Abstract
Background
Chorioamnionitis (CAM) is a common risk factor for preterm births, resulting in several adverse outcomes. The association between infertility treatment and CAM is unclear. Therefore, this study examined the association between infertility treatment and CAM and described subsequent neonatal outcomes.
Methods
This population-based cohort study used data from the National Vital Statistics System Database. We included women who had a singleton live birth from January 1, 2016 to December 31, 2018. Women-infant pairs were stratified by infertility treatment, and the main outcome was a reported diagnosis of CAM in a checkbox format: clinical CAM or maternal temperature of > 38 °C. Multivariate logistic regression was used to examine the association between infertility treatment and CAM and the effect of infertility treatment on neonatal outcomes in women diagnosed with CAM.
Results
The final sample comprised 10,900,495 woman-infant pairs, and 1.4% received infertility treatment. Compared with the natural conception group, women receiving infertility treatment had a significantly higher risk of CAM (adjusted odds ratio [aOR] 1.772 [95% confidence interval {CI}, 1.718–1.827]). Furthermore, newborns exposed to CAM had a higher risk of very low birth weight (VLBW) (aOR, 2.083 [95% CI, 1.664–2.606], P < .001), preterm birth (aOR, 1.497 [95% CI, 1.324–1.693]; P < .001), neonatal intensive care unit admission (aOR, 1.234 [95% CI, 1.156–1.317]; P < .001), and other adverse neonatal outcomes in the infertility treatment group compared with ones conceived naturally.
Conclusions
This study found that women who received infertility treatment had a higher risk of CAM. And CAM deteriorated neonatal outcomes in the infertility treatment group.
Similar content being viewed by others
Introduction
As of 2020, 10.09% of all births in the United States were premature [1], resulting in 75% perinatal mortality and half long-term morbidity [2]. In addition, 40–70% of premature births are induced by chorioamnionitis (CAM), particularly in early gestation [3, 4]. Acute CAM or intra-uterine inflammation indicates that a pregnant woman is exposed to inflammatory or infectious disorders of the chorion or amnion. Either of these conditions could lead to an increased risk of developing serious complications [5] such as sepsis [6], cerebral palsy [7], and bronchopulmonary dysplasia in the mother-infant pair [8].
Infertility is defined as 1 year of unwanted non-conception with unprotected intercourse in the fertile phase of menstrual cycles [9] and affects 8–12% of the population worldwide [10]. Consequently, assisted reproductive technology (ART) has become widespread since the early 1980s; this technology includes in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) [11]. Non-ART treatments, consisting of fertility medications, artificial insemination, and intrauterine insemination, result in 4.6% of United States (US) births, which is four times greater than the contribution of ART [12]. Despite great progress, newborns after IVF/ICSI have more compromised perinatal outcomes than spontaneously conceived newborns [13], such as preterm birth [14] and defects in neurodevelopmental health [15] and cardiovascular function and metabolism [16].
Moreover, ART is associated with an abnormal condition in the mother-infant surface modulated by the placenta, which might contribute to a hyper/hyporeactive status to infection or other inflammations [17]. CAM has been demonstrated to have an infection/inflammation status before delivery; however, the association between infertility treatment and CAM has not been clarified. One study found that women with mixed infertility who conceived by IVF had a higher risk of CAM among singleton pregnancies than those who conceived spontaneously [18]. However, few studies have considered the maternal infection status during pregnancy when evaluating the relationship between infertility treatment and CAM. Additionally, further studies are necessary to determine if infertility treatment deteriorates CAM-related neonatal outcomes.
In this study, we explored US birth certificate data to examine the association between infertility treatment and CAM and the subsequent neonatal outcomes in the population with CAM. This can provide information to obstetricians and neonatologists when evaluating women and infants receiving infertility treatment.
Methods
Study population
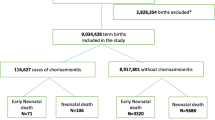
In this prospective, population-based cohort study, we explored the National Vital Statistics System database and collected birth and death records submitted by 50 states and the District of Columbia to the Centers for Disease Control (CDC). This study included 1,162,440 mothers in the database with live births from January 1, 2016 to December 31, 2018. After excluding 10,310 missing obstetric complications records, 396,031 with twins or multiple births, 208,169 with pre-pregnancy hypertension, 84,622 with diabetes, and 33,056 with incomplete medical records, a total of 10,900,495 mother-infant pairs were finally recruited. According to the International Peace Maternal and Child Hospital Institutional Review Board, this study was exempt from the requirement for informed consent because the data used were publicly available. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Exposure and outcomes
The main outcome was a diagnosis of CAM during the present pregnancy after infertility treatment, which was identified in a checkbox format: clinical CAM or maternal temperature > 38 °C.
