granulosa-like tumor cell line, KGN, that expresses functional follicle-stimulating hormone receptor. Endocrinology 142:437–445
Xu Y, Zagoura D, Keck C, Pietrowski D (2006) Expression of Eph receptor tyrosine kinases and their ligands in human granulosa lutein cells and human umbilical vein endothelial cells. Exp Clin Endocrinol Diabetes 114:590–595
Hovemann I, Keck C, Fiebich BL, Pietrowski D (2008) Effects of selenium and mistletoe extracts on the expression of angiogenic growth factors and sprout formation in a spheroid cell culture system of human granulosa lutein cells. Geburtshilfe Frauenheilkd 68:620–624
Fang L, Guo Y, Li Y, Jia Q, Han X, Liu B et al (2022) Epigallocatechin-3-gallate stimulates StAR expression and progesterone production in human granulosa cells through the 67-kDa laminin receptor-mediated CREB signaling pathway. J Cell Physiol 237:687–695
Lancaster MA, Knoblich JA (2014) Organogenesis in a dish: modeling development and disease using organoid technologies. Science 345:1247125
Qiu M, Liu J, Han C, Wu B, Yang Z, Su F et al (2014) The influence of ovarian stromal/theca cells during in vitro culture on steroidogenesis, proliferation and apoptosis of granulosa cells derived from the goat ovary. Reprod Domest Anim 49:170–6
Becker J, Walz A, Daube S, Keck C, Pietrowski D (2007) Distinct responses of human granulosa lutein cells after hCG or LH stimulation in a spheroidal cell culture system. Mol Reprod Dev 74:1312–1316
Walz A, Keck C, Weber H, Kissel C, Pietrowski D (2005) Effects of luteinizing hormone and human chorionic gonadotropin on corpus luteum cells in a spheroid cell culture system. Mol Reprod Dev 72:98–104
de Souza BM, Bouças AP, Oliveira FD, Reis KP, Ziegelmann P, Bauer AC et al (2017) Effect of co-culture of mesenchymal stem/stromal cells with pancreatic islets on viability and function outcomes: a systematic review and meta-analysis. Islets 9:30–42
Jiang L, Womble T, Saporta S, Chen N, Sanberg CD, Sanberg PR et al (2010) Human umbilical cord blood cells decrease microglial survival in vitro. Stem Cells Dev 19:221–228
Doğan A, Demirci S, Apdik H, Apdik EA, Şahin F (2019) Mesenchymal stem cell isolation from pulp tissue and co-culture with cancer cells to study their interactions. J Vis Exp. https://doi.org/10.3791/58825
Mackay S, Willerton L, Ballingall CL, Henderson NJ, Smith RA (2004) Developing mouse Sertoli cells in vitro: effects on developing ovaries in co-culture and production of anti-Müllerian hormone. Cells Tissues Organs 177:79–86
Acknowledgements
Human KGN cells were a friendly kind gift by K. Horling Department of Anatomy and Cell Biology, Martin Luther University Faculty of Medicine, Halle (Saale), Germany. The human ovarian cancer cell line OvCar-3 were a friendly gift by Dr. D.C. Castillo-Tong (Medical University Vienna, Vienna, Austria).
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MG, DP and IH. The first draft of the manuscript was written by DP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Not applicable as this is a basic research study using established cell lines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pietrowski, D., Grgic, M., Haslinger, I. et al. Co-cultivation of human granulosa cells with ovarian cancer cells leads to a significant increase in progesterone production. Arch Gynecol Obstet 307, 1593–1597 (2023). https://doi.org/10.1007/s00404-023-06914-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-06914-z