Abstract
Purpose
There are few data on maternal and neonatal morbidities associated with shoulder dystocia (SD), depending on the use of fetal manipulation (FM). A prior 5-year study was conducted in our center in 2012 for this purpose. Our objective was to compare severe maternal and neonatal morbidities according to FM execution in a larger cohort.
Methods
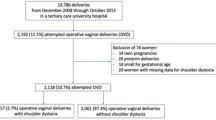
We conducted a retrospective study between 2007 and 2020. SD was considered when additional maneuvers were required to complete a delivery. Severe maternal morbidity was defined as the occurrence of obstetric anal sphincter injury (OASI). Severe neonatal morbidity was defined as Apgar < 7 at 5 min and/or cord arterial pH < 7.1 and/or or a permanent brachial plexus palsy. We studied these data in the FM group compared to the non- FM group.
Results
FM was associated with increased OASI rates (21.1% vs. 3.8%, OR = 6.72 [2.7–15.8]). We found no significant difference in severe neonatal morbidity. Maternal age > 35 and FM appear to be associated with the occurrence of OASI, with ORa = 13.3 [1.5–121.8] and ORa = 5.3 [2.2–12.8], respectively. FM was the only factor associated with the occurrence of severe neonatal morbidity (ORa = 2.3 [1.1–4.8]. The rate of episiotomy was significantly decreased (20% versus 5% p < 0.05) and there was an increase in the rate of SD managed with FM in our center.
Conclusion
FM is the only factor associated with an increased risk of OASI. In case of failure of non-FM maneuvers, the rapid implementation of FM maneuvers resulted in no difference regarding severe neonatal morbidity.


Similar content being viewed by others
References
Deneux-Tharaux C, Delorme P (2015) Epidemiology of SD. J Gynecol Obstet Biol Reprod (Paris) 44:1234–1247. https://doi.org/10.1016/j.jgyn.2015.09.036
American College of Obstretricians and Gynecologists (2017) Practice bulletin No 178: SD. Obstet Gynecol 129:e123–e133. https://doi.org/10.1097/AOG.0000000000002043
Ouzounian JG (2016) SD: incidence and risk factors. Clin Obstet Gynecol 59:791–794. https://doi.org/10.1097/GRF.0000000000000227
Sentilhes L, Sénat M-V, Boulogne A-I, Deneux-Tharaux C, Fuchs F, Legendre G et al (2016) SD: guidelines for clinical practice from the French college of gynecologists and obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol 203:156–161. https://doi.org/10.1016/j.ejogrb.2016.05.047
O’Leary BD, Ciprike V (2020) Anal sphincter injury associated with SD. J Matern Fetal Neonatal Med 33:3136–3140. https://doi.org/10.1080/14767058.2019.1569617
Levin G, Rottenstreich A, Tsur A, Cahan T, Yoeli-Ullman R, Shai D et al (2021) Risk factors for obstetric anal sphincter injury among parous women. Arch Gynecol Obstet 303:709–714. https://doi.org/10.1007/s00404-020-05806-w
Thubert T, Cardaillac C, Fritel X, Winer N, Dochez V (2018) Definition, epidemiology and risk factors of obstetric anal sphincter injuries: CNGOF perineal prevention and protection in obstetrics guidelines. Gynecol Obstet Fertil Senol 46(12):913–921. https://doi.org/10.1016/j.gofs.2018.10.028
Beta J, Khan N, Khalil A, Fiolna M, Ramadan G, Akolekar R (2019) Maternal and neonatal complications of fetal macrosomia: systematic review and meta-analysis. Ultrasound Obstet Gynecol 54:308–318. https://doi.org/10.1002/uog.20279
Dajani NK, Magann EF (2014) Complications of SD. Semin Perinatol 38:201–204. https://doi.org/10.1053/j.semperi.2014.04.005
Lopez E, Courtivron B, Saliba E (2015) Neonatal complications of SD: risk factors and management. J Gynecol Obstet Biol Reprod 44:1294–1302. https://doi.org/10.1016/j.jgyn.2015.09.049
Stallings SP, Edwards RK, Johnson JWC (2001) Correlation of head-to-body delivery intervals in SD and umbilical artery acidosis. Am J Obstet Gynecol 185:268–274. https://doi.org/10.1067/mob.2001.116730
Battin MR, van den Boom J, Oben G, McDonald G (2021) SD, umbilical cord blood gases and neonatal encephalopathy. Aust N Z J Obstet Gynaecol 61:604–606. https://doi.org/10.1111/ajo.13351
Moni S, Lee C, Goffman D (2016) SD: quality, safety, and risk management considerations. Clin Obstet Gynecol 59:841–852. https://doi.org/10.1097/GRF.0000000000000228
Chauhan SP, Chang KW-C, Ankumah N-AE, Yang LJ-S (2016) Neonatal brachial plexus palsy: obstetric factors associated with litigation. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2016.1252745
Zaami S, Busardò FP, Signore F, Felici N, Briganti V, Baglio G et al (2018) Obstetric brachial plexus palsy: a population-based retrospective case-control study and medicolegal considerations. J Matern-Fetal Neonatal Med Off J Eur Assoc Perinat Med Fed Asia Ocean Perinat Soc Int Soc Perinat Obstet 31:1412–1417. https://doi.org/10.1080/14767058.2017.1317737
Hall LW, Scott SD (2012) The second victim of adverse health care events. Nurs Clin North Am 47:383–393. https://doi.org/10.1016/j.cnur.2012.05.008
Gherman RB, Goodwin TM, Souter I, Neumann K, Ouzounian JG, Paul RH (1997) The McRoberts’ maneuver for the alleviation of SD: how successful is it? Am J Obstet Gynecol 176:656–661. https://doi.org/10.1016/s0002-9378(97)70565-9
