Abstract
Purpose
Surgical training usually means inexperienced physicians initially doing operations supervised by an experienced physician, to gain the experience and skills needed to conduct surgery independently. Various issues arise here for both hospitals and patients. Are training procedures associated with higher complication rates, blood losses, and transfusion rates? What does training in the operating room ultimately cost in terms of valuable surgical time? Do longer hospitalization periods potentially mean financial losses for the hospital under the diagnosis-related groups (DRG) system?
Methods
A retrospective analysis was carried out of data for 571 patients who underwent total laparoscopic hysterectomy (TLH) in the Department of Gynecology at the University of Erlangen from 2009 to 2012, with/without adnexectomy, due to benign indication; and of data for 255 patients who underwent the same procedures in Karlsruhe Municipal Hospital in 2013–2014. The patients were classified into two groups: those in whom surgery was carried out by experienced specialists who had carried out at least 40 independent operations; and those in whom it was carried out by a trainee resident who had personally done fewer than 40 operations.
Results
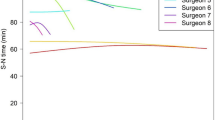
In the two groups, the patients had similar mean body mass indexes, uterus weights, and blood losses. Patients in the specialist group were slightly older. There were no differences in complication rates. Over two-thirds of complications occurred in patients with previous surgery. Procedures by residents took significantly longer. Hospitalization periods in both groups were still below the mean threshold length of stay under Germany’s DRG system, so that no income losses occurred even with training procedures.
Conclusions
Training and teaching operations supervised by experienced surgeons are just as safe as operations by experienced surgeons themselves. Interpretation of these data is of course limited by the retrospective study design; patients treated by specialists tended to have more prior operations and were older, with a trend toward larger uteri. Surgical training, as the example of TLH in benign indication shows here, involves an additional time of approximately 10–20 min per operation. With regard to the revenue situation, the hospitalization periods in both groups were within the profit zone for the hospital concerned.
Similar content being viewed by others
References
Landesärztekammer B (2012) Weiterbildungsordnung für die Ärzte Bayerns vom 24.04.2004 i. d. F. d. Beschlüsse vom 16.10.2011 Richtlinien über den Inhalt der Weiterbildung i. d. F. vom 21.04.2012
Prutz F, Knopf H, von der Lippe E, Scheidt-Nave C, Starker A, Fuchs J (2013) Prevalence of hysterectomy in women 18 to 79 years old: results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 56(5–6):716–722. https://doi.org/10.1007/s00103-012-1660-7
Neis KJ, Zubke W, Romer T, Schwerdtfeger K, Schollmeyer T, Rimbach S, Holthaus B, Solomayer E, Bojahr B, Neis F, Reisenauer C, Gabriel B, Dieterich H, Runnenbaum IB, Kleine W, Strauss A, Menton M, Mylonas I, David M, Horn LC, Schmidt D, Gass P, Teichmann AT, Brandner P, Stummvoll W, Kuhn A, Muller M, Fehr M, Tamussino K (2016) Indications and route of hysterectomy for benign diseases. Guideline of the DGGG, OEGGG and SGGG (S3 Level, AWMF Registry No. 015/070, April 2015). Geburtshilfe Frauenheilkd 76(4):350–364. https://doi.org/10.1055/s-0042-104288
Balayla J, Abenhaim HA, Martin MC (2012) Does residency training improve cognitive competence in obstetric and gynaecologic surgery? J Obstet Gynaecol Can 34(2):190–196
Curran D, Xu X, Dewald S, Johnson TR, Reynolds RK (2012) An alumni survey as a needs assessment for curriculum improvement in obstetrics and gynecology. J Grad Med Educ 4(3):317–321. https://doi.org/10.4300/jgme-d-11-00122.1
Leung Y, Salfinger S, Mercer A (2015) The positive impact of structured teaching in the operating room. Aust N Z J Obstet Gynaecol 55(6):601–605. https://doi.org/10.1111/ajo.12392
Chen CC, Green IC, Colbert-Getz JM, Steele K, Chou B, Lawson SM, Andersen DK, Satin AJ (2013) Warm-up on a simulator improves residents’ performance in laparoscopic surgery: a randomized trial. Int Urogynecol J 24(10):1615–1622. https://doi.org/10.1007/s00192-013-2066-2
Levine RL, Kives S, Cathey G, Blinchevsky A, Acland R, Thompson C, Pasic R (2006) The use of lightly embalmed (fresh tissue) cadavers for resident laparoscopic training. J Minim Invasive Gynecol 13(5):451–456. https://doi.org/10.1016/j.jmig.2006.06.011
Jokinen E, Brummer T, Jalkanen J, Fraser J, Heikkinen AM, Makinen J, Sjoberg J, Tomas E, Mikkola TS, Harkki P (2015) Hysterectomies in Finland in 1990–2012: comparison of outcomes between trainees and specialists. Acta Obstet Gynecol Scand 94(7):701–707. https://doi.org/10.1111/aogs.12654
