Abstract
Purpose
To identify whether biochemical pregnancy (BP) and spontaneous abortion (SA) cases have the same clinical characteristics in assisted reproductive therapy (ART), and to assess its predictive value for the subsequent cycles.
Methods
Retrospectively reviewed 12,174 cycles in the first in vitro fertilization and embryo transfer (IVF-ET) cycle from January 2009 to December 2012 of Peking University Third Hospital Reproductive Medical Center. Besides those patients who reached ongoing pregnancy stage, 7,598 cases were divided into three groups: group 1, lack of pregnancy (n = 6,651); group 2, BP (n = 520); and group 3, SA (n = 427). We compared the basic status of patients of the three groups, including ages, body mass index, basic hormone levels, controlled ovarian hyperstimulation protocols, amount of gonadotropin use, and endometrium thickness. The reproductive outcome of the next embryo transfer cycles of the three groups was analyzed.
Results
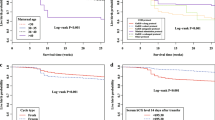
520 patients ended as BP, and 427 patients ended as SA. The age, primary infertility proportion, body mass index, basic FSH level and basic E2 level were similar among groups. Endometrial thickness, controlled ovarian hyperstimulation protocol, Gn dosage, average oocyte retrieval and ET numbers were also similar. Multivariate analysis showed that only the age (P = 0.037, OR 1.060, 95 % CI 1.001–1.120) and endometrium thickness on hCG administration day (P = 0.029, OR 1.136, 95 % CI 1.013–1.275) may result in the differences between BP and SA groups. In the subsequent ET cycles, the total BP rate was 4.37 %, clinical pregnancy rate was 37.28 %, and miscarriage rate was 8.18 %. The clinical pregnancy rates were similar among groups. However, BP group still had the highest BP rate (P < 0.05, 7.97 vs. 4.01 % and 5.28 %), BP and SA group had higher miscarriage rate (P < 0.05, 11.76 % and 14.75 vs. 7.41 %).
Conclusion
BP and SA in first IVF cycles had negative predictive value for subsequent ART outcomes.

Similar content being viewed by others
References
Annan JJ, Gudi A, Bhide P et al (2013) Biochemical pregnancy during assisted conception: a little bit pregnant. J Clin Med Res 5(4):269–274
Taylor T, Eliott G, Wright J et al. (2004) Biochemical pregnancy occur more frequently when transferred embryo quality is diminished on day 3 irrespective to overall embryo quality: the role of positive selection. In: Abstracts of the 20th Annual Meeting of the ESHRE, Berlin, Germany, 27–30 June 2004, O-203
Dor J, Seidman DS, Ben-Shlomo I et al (1996) Cumulative pregnancy rate following in vitro fertilization: the significance of age and infertility aetiology. Hum Reprod 11:425–428
Dickey RP, Olar TT, Taylor SN et al (1993) Relationship of biochemical pregnancy to pre-ovulatory endometrial thickness and pattern in patients undergoing ovulation induction. Hum Reprod 8(2):327–330
Cai QF, Wan F, Huang R et al (2011) Factors predicting the cumulative outcome of IVF/ICSI treatment: a multivariable analysis of 2450 patients. Hum Reprod 26(9):2532–2540
Abdallah RT, Singer T, Huang J et al. (2010) Endometrial polyps smaller than 2 cm increase the risk of biochemical pregnancy in in-vitro fertilization (IVF) cycles. Fertil Steril S243:P-522
Kalu E, Thum MY, Abdalla H (2011) Prognostic value of first IVF cycle on success of a subsequent cycle. J Assist Reprod Genet 28(4):379–382
Bates GW Jr, Ginsburg ES (2002) Early pregnancy loss in in vitro fertilization (IVF) is a positive predictor of subsequent IVF success. Fertil Steril 77(2):337–341
Sneeringer R, Klipstein S, Ryley DA et al (2008) Pregnancy loss in the first in vitro fertilization cycle is not predictive of subsequent delivery in women over 40 years. Fertil Steril 89(2):364–367
Serra VS, Vidal C, Bellver J et al. (2006) Biochemical pregnancy: Clinical significance in assisted reproduction. Fertil Steril S145:P-87
Christiansen OB (2011) Biochemical pregnancies—shall they count in the recurrent miscarriage diagnosis? Symp Abstr/J Reprod Immunol 90(131–163):S45
Sunkara SK, Coomarasamy A, Khalaf Y et al (2007) A three-arm randomised controlled trial comparing Gonadotrophin releasing hormone (GnRH) agonist long regimen versus GnRH agonist short regimen versus GnRH antagonist regimen in women with a history of poor ovarian response undergoing in vitro fertilisation (IVF) treatment: poor responders intervention trial (PRINT). Reprod Health 4:12
Kara M, Aydin T, Aran T et al (2013) Comparison of GnRH agonist and antagonist protocols in normoresponder patients who had IVF-ICSI. Arch Gynecol Obstet 288(6):1413–1416
Troncoso C, Bosch E, Rubio C et al (2003) The origin of biochemical pregnancies: lessons learned from preimplantation genetic diagnosis. Fertil Steril 79(2):449–450
Long W, Yin TL, Zhao QH et al (2011) An analysis of biochemical pregnancy rate and its causes in frozen-thawed embryo transfer cycles (Electronic Edition). Chin J Clin 5(17):5154–5157
Zou L, Peng CL, Ma TZ et al (2014) The analysis on related factors of 53 intrauterine insemination cycles terminated in biochemical pregnancy or clinical pregnancy. Chin J Fam Plan Gynecotokol 6(1):58–60
Yamada H, Morikawa M, Kato EH et al (2003) Pre-conceptional natural killer cell activity and percentage as predictors of biochemical pregnancy and spontaneousabortion with normal chromosome karyotype. Am J Reprod Immunol 50(4):351–354
Fukui A, Kwak-Kim J, Ntrivalas E et al (2008) Intracellular cytokine expression of peripheral blood natural killer cell subsets in women with recurrent spontaneous abortions and implantation failures. Fertil Steril 89(1):157–165
Lin L, Quan S, Chen LN et al (2010) The Effects of oocyte and embryo quality on the occurrence of biochemical pregnancy. Guangdong Med J 31(19):2496–2498
Haas J, Lerner-Geva L, Yerushalmi GM et al (2012) Previous abortion is a positive predictor for ongoing pregnancy in the next cycle in women with repeated IVF failures. Reprod Biomed Online 25(4):339–344
Han LF, Zhang L, Jing WN et al (2006) An analysis of lymphocyte immune therapy on 38 cases of repeated biochemical pregnancy. J Pract Obstet Gynecol 22(5):316–317
Acknowledgments
We appreciate Dr. Lixue Chen for statistic support and Dr. Hai Na for his assistance in revision of the article.
Conflict of interest
The manuscript has been seen and approved by all authors and has no conflicts of interest for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, R., Yang, S., Li, R. et al. Biochemical pregnancy and spontaneous abortion in first IVF cycles are negative predictors for subsequent cycles: an over 10,000 cases cohort study. Arch Gynecol Obstet 292, 453–458 (2015). https://doi.org/10.1007/s00404-015-3639-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3639-8