Abstract
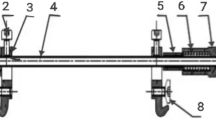
The tension in the skin margin of a wound is the major determinant for wound healing. The difficulty of primary closure for large skin defects due to excessive wound tension has long been a clinical challenge. In this study, we designed and fabricated a reverse-traction skin-stretching device (RT-SSD) to relieve the skin tension of a large skin defect and thereby allow primary wound closure. The novel RT-SSD designed in this study drives the fixing device fixed on the skin edge of the wound by rotating the pulling device, thus exerting a reverse tensile force on both sides of the wound, causing creep and stress relaxation, thus reducing the skin tension. Through the tension analyses; microcirculation detection; clinical scores; and a series of histological staining in vivo, it is verified that intraoperative application of RT-SSD can stretch and straighten collagen and fragment elastin, thus effectively reducing skin tension of large skin defect of miniature pigs. In addition, its special linear and planar traction protects the subcutaneous microcirculation of the wound site. The evaluation of wound healing confirmed that RT-SSD had negligible negative impact on wounds, reduced the incidence of complications, and promoted the healing of large skin defects. Therefore, this study provides a new safe and effective device for the primary closure of large skin defects.







Similar content being viewed by others
References
Hung MH, Liao CT, Kang CJ, Huang SF (2017) Local rhomboid flap reconstruction for skin defects after excising large parotid gland tumors. J Oral Maxillofac Surg. 75(1):225 (e1–e5)
Li Z, Knetsch M (2018) Antibacterial strategies for wound dressing: preventing infection and stimulating healing. Curr Pharm Des 24(8):936–951
Ji X, Li R, Jia WY, Liu GM, Luo YG, Cheng ZQ (2020) Co-axial fibers with janus-structured sheaths by electrospinning release corn peptides for wound healing. ACS Appl Bio Mater 3(9):6430–6438
Kim SW, Choi SH, Kim JT, Kim YH (2015) An additional option for split-thickness skin graft donors: the previous free flap sites. Ann Plast Surg 75(6):634–636
Yan S, Shi H, Chen D, Guo J, Sun Y, Wu S (2018) Repair of large full-thickness scalp defects using biomaterial and skin grafting. J Craniofac Surg 29(4):e426–e429
Lorenzen MM, Gunnarsson GL, Bille C, Tos T, Koudahl V, Rindom MB et al (2019) Visualized bilateral breast reconstruction by propeller thoracodorsal artery perforator flaps. Gland Surg 8:S262–S270
Silva AK, Humphries LS, Maldonado AA, Gottlieb LJ (2019) Chimeric vs composite flaps for mandible reconstruction. Head Neck 41(6):1597–1604
Lee TJ, Oh TS, Kim EK, Suh H, Ahn SH, Son BH et al (2016) Risk factors of mastectomy skin flap necrosis in immediate breast reconstruction using low abdominal flaps. J Plast Surg Hand Surg 50(5):302–306
Song M, Zhang Z, Liu T, Liu S, Li G, Liu Z et al (2017) EASApprox(®) skin-stretching system: a secure and effective method to achieve wound closure. Exp Ther Med 14(1):531–538
Lei Y, Liu L, Du SH, Zong ZW, Zhang LY, Guo QS (2018) The use of a skin-stretching device combined with vacuum sealing drainage for closure of a large skin defect: a case report. J Med Case Rep 12(1):264
Lapid O (2006) An improvised wound closure system. J Trauma 60(4):910–914
Joodaki H, Panzer MB (2018) Skin mechanical properties and modeling: a review. Proc Inst Mech Eng H 232(4):323–343
Ali AK, Abubakar AA, Kaka U, Radzi Z, Khairuddin NH, Yusoff MSM et al (2018) Histological changes of immediate skin expansion of the distal limb of rats. Vet World 11(12):1706–1711
Verhaegen PD, van Trier AJ, Jongen SJ, Vlig M, Nieuwenhuis MK, Middelkoop E et al (2011) Efficacy of skin stretching for burn scar excision: a multicenter randomized controlled trial. Plast Reconstr Surg 127(5):1958–1966