We included several neonatal outcomes including sex, gestational age, birth weight, neonatal intensive care unit (NICU) admission, assisted ventilation, assisted ventilation > 6 h, and surfactant or antibiotic use. Neonatal sex was categorized as male or female. Gestational age was calculated using obstetric estimation at delivery as preterm (< 37 weeks) and a specified category: extremely (delivery < 28 weeks), very (delivery at 28–31+6 weeks), and moderate and late (delivery at 32–36+6 weeks). Birth weight was classified as normal, low (LBW, 1500 g -2500 g), and very low (VLBW, ≤ 1500 g).
The exposure in this study was infertility treatment, including (1) ART, such as IVF, intrafallopian gamete transfer, and zygote intrafallopian transfer, and (2) non-ART treatment, such as fertility-enhancing drugs, artificial insemination, and intrauterine insemination. Mothers who received both ART and non-ART treatment were classified into the ART group. In the main analysis, both (1) and (2) were considered infertility treatment groups. For the subgroup analysis, (1) and (2) were evaluated separately. Exposure information was obtained directly from the Health and Medical Information section of the US Standard Certificate of Live Births.
Covariates
Baseline variables that were considered clinically relevant or showed a univariate relationship with the outcome were entered into the multivariate logistic regression model (data not shown). Variables for inclusion were carefully chosen to ensure the parsimony of the final model, given the number of events available. Second, candidate variables with P < 0.05 on univariate analysis were included in the multivariable model; however, all baseline variables were significant in the univariable logistic regression model due to the large sample size.
The variables included maternal age, race, ethnicity, educational level, marital status, parity, smoking status before and during pregnancy, history of preterm delivery, history of cesarean delivery, pre-pregnancy body mass index (BMI), timing of initiation of prenatal care, prenatal visit counts, WIC (Supplemental Nutrition Program for Women, Infants, and Children), payment for delivery, gestational hypertension, eclampsia, gestational diabetes, neonatal sex, and infection status.
Maternal age was defined as the age at the time of birth and was classified as < 20, 20–24, 25–29, 30–34, 35–39, or ≥ 40 years. Maternal race and ethnicity were categorized as White, Black, Asian, Native American or Alaska Native, Native Hawaiian or other Pacific Islander, people of more than one race, Hispanic, or unknown or unstated racial or ethnic origin. Maternal educational levels were recorded as 8th grade or lower, 9th–12th grade without a diploma, 9th–12th grade with a diploma, or higher than 12th grade. Marital status was categorized as married or unmarried. Parity, defined as the total number of live births excluding the current delivery, was classified as zero, one, two, three–seven, and eight or more. Smoking status before and during pregnancy was classified as “yes” or “no.” The time of prenatal care initiation was categorized according to the trimester of the first prenatal visit as no prenatal care, first trimester, second trimester, or third trimester. Maternal pre-pregnancy BMI was classified as < 18.5, 18.5– 24.9, 25.0– 29.9, 30.0– 34.9, 35.0– 39.9, or ≥ 40 kg/m2. Other risk factors during pregnancy were directly collected from the facility worksheet of the US Standard Certificate of Live Births. Four options for the source of payment at delivery were identified in a checkbox format: 1) private insurance, 2) Medicaid, 3) self-pay, and 4) other (must be specified). Gestational diabetes, gestational hypertension, eclampsia, and history of preterm delivery were classified as “yes” or “no.” These maternal variables were identified from the facility worksheet of the US Standard Certificate of Live Birth (https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks), and diagnostic criteria were documented in the worksheet. When necessary, a missing category for the covariates was added.
Statistical analysis
Continuous variables are expressed as means and standard deviations, and categorical variables are expressed as frequencies and percentages. A χ2 test was used to analyze categorical variables, and an unpaired two-tailed t-test or Mann–Whitney U test was used for numerical variables.
