Abstract
Purpose
Vaginal microecological environment is an important factor of recurrent vulvovaginal candidiasis (RVVC). This study was undertaken to investigate dynamic changes of vaginal microecosystem in patients with RVVC.
Methods
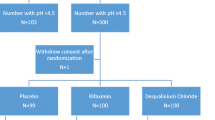
Four hundred patients with VVC and 400 healthy women of reproductive age who admitted to the hospital from January 2012 to December 2013 were evaluated retrospectively. Vaginal microecological factors were evaluated before and after treatment until no recurrence, including vaginal cleanliness, white blood cells, Lactobacillus, Lactobacillus classification, bacteria density, flora diversity, Nugent scores, etc. The grouping was done according to the recurrence of the disease. Every time after treatment, the relapsing patients were defined as case group and the cured patients without recurrence were defined as control group. The differences in the results between the case and the control groups were analyzed by t test.
Results
With the development of RVVC, the ages of all case groups were lower than the corresponding control groups. In different stages of the disease, the bacteria density of the case groups and their corresponding control groups had no significant difference (P > 0.05). Most of the microecological indicators of the first occurring group were significantly different (P < 0.05) from that of the control group. In the recurrence groups, only a few indicators were significantly different from the control groups. The values of all vaginal microecological indicators (except Lactobacillus) of all case groups were higher than that of the control groups. The values of Lactobacillus of all RVVC case groups were lower than that of the RVVC control groups.
Conclusions
There were vaginal microecological imbalances in all developing stages of RVVC. As for vaginal flora, diverse sorts changed to normal Lactobacillus dominantly with the development of RVVC. In the first occurrence of RVVC, after antifungal treatment, Lactobacillus is suggested to be timely supplemented to restore vaginal microecological balance.



Similar content being viewed by others
Abbreviations
- BV:
-
Bacterial vaginosis
- RVVC:
-
Recurrent vulvovaginal candidiasis
- VVC:
-
Vulvovaginal candidiasis
- OML:
-
Oil immersion lens
- HPL:
-
High-power lens
- H2O2 :
-
Hydrogen peroxide
- WBC:
-
White blood cells
- WCSUH:
-
West China Second University Hospital
References
Buchta V, Spaček J (2011) Pitfalls of the current laboratory diagnosis and treatment of vulvovaginal candidiasis. Klin Mikrobiol Infekc Lek 17:158–163
Sobel JD, Wiesenfeld HC, Martens M, Danna P, Hooton TM, Rompalo A et al (2004) Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. N Engl J Med 351:876–883
Barousse MM, Espinosa T, Dunlap K, Fidel PL (2005) Vaginal epithelial cell anti-Candida albicans activity is associated with protection against symptomatic vaginal candidiasis. Infect Immun 73:7765–7767
Fidel PL (2007) History and update on host defense against vaginal candidiasis. Am J Reprod Immunol 57:2–12
Raška M, Běláková J, Křupka M, Weigl E (2007) Candidiasis—do we need to fight or to tolerate the Candida fungus? Folia Microbiol (Praha) 52:297–312
Santoni G, Boccanera M, Adriani D, Lucciarini R, Amantini C, Morrone S et al (2002) Immune cell-mediated protection against vaginal candidiasis: evidence for a major role of vaginal CD4+ T cells and possible participation of other local lymphocyte effectors. Infect Immun 70:4791–4797
Liu Z, Wang X, Liao Q (2009) Investigate the pathogen flora and the treatment of recurrent vulvovaginal candidiasis. J Pract Obstet Gynecol 12:013
Rosa MI, Silva BR, Pires PS, Silva FR, Silva NC, Souza SL et al (2013) Weekly fluconazole therapy for recurrent vulvovaginal candidiasis: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 167:132–136
Richter SS, Galask RP, Messer SA, Hollis RJ, Diekema DJ, Pfaller MA (2005) Antifungal susceptibilities of Candida species causing vulvovaginitis and epidemiology of recurrent cases. J Clin Microbiol 43:2155–2162
Donders G (1999) Microscopy of the bacterial flora on fresh vaginal smears. Infect Dis Obstet Gynecol 7:177
Kovachev S (2010) Vaginal ecosystem. Akush Ginekol (Sofiia) 50:41–49
Borges S, Silva J, Teixeira P (2014) The role of Lactobacilli and probiotics in maintaining vaginal health. Arch Gynecol Obstet 289:479–489
Mikić AN, Stojic S (2015) Study results on the use of different therapies for the treatment of vaginitis in hospitalised pregnant women. Arch Gynecol Obstet. doi:10.1007/s00404-015-3638-9
Kovachev SM, Vatcheva-Dobrevska RS (2015) Local probiotic therapy for vaginal Candida albicans infections. Probiotics Antimicrob Proteins 7:38–44
Osset J, Garcia E, Bartolome R, Andreu A (2001) Role of Lactobacillus as protector against vaginal candidiasis. Med Clin (Barc) 117:285–288
Myziuk L, Romanowski B, Johnson SC (2003) BVBlue test for diagnosis of bacterial vaginosis. J Clin Microbiol 41:1925–1928
Nugent RP, Krohn MA, Hillier S (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol 29:297–301
Ünlü C, Donders G (2011) Use of Lactobacilli and estriol combination in the treatment of disturbed vaginal ecosystem: a review. J Turk Ger Gynecol Assoc 12:239
Fan S, Liao Q, Liu X, Liu Z, Zhang D (2008) Vaginal allergic response in women with vulvovaginal candidiasis. Int J Gynecol Obstet 101:27–30
Egan ME, Lipsky MS (2000) Diagnosis of vaginitis. Am Fam Physician 62:1095–1104
Falagas ME, Betsi GI, Athanasiou S (2006) Probiotics for prevention of recurrent vulvovaginal candidiasis: a review. J Antimicrob Chemother 58:266–272
Acknowledgments
The authors would like to thank the staffs of the Department of Laboratory Medicine and the doctors of the outpatient department of Obstetrics and Gynecology at the West China Second University Hospital, Sichuan University, China. This work was funded by the Support Program of Science and Technology Department of Sichuan Province, China (2013SZ0037).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
X. Yue and P. Chen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yue, Xa., Chen, P., Tang, Y. et al. The dynamic changes of vaginal microecosystem in patients with recurrent vulvovaginal candidiasis: a retrospective study of 800 patients. Arch Gynecol Obstet 292, 1285–1294 (2015). https://doi.org/10.1007/s00404-015-3774-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3774-2