Freeman LJ, Pettit GD, Robinette JD, Lincoln JD, Person MW (1987) Tissue reaction to suture material in the feline linea alba: a retrospective, prospective, and histologic study. Vet Surg. 16(6):440–445
Tapan M, Igde M, Yildirim AR, Yasar B, Ergani HM, Duru C (2018) Reverse thenar perforator flap for large palmar and digital defects. J Hand Surg Am 43(10):956e1–956e6
Ji X, Liu GM, Cui YT, Jia WY, Luo YG, Cheng ZQ (2020) A hybrid system of hydrogel/frog egg-like microspheres accelerates wound healing via sustained delivery ofRCSPs. J Appl Polym Sci 137(46):49521
Zhao Y, Li Z, Song S, Yang K, Liu H, Yang Z et al (2019) Skin-inspired antibacterial conductive hydrogels for epidermal sensors and diabetic foot wound dressings. Adv Funct Mater 29(31):1901474
Lear W, Blattner CM, Mustoe TA, Kruzic JJ (2019) In vivo stress relaxation of human scalp. J Mech Behav Biomed Mater 97:85–89
Hussain SH, Limthongkul B, Humphreys TR (2013) The biomechanical properties of the skin. Dermatol Surg 39(2):193–203
Pamplona DC, Weber HI, Leta FR (2014) Optimization of the use of skin expanders. Skin Res Technol 20(4):463–472
Wood JMB, Soldin M, Shaw TJ, Szarko M (2014) The biomechanical and histological sequelae of common skin banking methods. J Biomech 47(5):1215–1219
Beltran-Frutos E, Ferrer C, Seco-Rovira V, Martinez-Hernandez J, Serrano-Sanchez MI, Pastor LM (2021) Differences in the response in the dermis of the tails of young and old SD rats to treatment with bipolar RF. J Cosmet Dermatol 20(8):2519–2526
Yamawaki Y, Mizutani T, Okano Y, Masaki H (2021) Xanthophyll carotenoids reduce the dysfunction of dermal fibroblasts to reconstruct the dermal matrix damaged by carbonylated proteins. J Oleo Sci 70(5):647–655
Elsner P (2003) What textile engineers should know about the human skin. Curr Probl Dermatol 31:24–34
Derler S, Gerhardt LC (2012) Tribology of skin: review and analysis of experimental results for the friction coefficient of human skin. Tribol Lett 45(1):1–27
Annaidh AN, Bruyere K, Destrade M, Gilchrist MD, Maurini C, Ottenio M et al (2012) Automated estimation of collagen fibre dispersion in the dermis and its contribution to the anisotropic behaviour of skin. Ann Biomed Eng 40(8):1666–1678
Pawlaczyk M, Lelonkiewicz M, Wieczorowski M (2013) Age-dependent biomechanical properties of the skin. Postepy Dermatol Alergol 30(5):302–306
Topaz M, Ashkenazi I, Barzel O, Biswas S, Atar D, Shadmi N et al (2021) Minimizing treatment complexity of combat-related soft tissue injuries using a dedicated tension relief system and negative pressure therapy augmented by high-dose in situ antibiotic therapy and oxygen delivery: a retrospective study. Burns Trauma. https://doi.org/10.1093/burnst/tkab007
Bai HT, Kyu-Cheol N, Wang ZH, Cui YT, Liu H, Liu H et al (2020) Regulation of inflammatory microenvironment using a self-healing hydrogel loaded with BM-MSCs for advanced wound healing in rat diabetic foot ulcers. J Tissue Eng. https://doi.org/10.1177/2041731420947242
Funding
This study was supported by Scientific Development Program of Jilin Province [20200404190YY, 20200404140YY] and Program of Jilin Provincial Health Department [2019SCZT014].
Author information
Authors and Affiliations
Contributions
YC: Conceptualization, Methodology, Investigation, Formal analysis, Writing-original draft, Data curation. BY: Writing-review and editing, Methodology. YZ: Resources, Methodology, Data curation. GR: Data curation, Investigation. MD: Writing—review and editing. CP: Funding acquisition, Writing—review and editing. DW: Conceptualization, Funding acquisition, Writing—review and editing, Supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cui, Y., Yuan, B., Zhang, Y. et al. Reverse-traction skin-stretching device for primary closure of large skin defects. Arch Dermatol Res 315, 751–760 (2023). https://doi.org/10.1007/s00403-022-02408-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-022-02408-1