Hill DA, Lense J, Roepcke F (2020) SD: managing an obstetric emergency. Am Fam Physician 102:84–90
Gachon B, Desseauve D, Fritel X, Pierre F (2016) Is FM during SD management associated with severe maternal and neonatal morbidities? Arch Gynecol Obstet 294:505–509. https://doi.org/10.1007/s00404-016-4013-1
American College of Obstetricians and Gynecologists (2021) Patient safety checklist No. 6: documenting SD - PubMed n.d. https://pubmed.ncbi.nlm.nih.gov/22825113/. Accessed 23 Nov 2021
Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM (2006) SD: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol 195:657–672. https://doi.org/10.1016/j.ajog.2005.09.007
McFarland MB, Langer O, Piper JM, Berkus MD (1996) Perinatal outcome and the type and number of maneuvers in SD. Int J Gynecol Obstet 55:219–224. https://doi.org/10.1016/S0020-7292(96)02766-X
Hoffman MK, Bailit JL, Branch DW, Burkman RT, Van Veldhusien P, Lu L et al (2011) A comparison of obstetric maneuvers for the acute management of SD. Obstet Gynecol 117:1272–1278. https://doi.org/10.1097/AOG.0b013e31821a12c9
Michelotti F, Flatley C, Kumar S (2018) Impact of SD, stratified by type of manoeuvre, on severe neonatal outcome and maternal morbidity. Aust N Z J Obstet Gynaecol 58:298–305. https://doi.org/10.1111/ajo.12718
Hehir MP, Rubeo Z, Flood K, Mardy AH, O’Herlihy C, Boylan PC et al (2018) Anal sphincter injury in vaginal deliveries complicated by SD. Int Urogynecol J 29:377–381. https://doi.org/10.1007/s00192-017-3351-2
Gauthaman N, Walters S, Tribe I-A, Goldsmith L, Doumouchtsis SK (2016) SD and associated manoeuvres as risk factors for perineal trauma. Int Urogynecol J 27:571–577. https://doi.org/10.1007/s00192-015-2863-x
Sagi-Dain L, Sagi S (2015) The role of episiotomy in prevention and management of SD: a systematic review. Obstet Gynecol Surv 70:354–362. https://doi.org/10.1097/OGX.0000000000000179
Paris AE, Greenberg JA, Ecker JL, McElrath TF (2011) Is an episiotomy necessary with a SD? Am J Obstet Gynecol 205(217):e1-3. https://doi.org/10.1016/j.ajog.2011.04.006
Shoulder dystocia (Green-top Guideline No. 42). Royal College of Obstetricians and Gynaecologists https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg42/. Accessed 12 Aug 2021
Gurewitsch ED, Donithan M, Stallings SP, Moore PL, Agarwal S, Allen LM et al (2004) Episiotomy versus FM in managing severe SD: a comparison of outcomes. Am J Obstet Gynecol 191:911–916. https://doi.org/10.1016/j.ajog.2004.06.041
MacKenzie IZ, Shah M, Lean K, Dutton S, Newdick H, Tucker DE (2007) Management of SD: trends in incidence and maternal and neonatal morbidity. Obstet Gynecol 110:1059–1068. https://doi.org/10.1097/01.AOG.0000287615.35425.5c
Nocon JJ, McKenzie DK, Thomas LJ, Hansell RS (1993) SD: an analysis of risks and obstetric maneuvers. Am J Obstet Gynecol 168:1732–1737. https://doi.org/10.1016/0002-9378(93)90684-b (discussion 1737-1739)
Enquête Nationale Périnatale de 2016, http://www.xn--epop-inserm-ebb.fr/wp-content/uploads/2017/11/ENP2016_rapport_complet.pdf. Accessed 29 Oct 2021
Deering SH, Tobler K, Cypher R (2010) Improvement in documentation using an electronic checklist for SD deliveries. Obstet Gynecol 116:63–66. https://doi.org/10.1097/AOG.0b013e3181e42220
Zuckerwise LC, Hustedt MM, Lipkind HS, Funai EF, Raab CA, Pettker CM (2020) Effect of implementing a standardized SD documentation form on quality of delivery notes. J Patient Saf 16:259–263. https://doi.org/10.1097/PTS.0000000000000305
Legendre G, Bouet P-E, Sentilhes L (2015) Place of simulation to reduce neonatal and secondary maternal morbidity to SD. J Gynecology Obstetrics Biol Reprod 44:1285–1293. https://doi.org/10.1016/j.jgyn.2015.09.047
Olson DN, Logan L, Gibson KS (2021) Evaluation of multidisciplinary SD simulation training on knowledge, performance, and documentation. Am J Obstet Gynecol MFM 3:100401. https://doi.org/10.1016/j.ajogmf.2021.100401
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
BD: Data collection, data analysis, manuscript writing. FP: Project development. BG: Project development, data collection, data analysis, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
As our study was observational and did not involve any change in our practices, patients underwent no supplementary procedures. We reported non-identifying data from patient’s medical records. Ethical Committee approval was therefore not required for this study according to the Jardé law. Nevertheless, upon admission in our institution, each patient receives a document stating that personal medical data collected during hospitalization could be used anonymously for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Diack, B., Pierre, F. & Gachon, B. Impact of fetal manipulation on maternal and neonatal severe morbidity during shoulder dystocia management. Arch Gynecol Obstet 307, 501–509 (2023). https://doi.org/10.1007/s00404-022-06783-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06783-y