In the main analyses, we estimated the association between infertility treatment (ART and non-ART groups separately in the subgroup analysis) and CAM; the natural conception group was used as the reference. Model 1 presents the univariate analysis. Model 2 was adjusted for sociodemographic characteristics, including maternal age, race and ethnicity, educational level, marital status, parity, smoking status before and during pregnancy, history of preterm delivery, history of cesarean delivery, pre-pregnancy BMI, timing of initiation of prenatal care, prenatal visit counts, gestational hypertension, gestational diabetes, eclampsia, neonatal sex, WIC, and payment method. Model 3 included the adjustments for model 2 and was further adjusted for the infection status during pregnancy. All results are presented as odds ratios (OR) and 95% confidence intervals (CI). Several studies have found that CAM is closely related to poor neonatal outcomes, including premature rupture of membranes, preterm birth, and LBW [19]; therefore, we further investigated the effect of infertility treatment on neonatal outcomes in women diagnosed with CAM. Multivariate logistic regression analysis, which was adjusted for the same covariates, was performed to evaluate the association between infertility treatment and neonatal outcomes in women diagnosed with CAM.
Statistical analyses were performed using R, version 4.0.1. All P-values were two-tailed, and P < 0. 05 was considered statistically significant.
Results
The final sample comprised 10,900,495 mothers with singleton live births (Fig. 1). A comparison of the present sample and the excluded individuals is shown in Table S1. Of these women, 151,008 (1.4%) received infertility treatment (Table 1). Compared with the natural conception group, the infertility treatment group tended to be older (34.4 ± 5.3 vs. 28.7 ± 5.8 years), Caucasian (72.4 vs. 51.4%), married (85.9 vs. 54.7%), primipara (42.2 vs. 31.4%), and have a college diploma or higher (90.1 vs. 59.8%). Pre-pregnancy BMI and weight gain during pregnancy were comparable between the two groups. Women receiving infertility treatment tended to take early (1st trimester prenatal care: 88.3 vs. 75.0%) and regular prenatal care visits (prenatal visit count ≥ 16: 10.1 vs. 5.7%) and were more likely to have gestational hypertension (10.1 vs. 6.3%), gestational diabetes (10.3 vs. 6.1%), and CAM (3.0 vs. 1.6%).
The association between infertility treatment and CAM risk is presented in Table 2. At the population level, crude analyses suggested that women receiving infertility treatment had a higher risk of developing CAM (OR, 1.954 [95% CI, 1.896–2.013]; P < 0.001). After adjustment for inclusion year, maternal age, race, ethnicity, and socioeconomic and obstetric covariates (model 2), the odds of CAM were 70% higher in the infertility treatment group than in the natural conception group (adjusted OR [aOR], 1.700 [95% CI, 1.664–1.737]; P < 0.001). Model 3 was further adjusted for infection status during pregnancy, and the trend remained (adjusted odds ratio [aOR], 1.772; 95% CI, 1.718–1.827). We further divided infertility treatment into two groups: (1) ART, such as IVF, and (2) non-ART treatment, such as fertility-enhancing drugs. Mothers who received both ART and non-ART treatment were classified into the ART group. Consistent with the main analysis, the ART (aOR, 1.881 [95% CI, 1.810–1.955]; P < 0.001) and non-ART groups (aOR, 1.471 [95% CI, 1.394–1.552]; P < 0.001) were both associated with a higher risk of CAM (Table S2).
CAM is known to result in short- and long-term effects in newborns [19]. In our study, women diagnosed with CAM delivered babies with poor outcomes (data not shown). However, it is unclear whether infertility treatment worsens the outcomes of newborns suffering from CAM. Therefore, we investigated whether infertility treatment was correlated with a higher risk of adverse neonatal outcomes in women with CAM. In our study, birth weight was lower in the infertility treatment group (3326 ± 693 (g) vs. 3344 ± 629 (g) (Table 3). Furthermore, VLBW was more frequent in the infertility group (3.6 vs. 2.5%). The prevalence of preterm birth was 7.2% in those with natural conception and 9.0% in those who received infertility treatment. The incidence rates of very preterm (1.6 vs. 1.2%) and extremely preterm births (2.9 vs. 1.8%) were significantly higher in the infertility treatment group than in the natural conception group. Neonates conceived after infertility treatment in women with CAM had a higher incidence of NICU admission (32.5 vs. 30.0%, P < 0.001), assisted ventilation (13.3 vs. 10.8%, P < 0.001), assisted ventilation > 6 h (13.3 vs. 10.8%, P < 0.001), surfactant use (1.7 vs. 1.1%, P < 0.001), and antibiotic use (31.0 vs. 24.0%, P < 0.001).