Kreiker GL, Bertoldi A, Larcher JS, Orrico GR, Chapron C (2004) Prospective evaluation of the learning curve of laparoscopic-assisted vaginal hysterectomy in a university hospital. J Am Assoc Gynecol Laparosc 11(2):229–235
Kroft J, Moody JR, Lee P (2011) Canadian hysterectomy educational experience: survey of recent graduates in obstetrics and gynecology. J Minim Invasive Gynecol 18(4):438–444. https://doi.org/10.1016/j.jmig.2011.03.004
Fiori W, Renner SP, Siam K, Babapirali J, Roeder N, Dausch E, Hildebrandt T, Hillemanns P, Nehmzow M, Zygmunt M, Piroth D, Schem C, Schwenzer T, Friese K, Wallwiener D, Beckmann W (2013) Shaping the system—the DRG evaluation project of the German Society for Gynaecology and Obstetrics (Deutsche Gesellschaft fur Gynakologie und Geburtshilfe, DGGG). Geburtshilfe und Frauenheilkunde. https://doi.org/10.1055/s-0033-1350748
Bonilla DJ, Mains L, Whitaker R, Crawford B, Finan M, Magnus M (2007) Uterine weight as a predictor of morbidity after a benign abdominal and total laparoscopic hysterectomy. J Reprod Med 52(6):490–498
Fiaccavento A, Landi S, Barbieri F, Zaccoletti R, Tricolore C, Ceccaroni M, Pomini P, Bruni F, Soriano D, Stepniewska A, Selvaggi L, Zanolla L, Minelli L (2007) Total laparoscopic hysterectomy in cases of very large uteri: a retrospective comparative study. J Minim Invasive Gynecol 14(5):559–563. https://doi.org/10.1016/j.jmig.2007.04.013
O’Hanlan KA, Dibble SL, Fisher DT (2006) Total laparoscopic hysterectomy for uterine pathology: impact of body mass index on outcomes. Gynecol Oncol 103(3):938–941. https://doi.org/10.1016/j.ygyno.2006.05.036
Heinberg EM, Crawford BL 3rd, Weitzen SH, Bonilla DJ (2004) Total laparoscopic hysterectomy in obese versus nonobese patients. Obstet Gynecol 103(4):674–680. https://doi.org/10.1097/01.aog.0000119224.68677.72
Obermair A, Manolitsas TP, Leung Y, Hammond IG, McCartney AJ (2005) Total laparoscopic hysterectomy versus total abdominal hysterectomy for obese women with endometrial cancer. Int J Gynecol Cancer 15(2):319–324. https://doi.org/10.1111/j.1525-1438.2005.15223.x
Becker S, Hirsch HA, Käser O, Iklé FA, Schmidt EH, De Wilde RL, Abele H, Bachmann C, Brucker S, Fehm T, Gardanis K, Grischke EM, Goerner R, Hahn M, Hoffmann J, Hornung R, Krainick-Strobel U, Krämer B, Reisenauer C, Röhm C, Solomayer E, Zubke W (2009) Atlas der gynäkologischen Operationen. 7., vollständig überarbeitete und erweiterte Auflage edn. Georg Thieme Verlag, Stuttgart. https://doi.org/10.1055/b-002-46977
Igwe E, Hernandez E, Rose S, Uppal S (2014) Resident participation in laparoscopic hysterectomy: impact of trainee involvement on operative times and surgical outcomes. Am J Obstet Gynecol 211(5):484.e481–484.e487. https://doi.org/10.1016/j.ajog.2014.06.024
Muller A, Thiel FC, Renner SP, Winkler M, Haberle L, Beckmann MW (2010) Hysterectomy-a comparison of approaches. Deutsches Arzteblatt international 107(20):353–359. https://doi.org/10.3238/arztebl.2010.0353
Advani V, Ahad S, Gonczy C, Markwell S, Hassan I (2012) Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg 203(3):347–351. https://doi.org/10.1016/j.amjsurg.2011.08.015 (discussion 351-342)
Akingba DH, Deniseiko-Sanses TV, Melick CF, Ellerkmann RM, Matsuo K (2008) Outcomes of hysterectomies performed by supervised residents vs those performed by attendings alone. American journal of obstetrics and gynecology 199(6):673.e671–673.e676. https://doi.org/10.1016/j.ajog.2008.07.052
Coates KW, Kuehl TJ, Bachofen CG, Shull BL (2001) Analysis of surgical complications and patient outcomes in a residency training program. American journal of obstetrics and gynecology 184(7):1380–1383 (discussion 1383–1385)
Shaked A, Calderom I, Durst A (1991) Safety of surgical procedures performed by residents. Arch Surg (Chicago, Ill: 1960) 126(5):559–560
Bridges M, Diamond DL (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 177(1):28–32
Author information
Authors and Affiliations
Contributions
TH: data collection or management, data analysis, manuscript, writing/editing. SE: data collection or management. AB: data collection or management. MWB: supervising/proof reading. AM: project development, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the survey involving human participants were in accordance with the ethical standards of institutional and national research committee (Ethic Committee of Friedrich Alexander University of Erlangen-Nuremberg). The study does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hildebrandt, T., Emir, S., Boosz, A. et al. Total laparoscopic hysterectomy: how does training for surgeons in a standardized operation affect hospitals and patients?. Arch Gynecol Obstet 298, 763–771 (2018). https://doi.org/10.1007/s00404-018-4869-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4869-3