We further explored the relationship between infertility treatments and neonatal outcomes (Table 4). The risk of VLBW was 108.3% higher in the infertility treatment group than in the natural conception group (aOR, 2.083 [95% CI, 1.665–2.606], P < 0.001). The risk of preterm birth increased by 49.7% in the infertility treatment group (aOR, 1.497 [95% CI, 1.324–1.693]; P < 0.001). The same trend was observed for moderate, late, very, and extremely preterm birth. In addition, fetuses delivered by mothers with CAM had a higher risk of NICU admission (aOR, 1.234 [95% CI, 1.156–1.317]; P < 0.001), assisted ventilation (aOR, 1.340 [95% CI, 1.224–1.467]; P < 0.001), assisted ventilation > 6 h (aOR, 1.603 [95% CI, 1.384–1.856]; P < 0.001), surfactant use (aOR, 1.948 [95% CI, 1.524–2.492]; P < 0.001), and antibiotic use (aOR, 1.496 [95% CI, 1.400–1.593]; P < 0.001). In general, the risk of adverse neonatal outcomes increased in the infertility treatment group with CAM.
Discussion
This nationwide cohort study included almost 11 million pairs of mothers and singleton newborns. We found that women receiving infertility treatment, either ART or non-ART, had significantly greater association with CAM compared with women who underwent natural conception. In addition, newborns delivered by women with CAM in the infertility group had a higher risk of adverse outcomes such as preterm birth, LBW, and NICU admission before discharge from the hospital compared with ones conceived naturally.
In recent decades, infertility has become an emerging common health issue and has attracted considerable attention [20]. Despite the increased availability and usage of fertility treatment worldwide, its potential adverse effects, including CAM, have not been fully explored. Consistent with our results, a retrospective cohort study exploring the pregnancy outcomes of frozen-thawed IVF with classified infertility etiology found that IVF pregnancies were related to a higher rate of CAM (2.93 [1.04–8.26]) than spontaneous pregnancies [18]. Another study evaluating the mediating effects of multiple gestations on pregnancy complications indicated that women who received treatment during pregnancy had a higher risk of CAM in both the direct and mediated pathways [21]. Pregnant women manifested with any combination of fever, maternal or fetal tachycardia, uterine tenderness, foul-smelling amniotic fluid, or an elevated white blood cell count are suspected to have CAM. However, the presence of one (or more) of these signs and symptoms is not always related to the occurrence of intra-uterine inflammation or the histopathologic CAM. A study found 24% patients diagnosed with preterm birth and clinical CAM had no evidence of either intra-amniotic infection or inflammation, and only 34% had positive amniotic fluid cultures. Patients without microbial invasion of the amniotic cavity or intra-amniotic inflammation had lower rates of adverse outcomes than those exposed to the infection or inflammation [22]. Due to the limitations of the database in the current study, clinical CAM was referred to as exposure, which might not be consistent with “golden evidence” from histological results. Imprecise definitions and variable clinical manifestations, as discussed above, are loosely used to label a heterogeneous array of conditions characterized by infection and inflammation or both. Further studies should explore the relationship between histological CAM and infertility treatment in order to provide clinical management for mothers with CAM and their newborns.
CAM is closely related to preterm birth [2]. The risk of preterm birth resulting from IVF/ICSI is known to be significantly greater than that in spontaneously conceived pregnancies, especially in singleton pregnancies [23,24,25]. In our study, we investigated whether infertility treatment worsens neonatal outcomes in women already diagnosed with CAM. Interestingly, infertility treatment increased all adverse neonatal outcomes, indicating a synergistic effect between the two exposures. Heterogeneous infertility factors such as endometriosis, adenomyosis, polycystic ovary syndrome, and uterine fibroids already exist; thus, inflammatory pathways, hormonal aberrations, decidual senescence, and vascular abnormalities that may impair pregnancy success might increase the adverse effect of infertility treatment. Except for preterm birth, patients with preterm premature rupture of membranes (PPROM) are apt to develop CAM during expectant management [26]; however, the relationship between ART and PPROM was inconsistent. A study found that IVF/ICSI pregnancies were associated with a decreased risk of PPROM (aOR, 0.64; 95% CI 0.42–0.99) [27]; meanwhile, a meta-analysis suggested no differences in the risk of PPROM among women after fresh embryo transplantation and those undergoing natural conception (Risk Ratio 0.92, 95% CI 0.72–1.18; I2 = 0%) [28]. The reason for this remains unclear, and the database did not include PPROM diagnoses.
The potential mechanisms underlying the association between infertility treatments and CAM remain unclear. Despite demonstrable microorganisms, CAM can occur as “sterile” intra-amniotic inflammation under conditions of cellular stress, injury, or death [29] and is induced by environmental pollutants [30], cigarette smoke [31], and ART. A Previous study has shown that ART is linked to dysregulated inflammation and oxidative stress in an assisted reproductive mouse model [32]. Specifically, greater levels of apoptosis and degraded nucleotides, accompanied by higher interleukin (IL)-6 concentrations, were observed in ART placentas, indicating inflammatory status and cellular stress. Placentas from mouse pregnancies achieved by ART also had lower activity of antioxidant enzymes such as superoxide dismutase, glutathione-S-transferase, and xanthine oxidase, which are more severe in pregnancies fertilized using ICSI [33]. Another proposed mechanism is that ART can influence the period around conception when widespread epigenetic changes occur [34]. Furthermore, steroid diffusion/flow from the mother to the fetus is altered in murine pregnancies conceived by ART [33], which may affect trophoblast function in early pregnancy during implantation and placentation. Further research on the potential biological mechanisms underlying CAM resulting from infertility treatment is necessary.
A consequence of ART is a progressive rise in the incidence of twin, triplet, and multiple pregnancies. To avoid potential bias, this study focused on singleton pregnancies. Several studies have reported that ART-induced pregnancies, whether singleton or multiple, have an increased risk of preterm birth and LBW compared with pregnancies that conceived naturally [35], which can also result from CAM. In this study, we found that newborns delivered by women with CAM who received infertility treatment had a higher risk of preterm birth, VLBW, NICU admission, and other supportive treatments. This suggests that infertility treatment could lead to adverse perinatal outcomes apart from CAM. A recent study found that cytokine levels, such as IL-1β, IL-6, and IL-8, were increased in natural conception pregnancies complicated by CAM. Conversely, interferon-γ and tumor necrosis factor-α were decreased in ART [17], which might explain the more inflexible status related to adverse neonatal outcomes in newborns exposed to both infertility treatment and CAM.
Strengths and limitations
This study has several strengths. This study analyzed a nationwide population of mother-newborn pairs, providing sufficient statistical power to examine the association between maternal infertility treatment and CAM. Furthermore, abundant data allowed us to include most confounding factors, such as infection status during pregnancy, to validate our results. However, this study had several limitations. First, the study did not consider the etiology of infertility diagnoses, such as ovulation disorder, tubal disease, endometriosis, male infertility, or mixed infertility (i.e., multiple infertility-related diagnoses). Second, although we adjusted for many maternal characteristics and complicated pregnancy conditions to mitigate confounding factors, we used administrative data, and thus could not guarantee complete and accurate data collection.
Conclusions
Our study results indicate that women receiving infertility treatment were associated with a higher risk of CAM than women who conceived naturally. Furthermore, newborns exposed to CAM in the infertility treatment group were at an increased risk of preterm birth, VLBW, and NICU admission compared with ones conceived naturally. Further investigations are warranted to elucidate the mechanisms underlying the association between infertility treatment and risk of CAM.
Availability of data and materials
Public-use data can be downloaded from the NVSS website (https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm).
Abbreviations
- CAM:
-
Chorioamnionitis
- OR:
-
Odds ratio
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- NICU:
-
Neonatal intensive care unit
- ART:
-
Assisted reproductive technology
- IVF:
-
In vitro fertilization
- ICSI:
-
Intracytoplasmic sperm injection
- LBW:
-
Low birth weight
- VLBW:
-
Very low birth weight
- BMI:
-
Body mass index
- PPROM:
-
Preterm premature rupture of membranes
- US:
-
United States
- IL:
-
Interleukin
References
Martin JA, Hamilton BE, Osterman M. Births in the United States, 2020. NCHS Data Brief. 2021;418:1–8.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet (London, England). 2008;371(9606):75–84.
Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med. 2000;342(20):1500–7.
Yoon BH, Romero R, Lim JH, Shim SS, Hong JS, Shim JY, Jun JK. The clinical significance of detecting Ureaplasma urealyticum by the polymerase chain reaction in the amniotic fluid of patients with preterm labor. Am J Obstet Gynecol. 2003;189(4):919–24.
Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, Silver RM, Raju TNK. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol. 2016;127(3):426–36.
Soraisham AS, Singhal N, McMillan DD, Sauve RS, Lee SK. A multicenter study on the clinical outcome of chorioamnionitis in preterm infants. Am J Obstet Gynecol. 2009;200(4):372.e371-376.
Shatrov JG, Birch SCM, Lam LT, Quinlivan JA, McIntyre S, Mendz GL. Chorioamnionitis and cerebral palsy: a meta-analysis. Obstet Gynecol. 2010;116(2 Pt 1):387–92.
Watterberg KL, Demers LM, Scott SM, Murphy S. Chorioamnionitis and early lung inflammation in infants in whom bronchopulmonary dysplasia develops. Pediatrics. 1996;97(2):210–5.
Evers JL. Female subfertility. Lancet (London, England). 2002;360(9327):151–9.
Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14(6):605–21.
Sunderam S, Kissin DM, Crawford SB, Folger SG, Boulet SL, Warner L, Barfield WD. Assisted reproductive technology surveillance - United States, 2015. MMWR Surveill Summ (Washington, DC: 2002). 2018;67(3):1–28.
Schieve LA, Devine O, Boyle CA, Petrini JR, Warner L. Estimation of the contribution of non-assisted reproductive technology ovulation stimulation fertility treatments to US singleton and multiple births. Am J Epidemiol. 2009;170(11):1396–407.
Berntsen S, Söderström-Anttila V, Wennerholm UB, Laivuori H, Loft A, Oldereid NB, Romundstad LB, Bergh C, Pinborg A. The health of children conceived by ART: ‘the chicken or the egg?’ Hum Reprod Update. 2019;25(2):137–58.
Qin JB, Sheng XQ, Wu D, Gao SY, You YP, Yang TB, Wang H. Worldwide prevalence of adverse pregnancy outcomes among singleton pregnancies after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Arch Gynecol Obstet. 2017;295(2):285–301.
Hart R, Norman RJ. The longer-term health outcomes for children born as a result of IVF treatment. Part II–mental health and development outcomes. Hum Reprod Update. 2013;19(3):244–50.
Guo XY, Liu XM, Jin L, Wang TT, Ullah K, Sheng JZ, Huang HF. Cardiovascular and metabolic profiles of offspring conceived by assisted reproductive technologies: a systematic review and meta-analysis. Fertil Steril. 2017;107(3):622-631.e625.
Price HR, Pang N, Kim H, Coughtrie MWH, Collier AC. Protective placental inflammatory and oxidative stress responses are attenuated in the context of twin pregnancy and chorioamnionitis in assisted reproduction. J Assist Reprod Genet. 2022;39(1):227–38.
Wang J, Liu Q, Deng B, Chen F, Liu X, Cheng J. Pregnancy outcomes of Chinese women undergoing IVF with embryonic cryopreservation as compared to natural conception. BMC Pregnancy Childbirth. 2021;21(1):39.
Jain VG, Willis KA, Jobe A, Ambalavanan N. Chorioamnionitis and neonatal outcomes. Pediatr Res. 2022;91(2):289–96.
Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. 2021;326(1):65–76.
Oberg AS, VanderWeele TJ, Almqvist C, Hernandez-Diaz S. Pregnancy complications following fertility treatment-disentangling the role of multiple gestation. Int J Epidemiol. 2018;47(4):1333–42.
Oh KJ, Kim SM, Hong J-S, Maymon E, Erez O, Panaitescu B, Gomez-Lopez N, Romero R, Yoon BH. Twenty-four percent of patients with clinical chorioamnionitis in preterm gestations have no evidence of either culture-proven intraamniotic infection or intraamniotic inflammation. Am J Obstet Gynecol. 2017;216(6):604.e601-604.e611.
Wang R, Shi Q, Jia B, Zhang W, Zhang H, Shan Y, Qiao L, Chen G, Chen C. Association of preterm singleton birth with fertility treatment in the US. JAMA Netw Open. 2022;5(2):e2147782.
Vannuccini S, Clifton VL, Fraser IS, Taylor HS, Critchley H, Giudice LC, Petraglia F. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum Reprod Update. 2016;22(1):104–15.
Cavoretto P, Candiani M, Giorgione V, Inversetti A, Abu-Saba MM, Tiberio F, Sigismondi C, Farina A. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: meta-analysis of cohort studies. Ultrasound Obstet Gynecol. 2018;51(1):43–53.
Bakar RZ, Köroğlu N, Turkgeldi LS, Tola EN, Cetin BA, Gedikbasi A. Maternal serum procalcitonin levels in prediction of chorioamnionitis in women with preterm premature rupture of membranes. Arch Med Sci. 2021;17(3):694–9.
Lin D, Li P, Fan D, Chen G, Wu S, Ye S, Ma H, Rao J, Zhou Z, Zeng M, et al. Association between IVF/ICSI treatment and preterm birth and major perinatal outcomes among dichorionic-diamnionic twin pregnancies: a seven-year retrospective cohort study. Acta Obstet Gynecol Scand. 2021;100(1):162–9.
Sha T, Yin X, Cheng W, Massey IY. Pregnancy-related complications and perinatal outcomes resulting from transfer of cryopreserved versus fresh embryos in vitro fertilization: a meta-analysis. Fertil Steril. 2018;109(2):330-342.e339.
Romero R, Miranda J, Chaiworapongsa T, Korzeniewski SJ, Chaemsaithong P, Gotsch F, Dong Z, Ahmed AI, Yoon BH, Hassan SS, et al. Prevalence and clinical significance of sterile intra-amniotic inflammation in patients with preterm labor and intact membranes. Am J Reprod Immunol (New York). 2014;72(5):458–74.
Bové H, Bongaerts E, Slenders E, Bijnens EM, Saenen ND, Gyselaers W, Van Eyken P, Plusquin M, Roeffaers MBJ, Ameloot M, et al. Ambient black carbon particles reach the fetal side of human placenta. Nat Commun. 2019;10(1):3866.
Menon R, Fortunato SJ, Yu J, Milne GL, Sanchez S, Drobek CO, Lappas M, Taylor RN. Cigarette smoke induces oxidative stress and apoptosis in normal term fetal membranes. Placenta. 2011;32(4):317–22.
Raunig JM, Yamauchi Y, Ward MA, Collier AC. Assisted reproduction technologies alter steroid delivery to the mouse fetus during pregnancy. J Steroid Biochem Mol Biol. 2011;126(1–2):26–34.
Raunig JM, Yamauchi Y, Ward MA, Collier AC. Placental inflammation and oxidative stress in the mouse model of assisted reproduction. Placenta. 2011;32(11):852–8.
Novakovic B, Lewis S, Halliday J, Kennedy J, Burgner DP, Czajko A, Kim B, Sexton-Oates A, Juonala M, Hammarberg K, et al. Assisted reproductive technologies are associated with limited epigenetic variation at birth that largely resolves by adulthood. Nat Commun. 2019;10(1):3922.
da Silva SG, da Silveira MF, Bertoldi AD, Domingues MR, dos Santos IDS. Maternal and child-health outcomes in pregnancies following Assisted Reproductive Technology (ART): a prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):106.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China Grants (81974232, 82271742), the Clinical Research Plan of SHDC (SHDC2020CR6027, SHDC22022303), the Program of Shanghai Academic Research Leader (21XD1403700), the Interdisciplinary Program of Shanghai Jiao Tong University (YZ2021ZD29) and the Shanghai Municipal Science and Technology Major Project (20Z11900602).
Author information
Authors and Affiliations
Contributions
All the authors who contributed to this work approved the final version of the manuscript. The contributions were as follows: study design: NM, LLJ, LZW; data collection: NM, WT, LBH, YTD; data analyses and interpretation: NM, SQW, LW, DXY, QSD; manuscript drafting: NM, LLJ; and critical revision of the manuscript: LZW, ZQQ, ZJR, NM.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was exempt from ethical approval and informed consent requirements according to the International Peace Maternal and Child Hospital Institutional Review Board, because the data used were publicly available.
Consent for publication
Not applicable.
Competing interests
All authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
The Baseline Comparison Between Included and Excluded Participants. Table S2. Odds Ratios for the Associations Between Infertility Treatment (ART and Non-ART) and Chorioamnionitis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ni, M., Li, L., Zhang, Q. et al. Association of chorioamnionitis with infertility treatment and subsequent neonatal outcomes in the US: a population-based cohort study. BMC Pregnancy Childbirth 23, 369 (2023). https://doi.org/10.1186/s12884-023-05619-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-05619-0